With Drs. Erez Nossek, Jeremy Liff, and Eytan Raz
The Petrous Apex fistula is a unique thing. It is dural from the standpoint of its supply — its ALL dural — primarily via contributors to its main feeder — the lateral tentorial arcade, or from the multiple potential pial-dural anastomoses (usually via the AICA). However, it is also not a typical dural fistula in that it seems to have a distinct subarachnoid component — the actual arteriovenous connections are usually in the subarachnoid space. It presents with bleeding more often than other dural fistulas, with possible exception of the ethmoid(al) kind — see cases 1 2 and 3. The bleeding is not from the fistula itself — its not like AVM nidus despite its subarachnoid location. Nevertheless, it is also not typical venous infarction type of bleeding that characterizes most brain dural fistulas. It does happen, but what also can bleed here are the brainstem veins draining the fistulas — again similar to the type of cortical venous rupture bleeding that we see with ethmoid fistulas. Finally, it is also unique in the higher than typical incidence of post-embolization hemorrhage. The source of this is not always clear, but frequent pial-dural connections with rupture of the fragile pial vessels have been blamed for it.
Mitsuhashi, Lasjaunias and Co. wrote that this fistula is a homolog of the spinal dural fistulas — and incorporated this into Lasjaunias’ global theory of epidural shunts craniospinal shunts in a classic article. The anatomy is intriguing, while the biologic behavior is not exactly similar. It is good to be pragmatic about it — take this fistula for what it is and know its unique behavior.
The one implication of its anatomy (subarachnoid location of the arteriovenous connections) is that it lends itself to surgical approaches. Those who have been burned by post-embo hemorrhagic issues (ourselves included) usually develop healthy respect for these lesions. Surgery has the advantage of directly controlling those pial-dural anastomoses, but requires thorough understanding of the anatomy and surgical targets.
This one has typical anatomical features, and showcases surgical technique by Dr. Erez Nossek. Presentation is with eye symptoms (this is actually not typical — we will get to that — but regional anatomy is)
MRI — look at the sheet of vessels along the dural edge — these are a gazillion arteries feeding the shunt. It even makes it look like the fistula might be in cavernous sinus
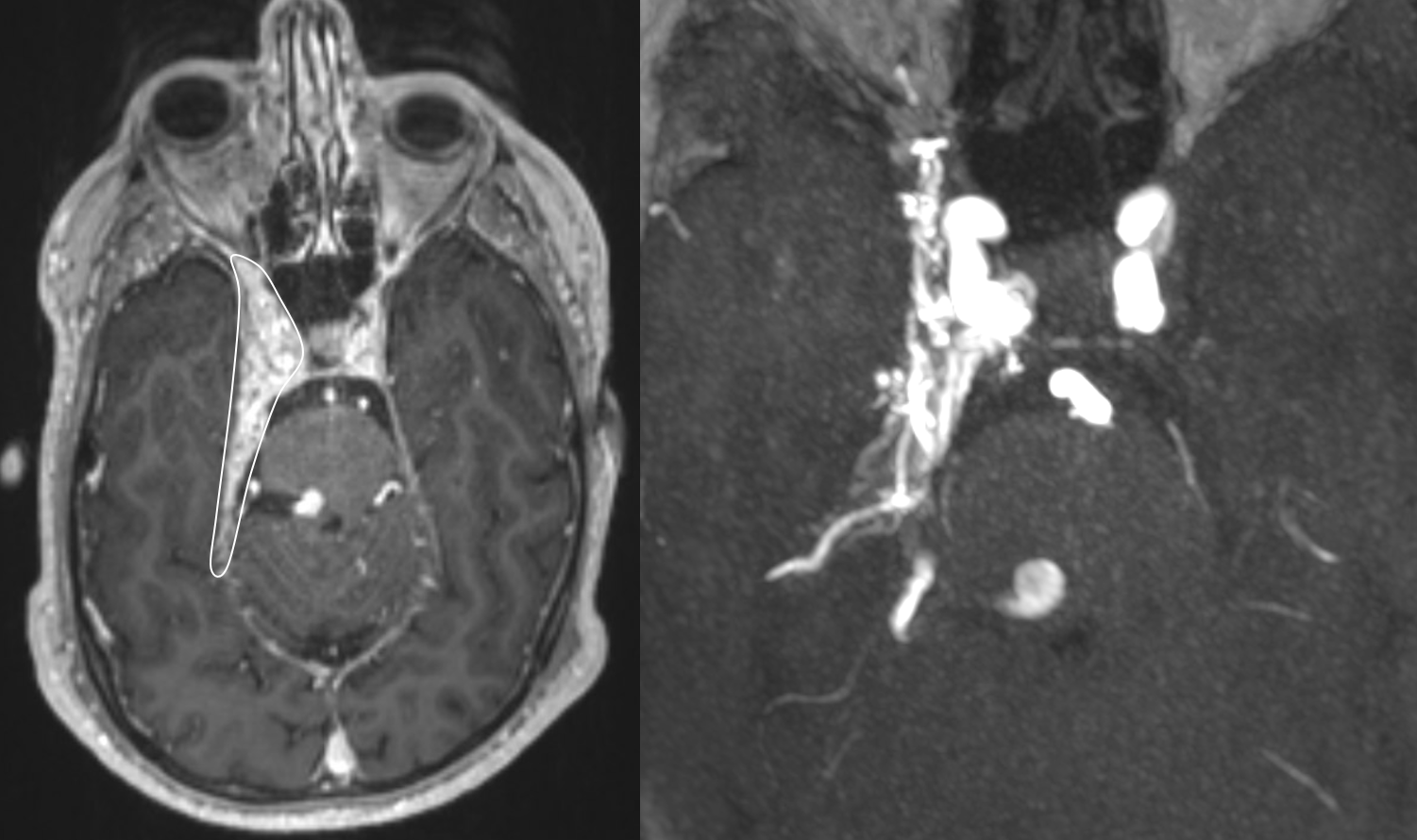
MRI best appreciated with this movie — pause to scroll thru individual frames. Look at enlarged right superior ophthalmic vein — it is important to make sure that there is not a cavernous sinus fistula for example
MRA
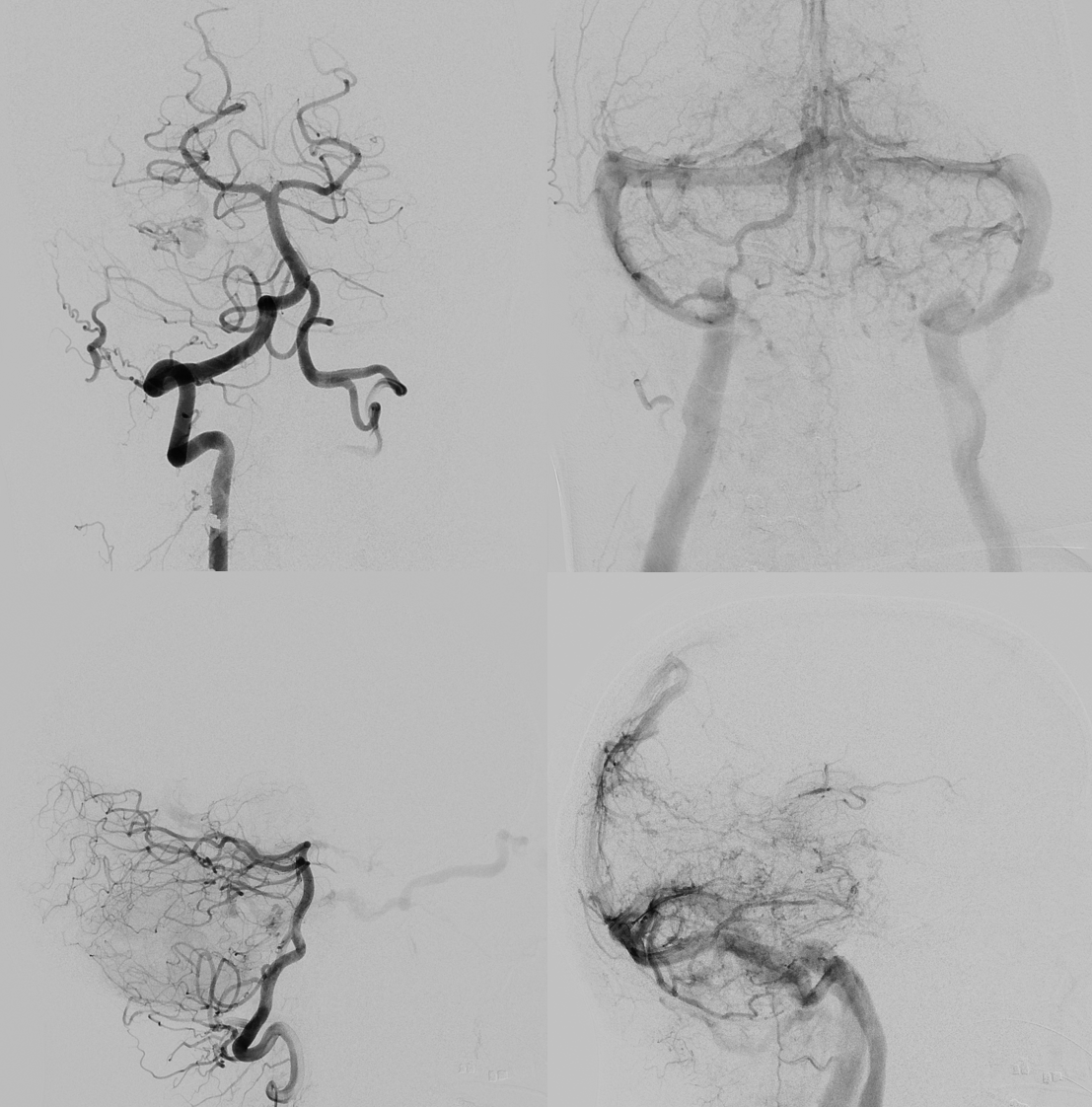
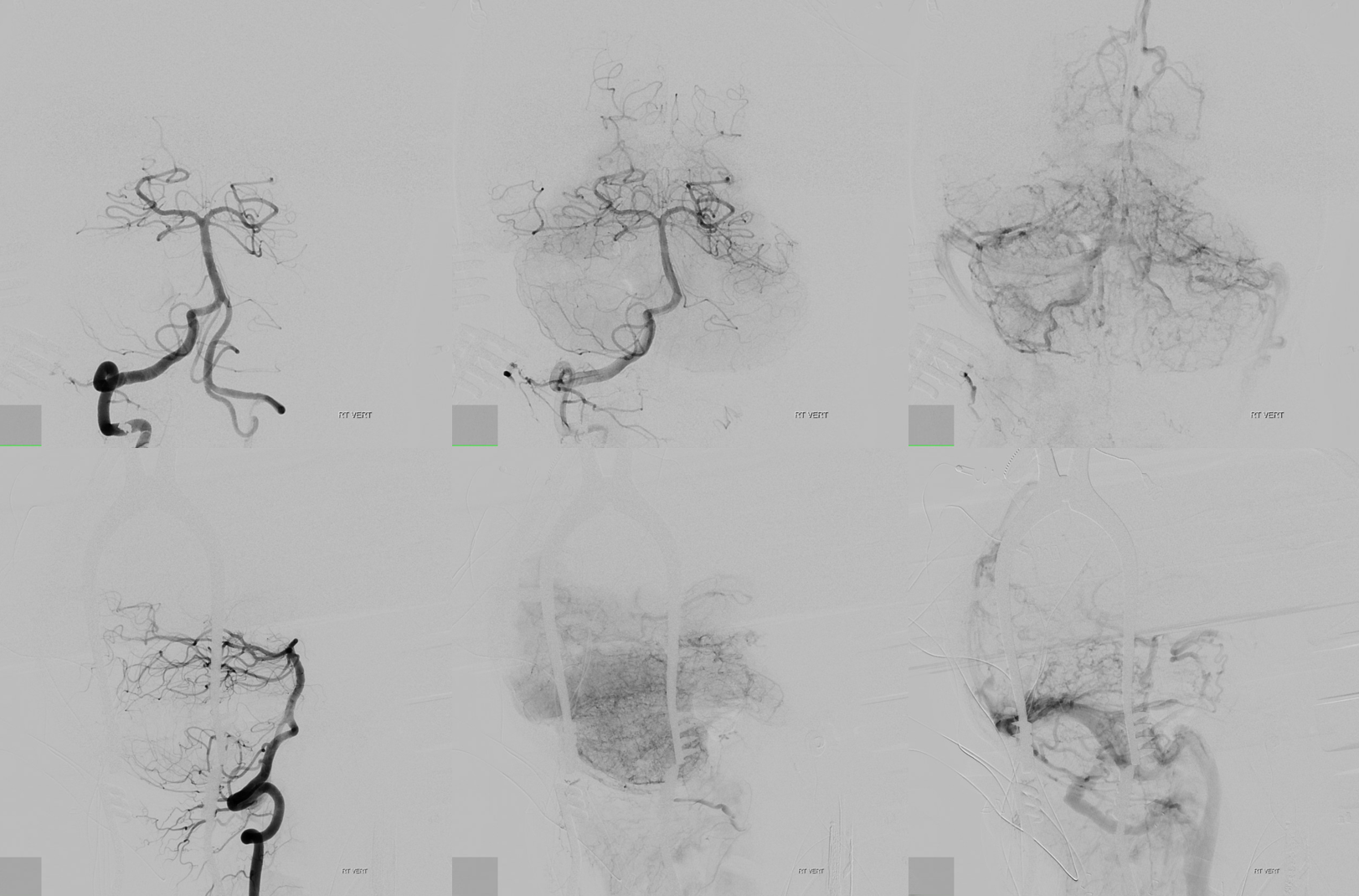
Angio — tons of venous congestion
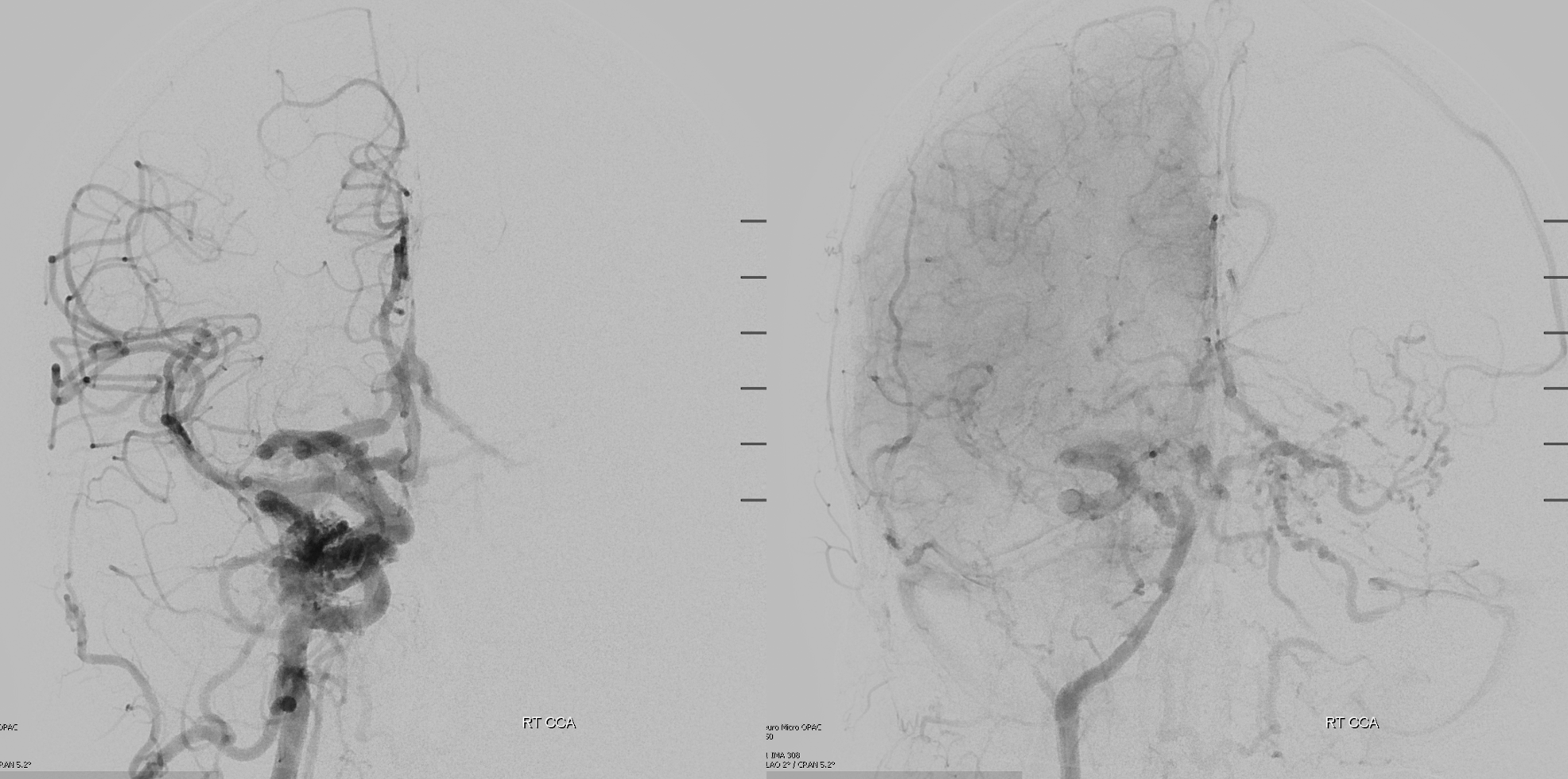
Lots of info here – and no arrows
DYNAs are important — and beautiful anatomy — these are cross-eye stereos
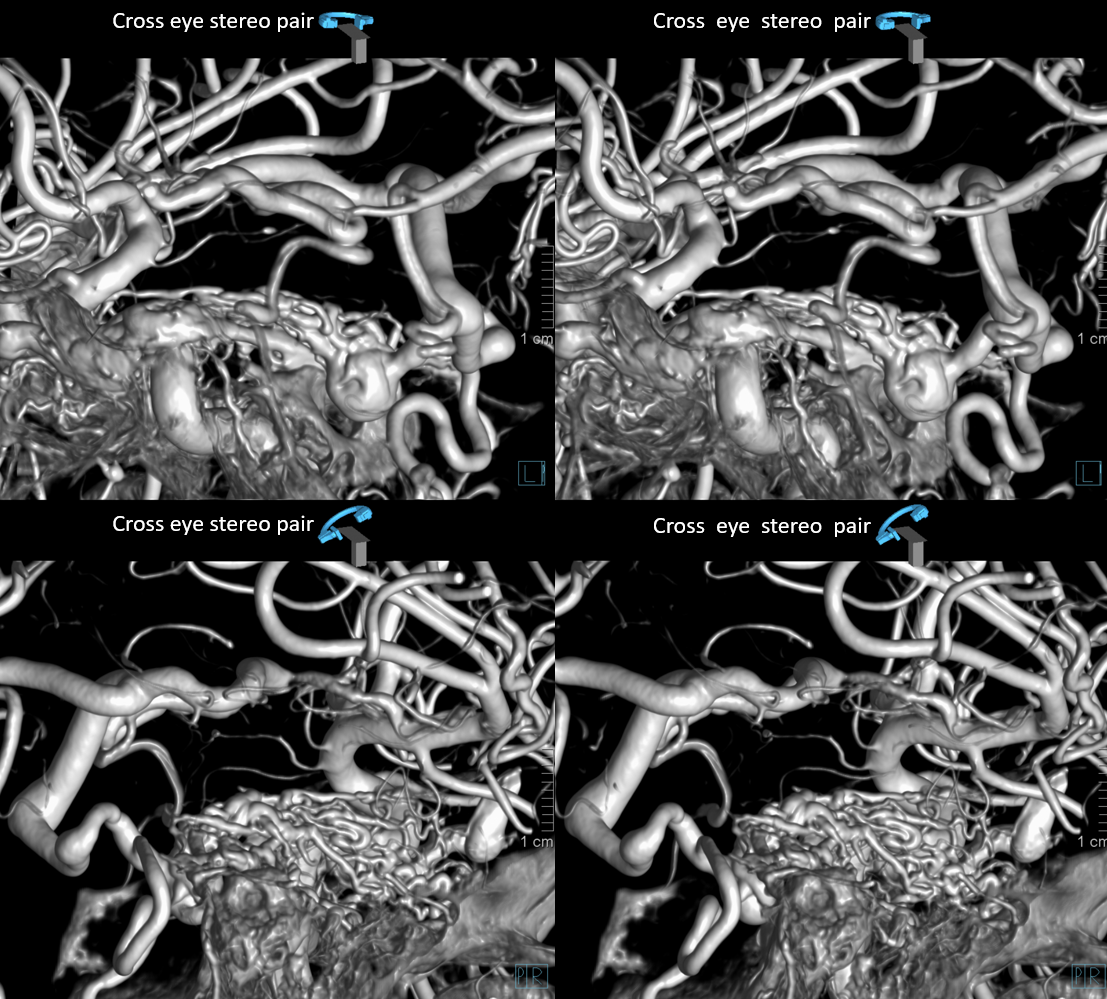

Source movies of DYNA
If you are a disciplined student — don’t look at the arrows below right away. Try to figure it out on your own. If you have, and want the answer key, or for whatever other reason — see below.
Dashed black arrow — fistula point. Black arrows — innumerable arterial tributaries along the lateral tentorial arcade. White arrow — petrosal vein, connecting to lateral mesensephalic vein (black ball arrow). The key to understanding venous problems here is to appreciate what veins are occluded. The straight sinus is — thus there is tremendous venous congestion — involving basal vein (black square point arrow), also congesting the anterior spinal venous system (black arrowhead). Dashed white arrow — short segment of petrosal vein, connecting the fistula to the superior petrosal sinus (open white arrows). Normally, it should connect to the sigmoid sinus — but it doesn’t (another point of occlusion). Instead, the outflow is directed into the cavernous sinus (open black arrow), which also has nowhere to go except the superior ophthalmic vein (dashed open white arrow) — hence the visual symptoms. A focal stenosis (white arrowhead) of the SOV with the angular vein is a potential problem for classic groin transvenous approach.
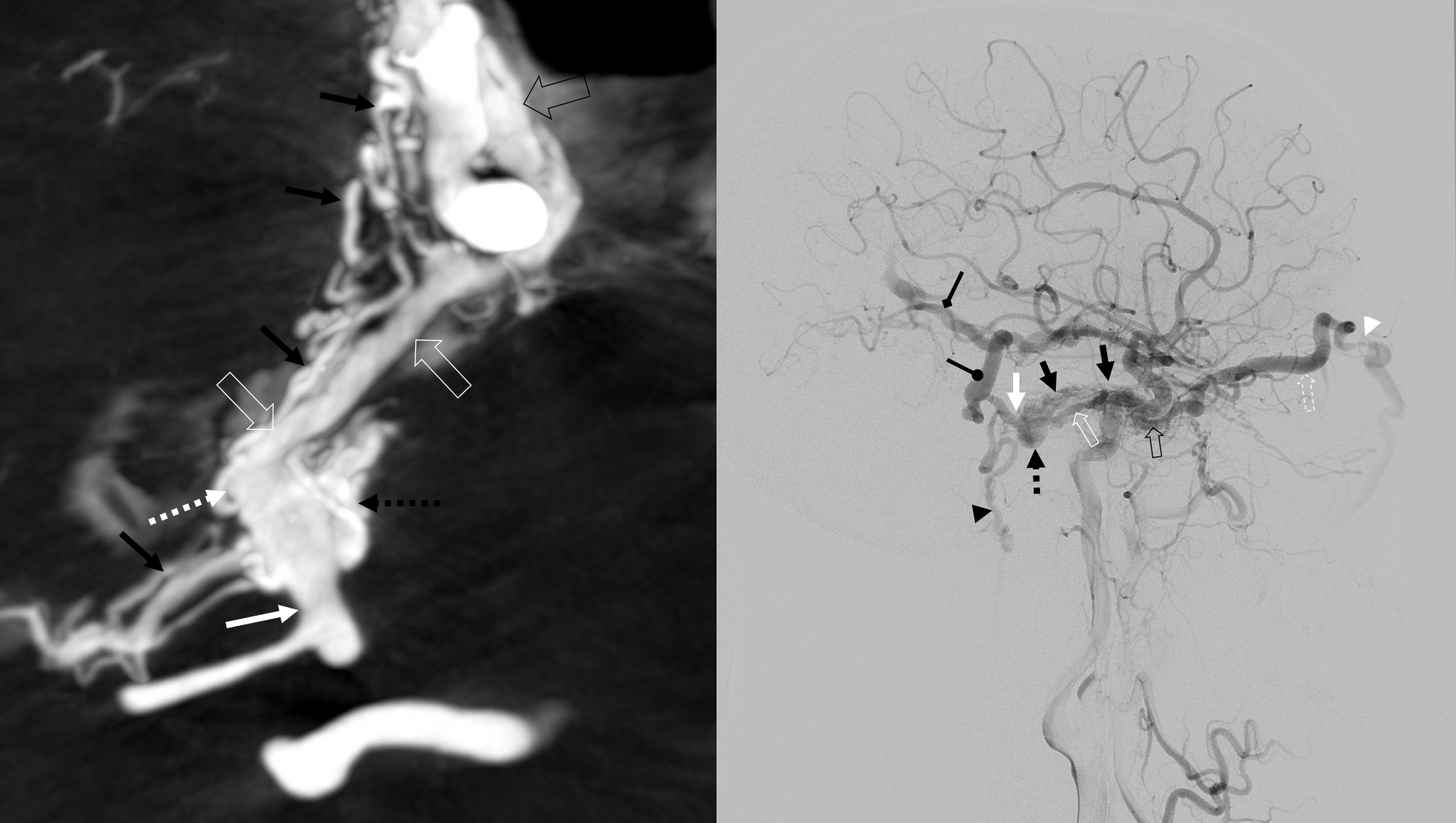

What are the options? Transarterial is bad. There is nothing decent that comes close enough to the fistula, and all major feeders will endanger cranial nerves or have serious EC-IC potential. Transvenous is certainly possible — via cavernous sinus connection with the superior petrosal sinus, aiming for subselective occlusion of the subarachnoid component (dashed black arrow) and its draining petrosal vein (dashed and solid white arrows). There are three ways to get there — first, by classic retrograde catheterization of the angular vein, across that focal stenosis. Second, by direct puncture of the SOV — that usually requires a cutdown. Third, by direct transorbital puncture approach. The third one is probably the most sure — there is a nice target for entry at the very medial point of the inferior orbital fissure.
The other option is open surgery. It is probably the surest thing to work — certainly we can expect closure of the subarachnoid venous drainage (solid white arrow). The connection with SPS is also likely to be closed, and we can expect control of the AICA supply. The choice is surgery.
Below is an intraop video
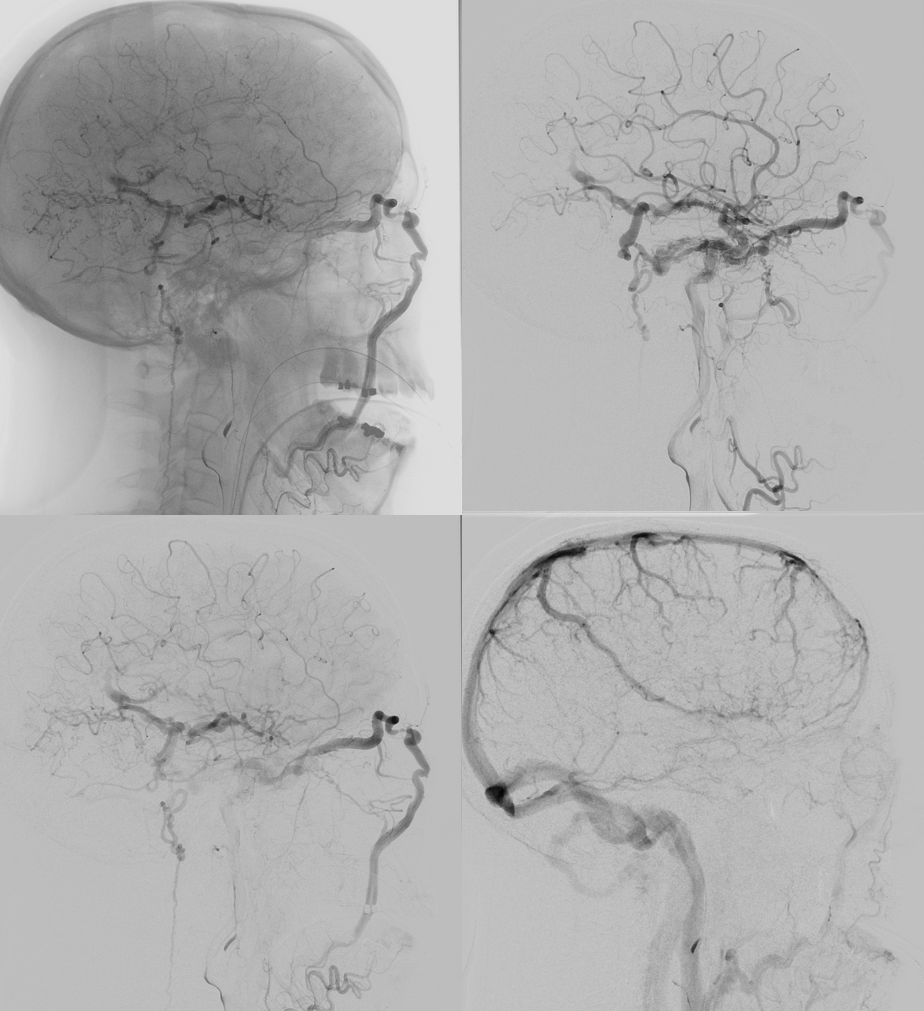
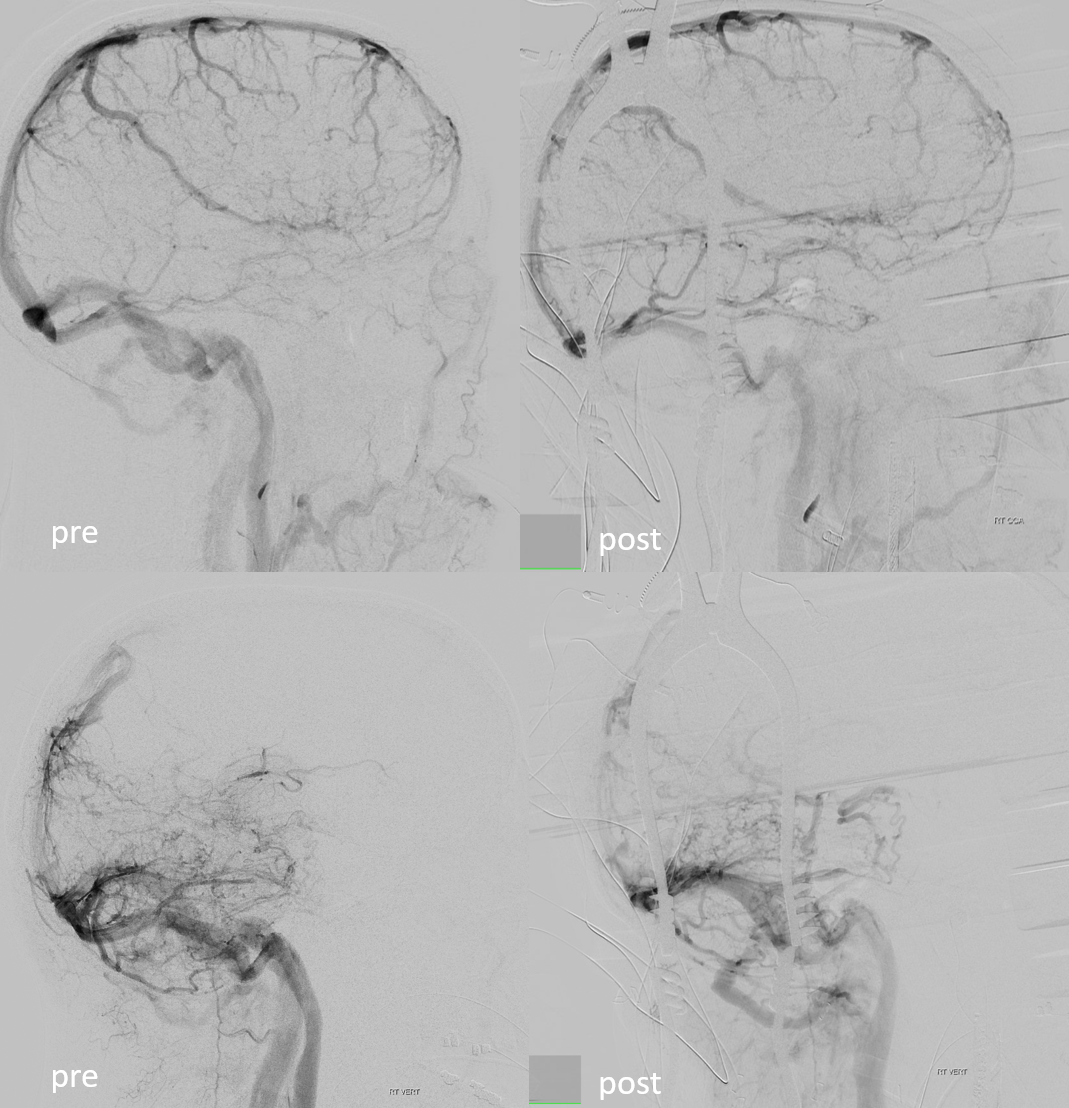
Intraoperative angiogram
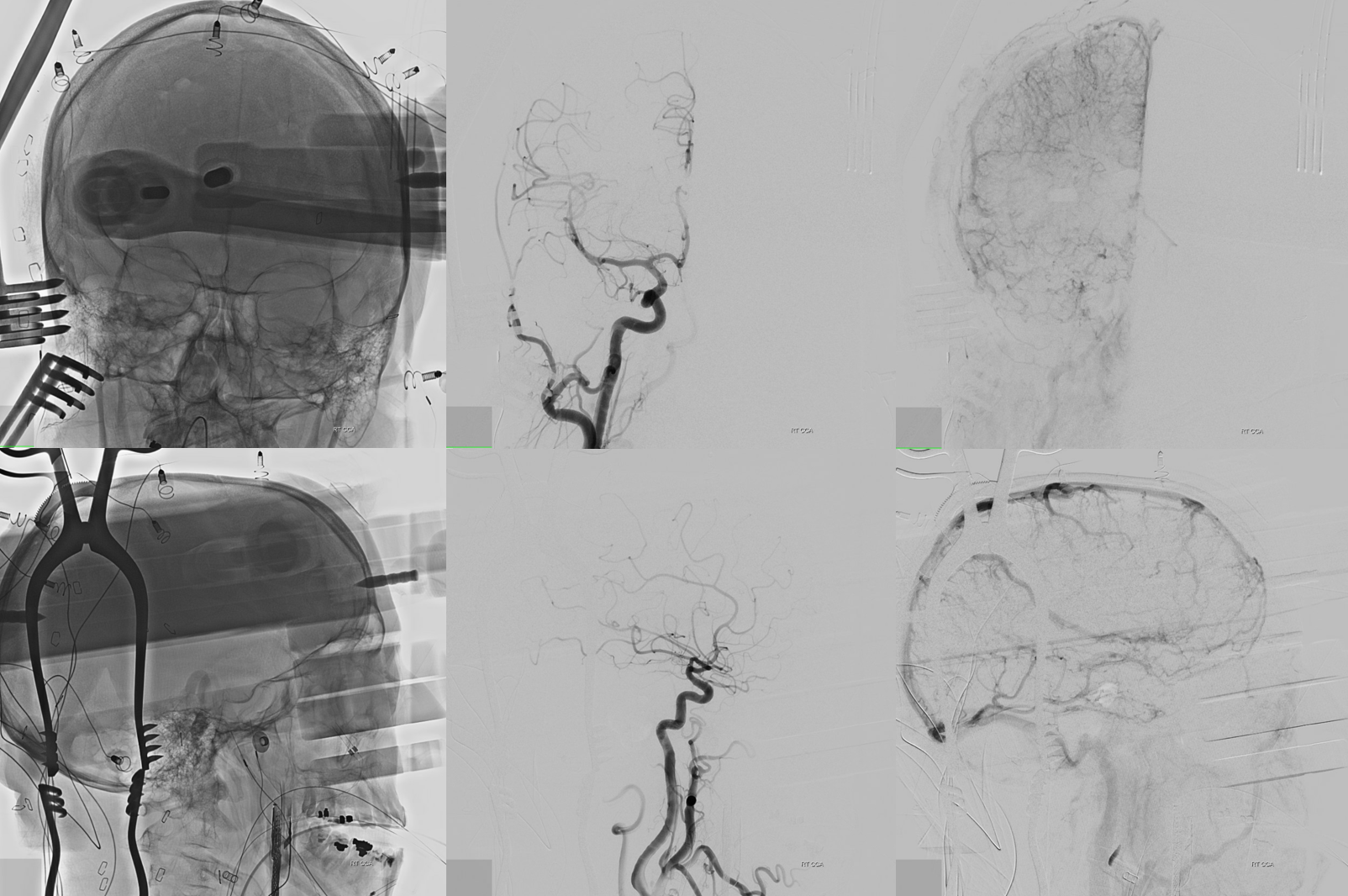
Can u see the labyrinthine artery below?
Before and after images of brain venous phase — there is immediate improvement in venous congestion, particularly of the vertebrobasilar circulation
That’s it — questions, comments — neuroangio@neuroangio.org
