The material / cases in this section were collected and organized by Dr. Guglielmo Pero. A neuroangio team effort!
A collection of complex cases that are very important in their own right, and highlighting how Cone Beam CT is essential if you want to go for the big ones.
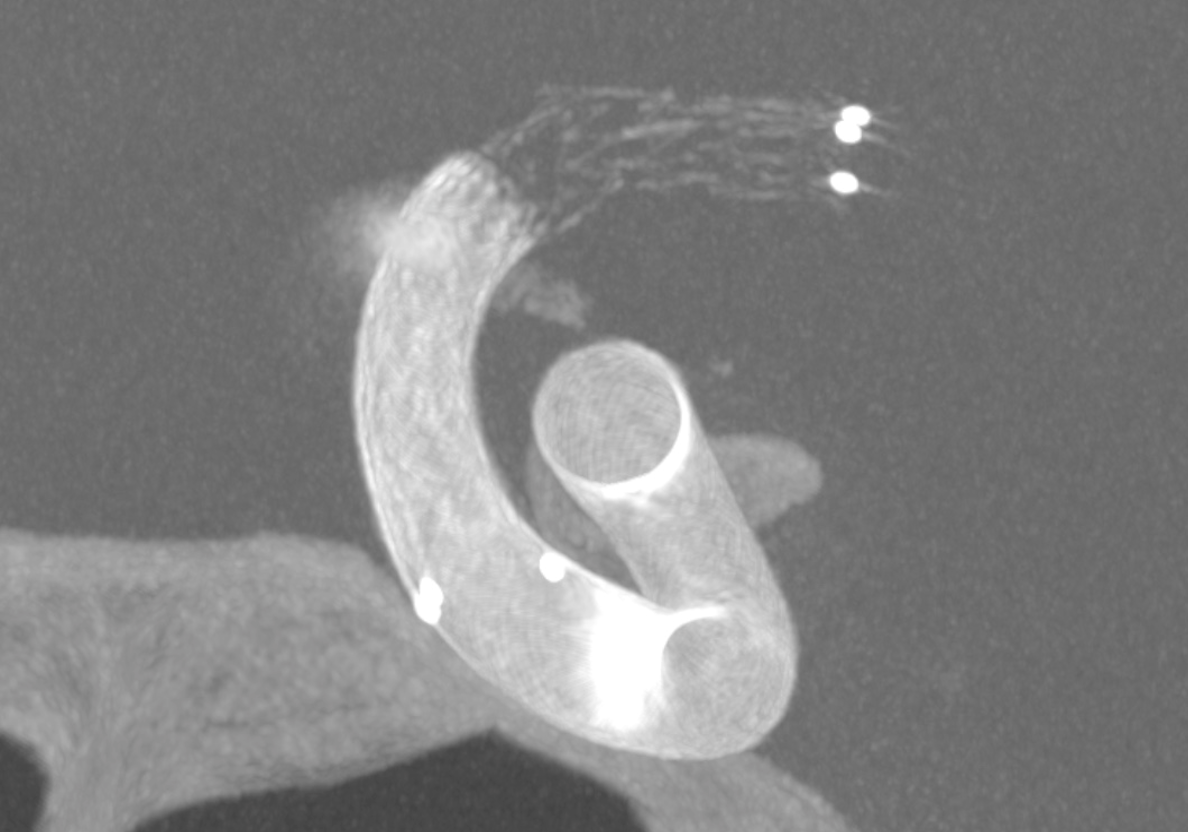
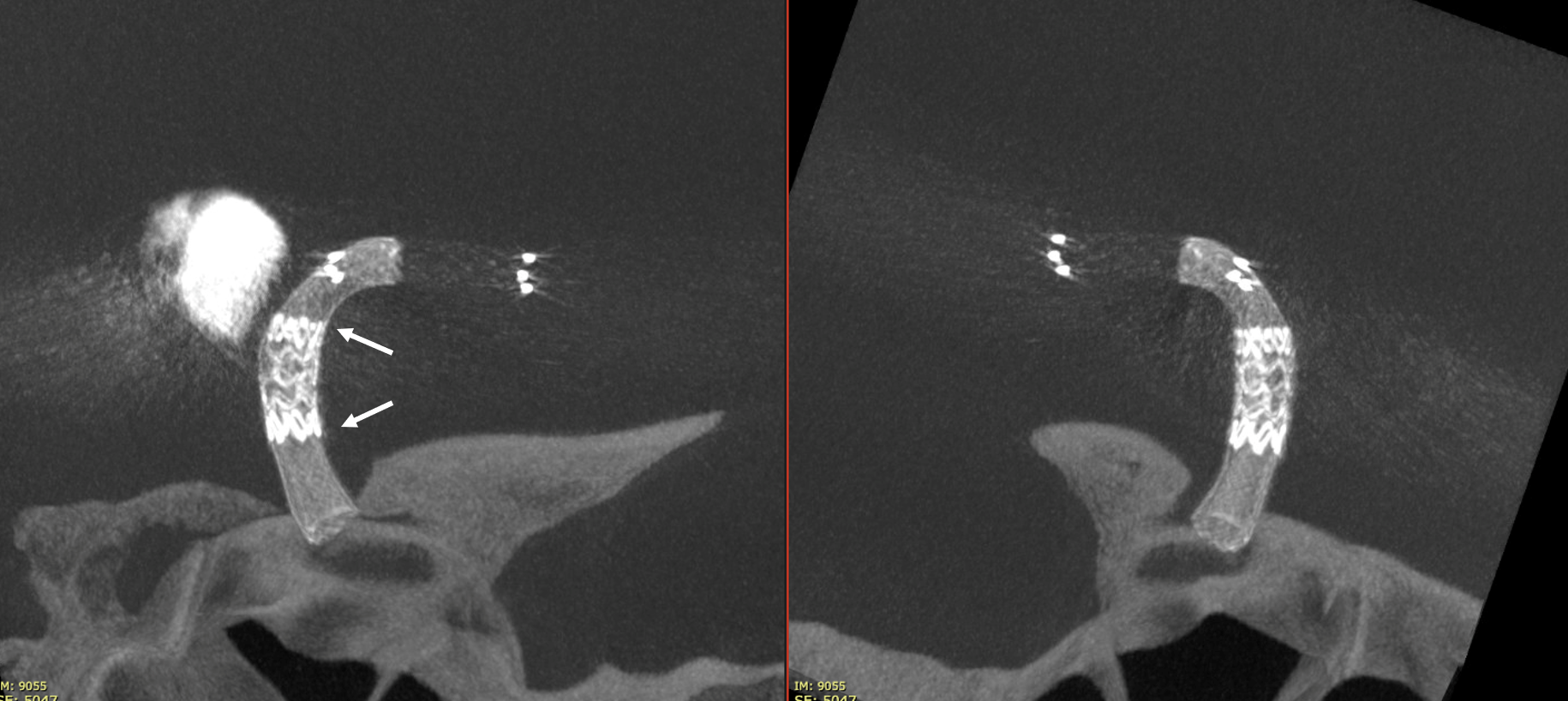
Not injected Vaso-CT, 22 cm FOV 20 seconds acquisition, followed by a secondary reconstruction with 50% FOV and 5123 resolution; Thick MIP. In this case, a Pcom aneurysm, a Derivo 2Heal was used. After the stent release, a minimum distal fish mouthing was seen, so we decided to immediately add a Pegasus stent.
We can see the struts of the Pegasus irregularly open in the carotid bifurcation. We can even recognize the typical distal end of the Derivo with the folded wires.
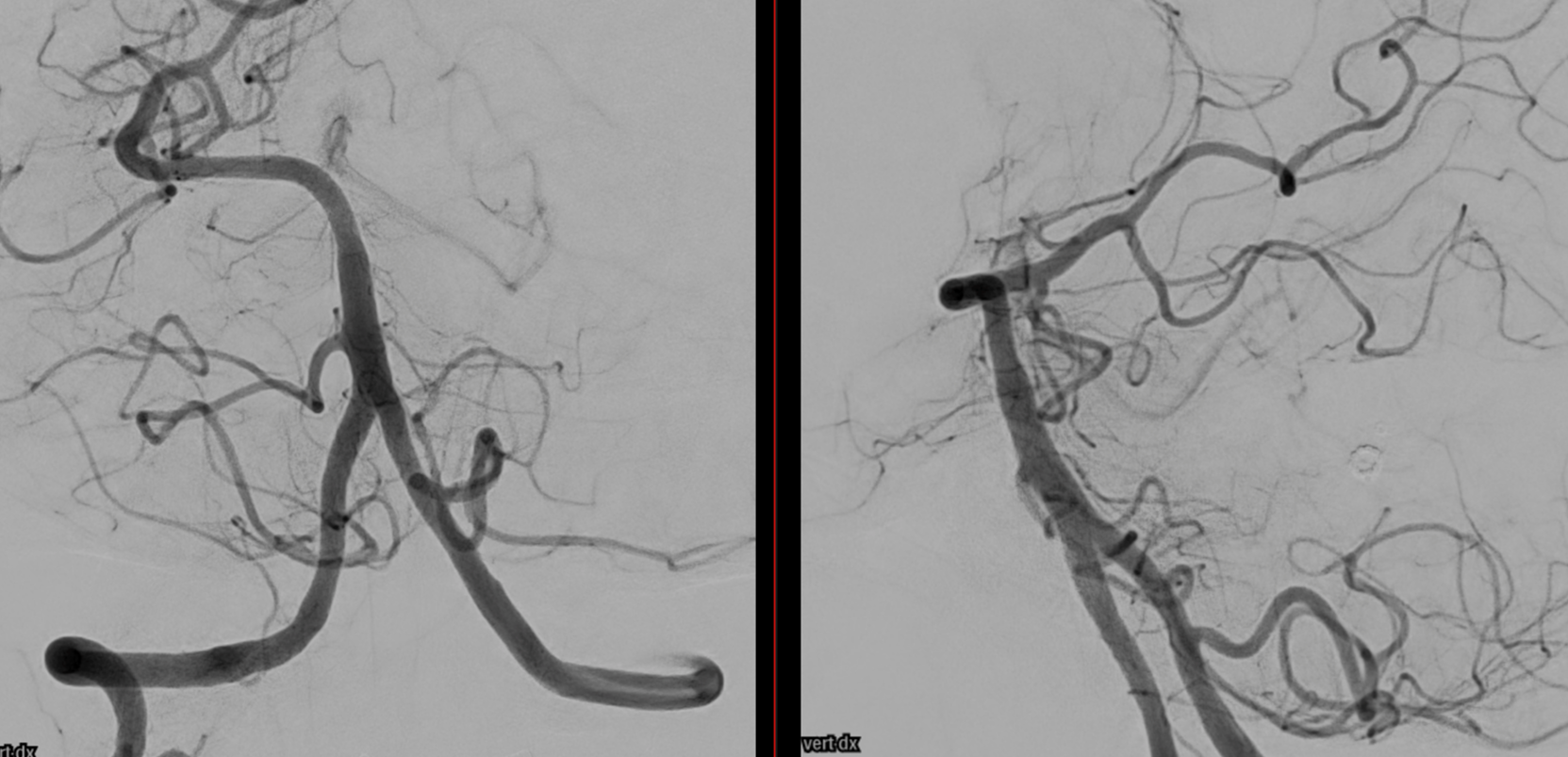
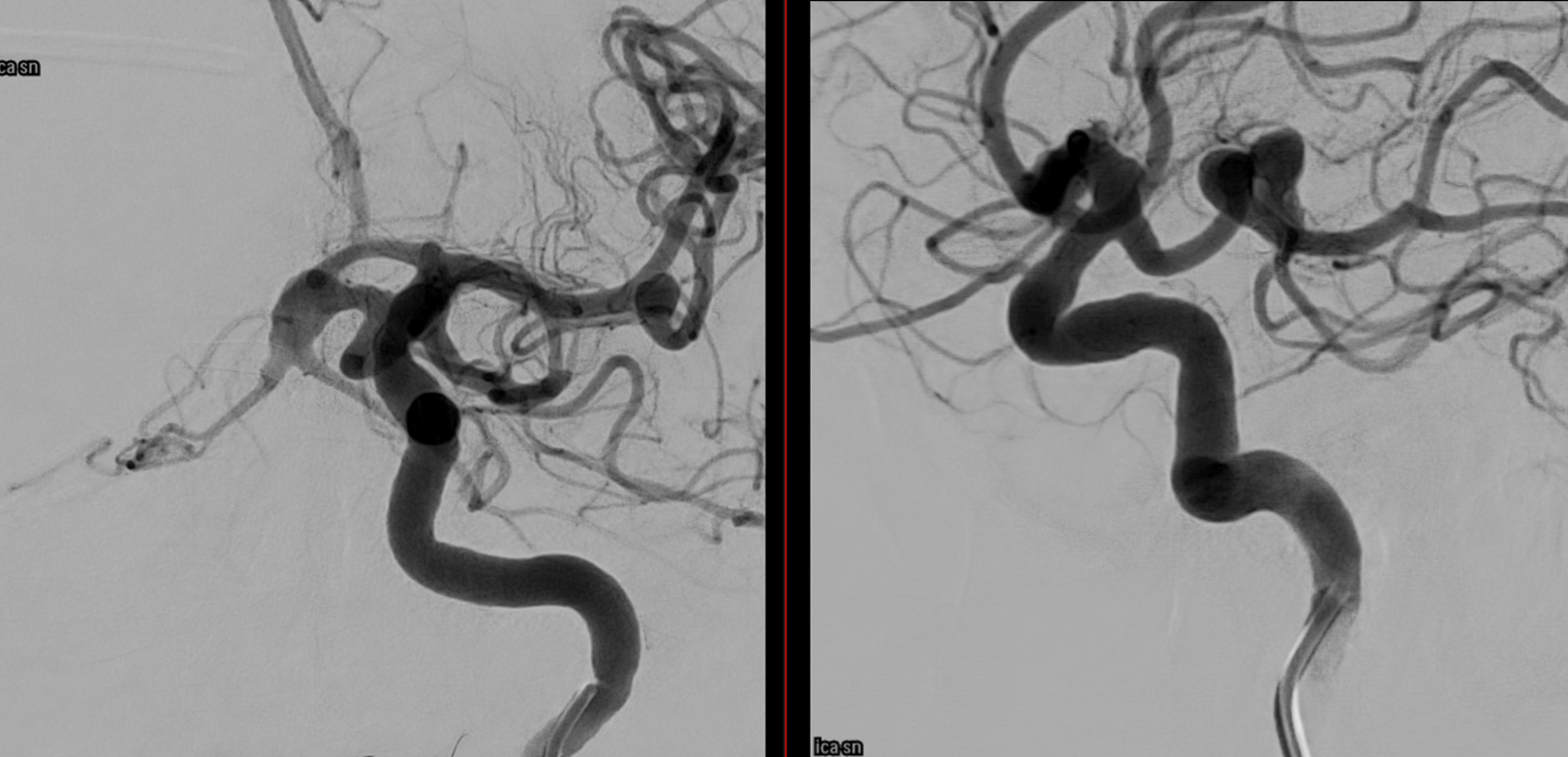
A symptomatic unruptured MCA bifurcation aneurysm in a young woman
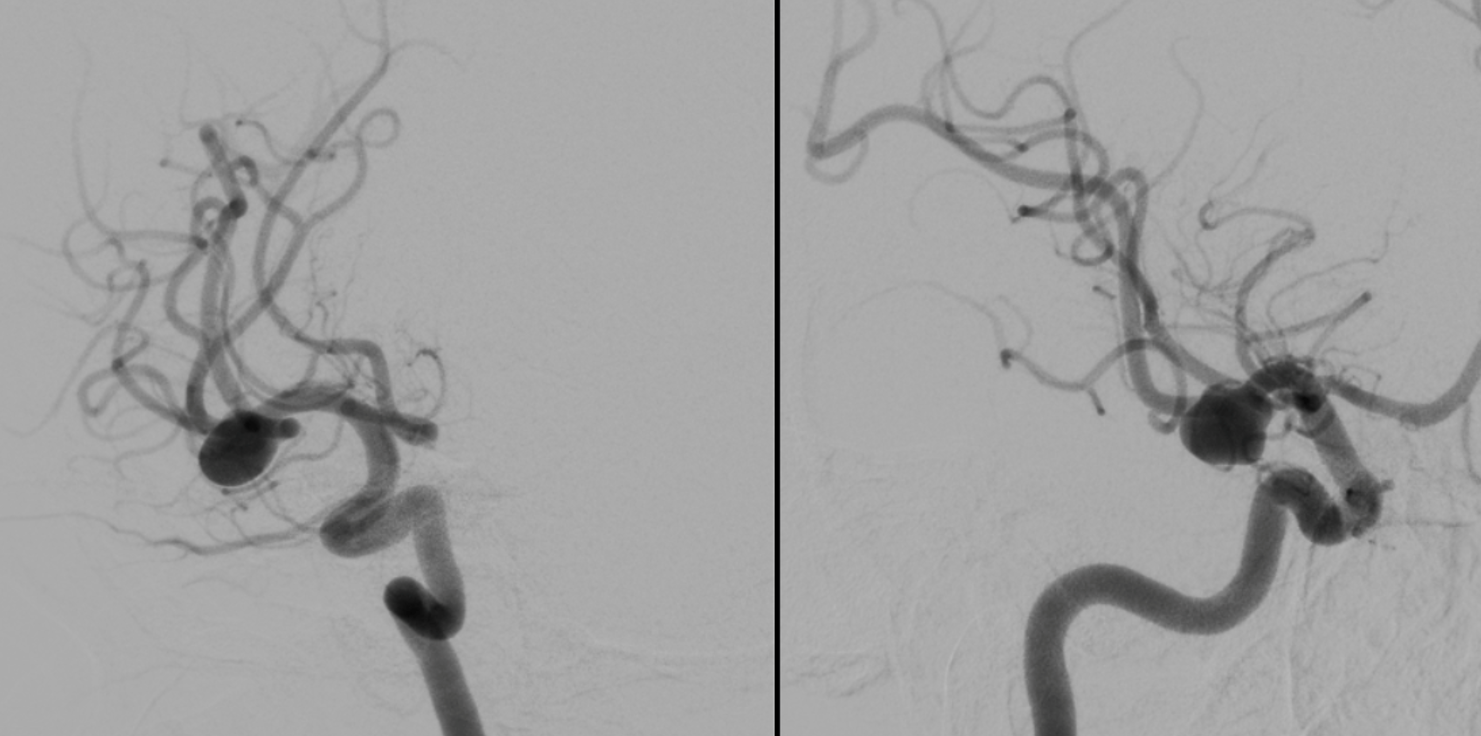
This video was made with Horos from the original 3D dataset (3D 5 seconds 15 cm FOV acquisition, manually injecting pure contrast – 250 mg/ml – with a 20 ml syringe).
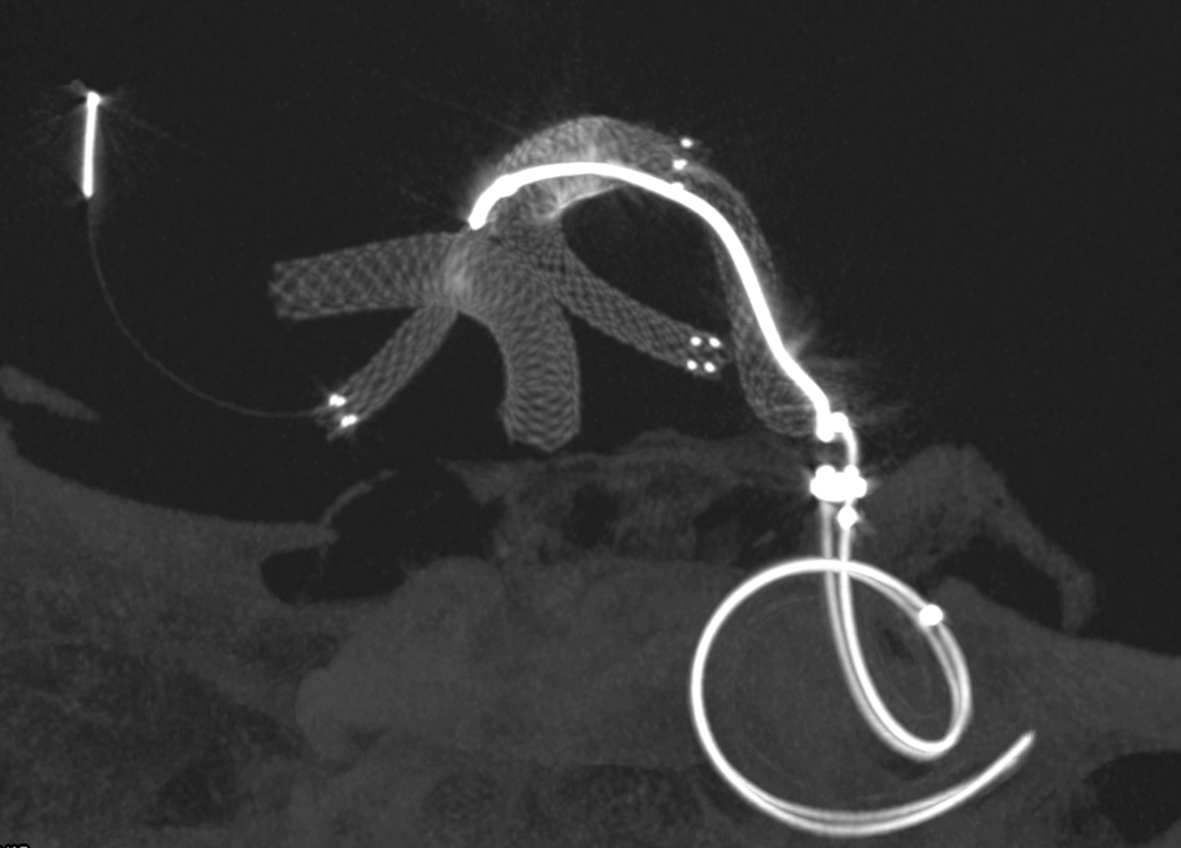
Noncontrast Vaso-CT, 22 cm FOV 20 seconds acquisition, followed by a secondary reconstruction with 50% FOV and 5123 resolution; Thick MIP.
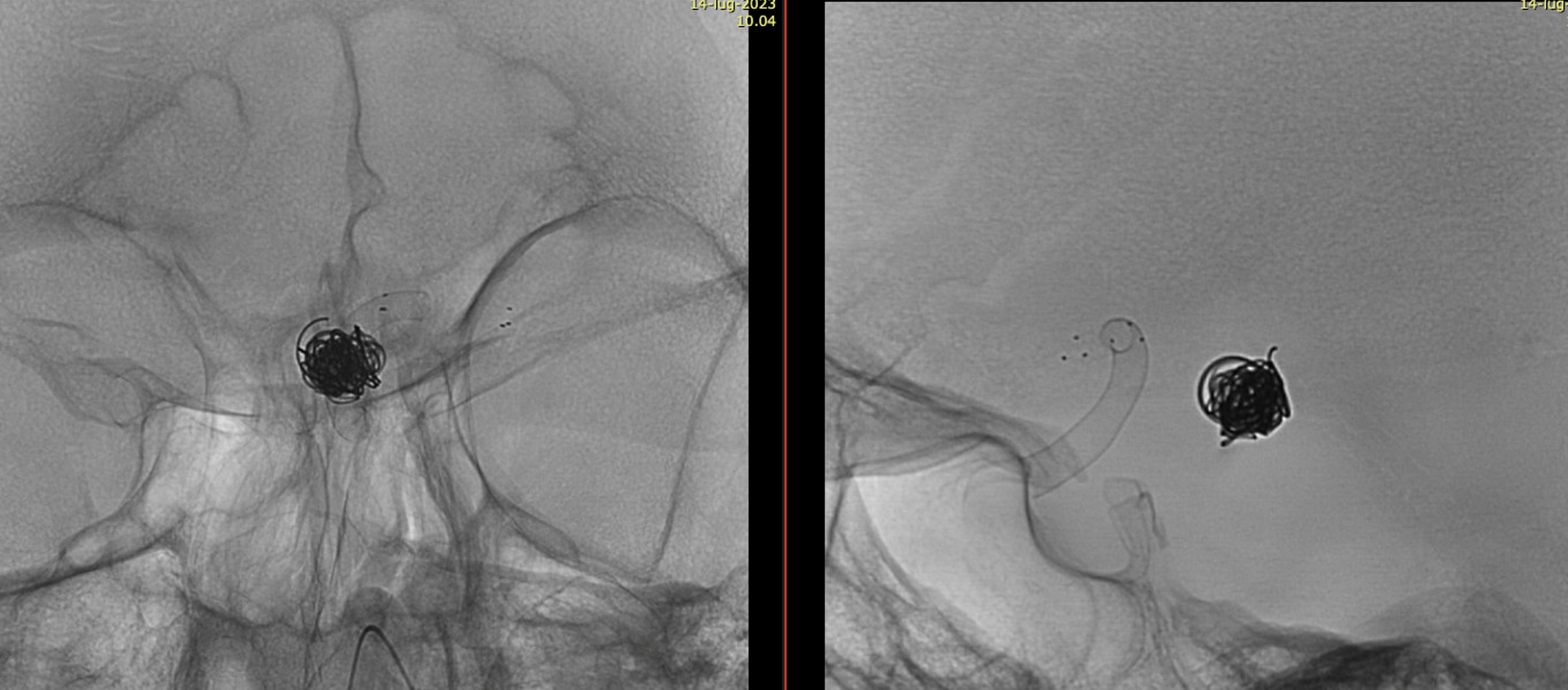
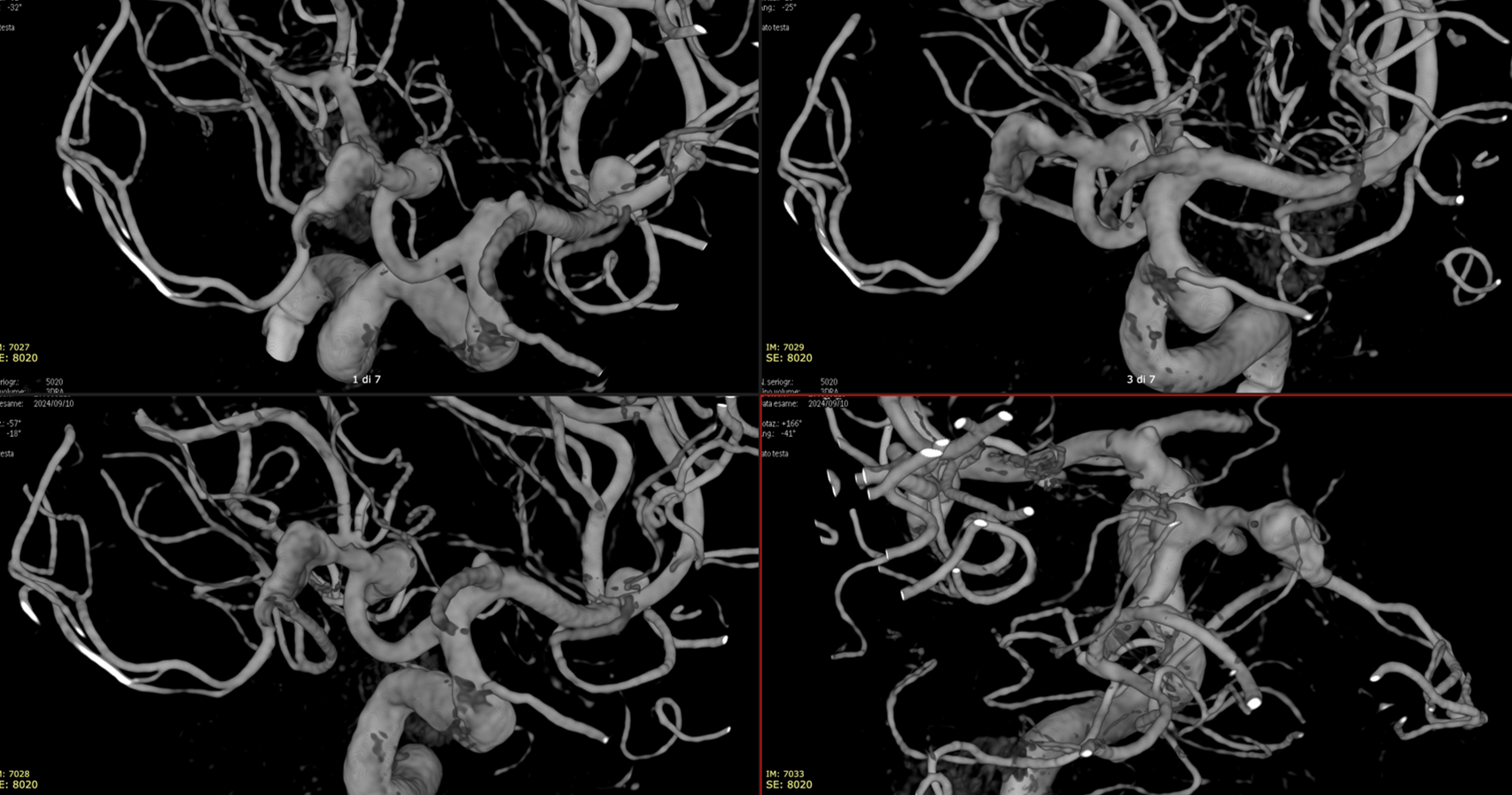
Wide neck MCA trifurcation aneurysm.
Y stenting with Atlas and Lvis Evo, in emergency. The Atlas diameter was too large because of the temporary limited availability in our centre; we can clearly see the struts of the Atlas too open at the level of the aneurysm neck (arrow). Even the microcatheter for coiling is fully visible jailed by the Lvis Evo in M1
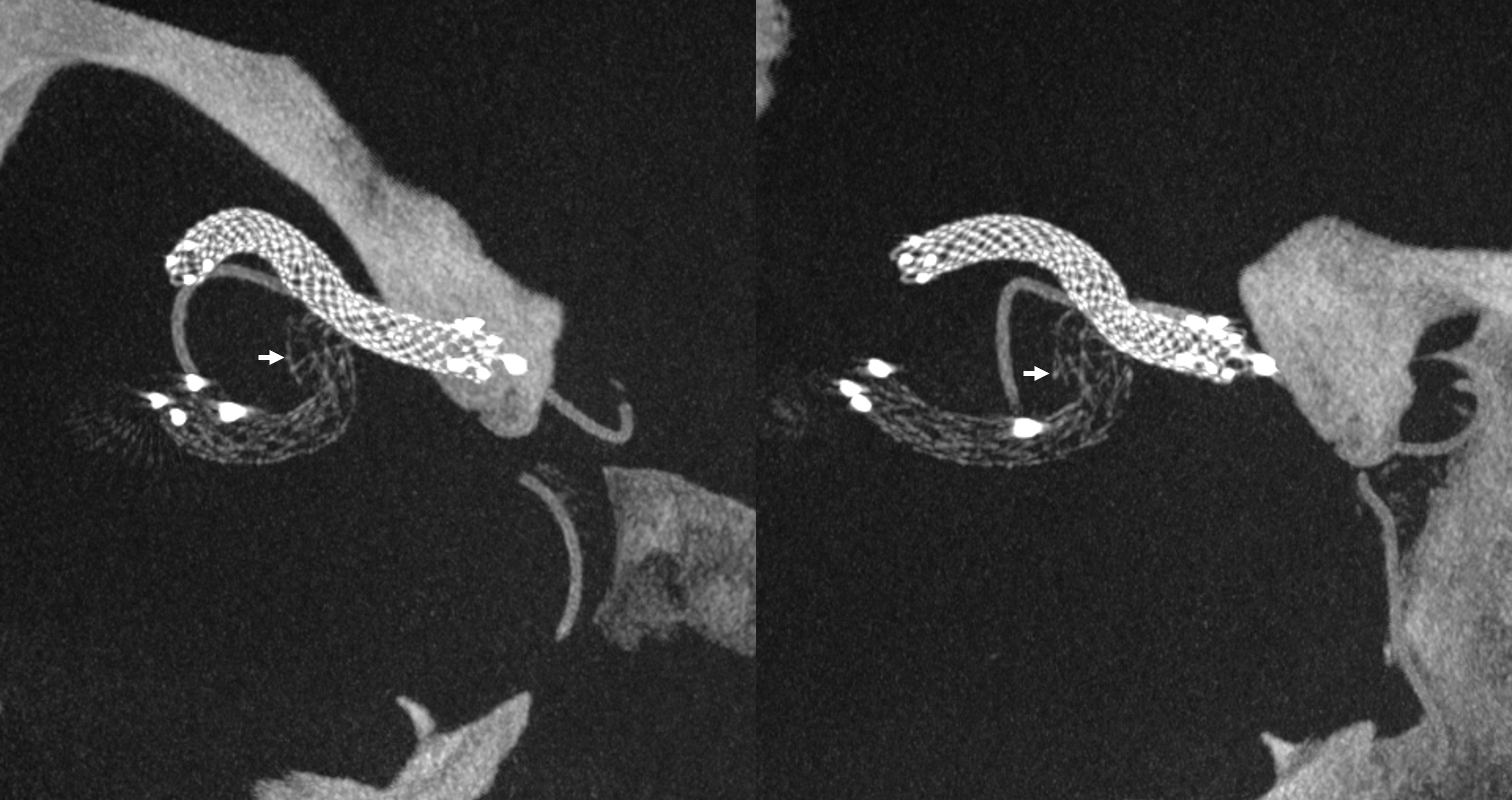
The injection of contrast medium (250 mg/ml, 50% dilution, manual injection, same reconstruction protocol as previous images) reduces the visibility of the struts — an important point to consider. Not everything is always the same contrast dilution, same injection rate, etc. etc. — you need to know how to vary every parameter to achieve desired results.

Important Case of Aggressive Anterior Choroidal Aneurysm
This is a specific subtype of ever-growing choroidal aneurysm that is extremely difficult to solve without complete occlusion of the aneurysm and the choroidal artery. Fortunately, perhaps because of the unique aneurysm biology, choroidal occlusion tends to be mildly or not at all symptomatic.
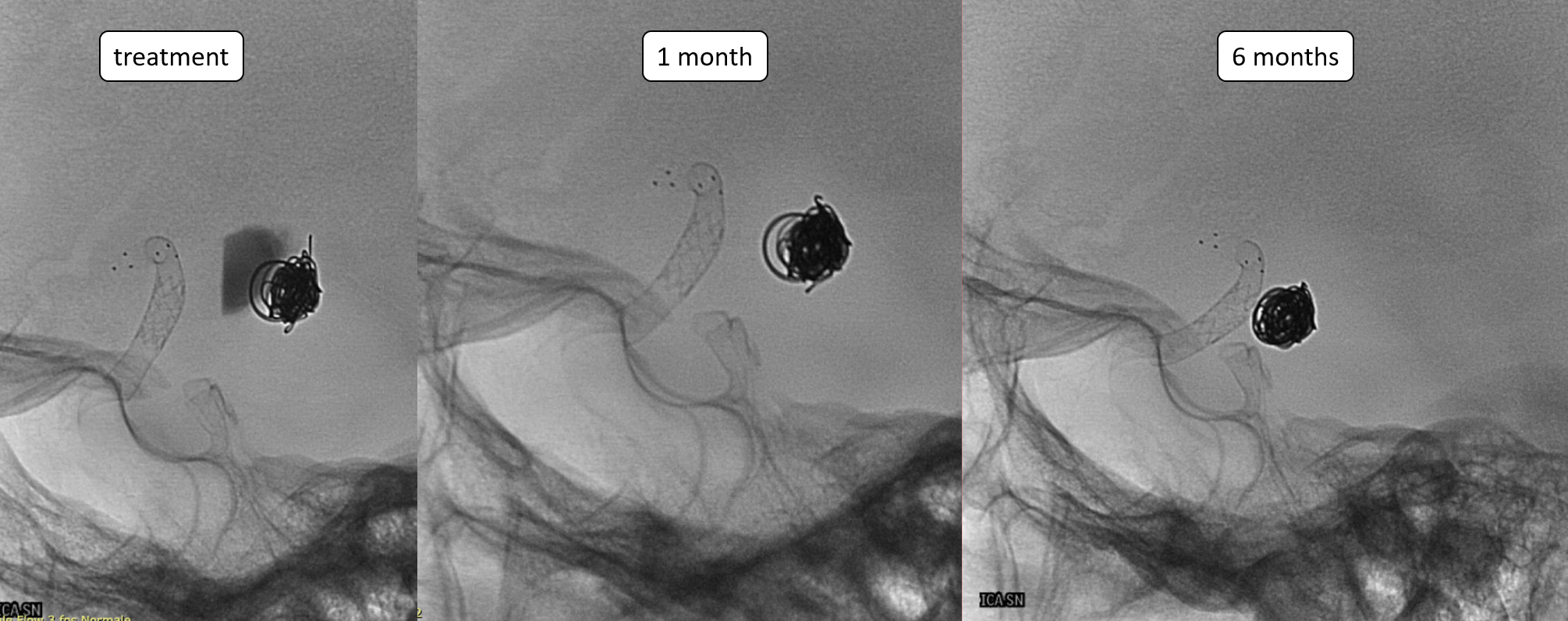
A young man with an unruptured but symptomatic dissecting aneurysm at the origin of the Anterior Choroidal artery. Treated in acute phase with coils; in the meantime the aneurysm has grown.
A Silk Vista was implanted a couple of weeks after coiling
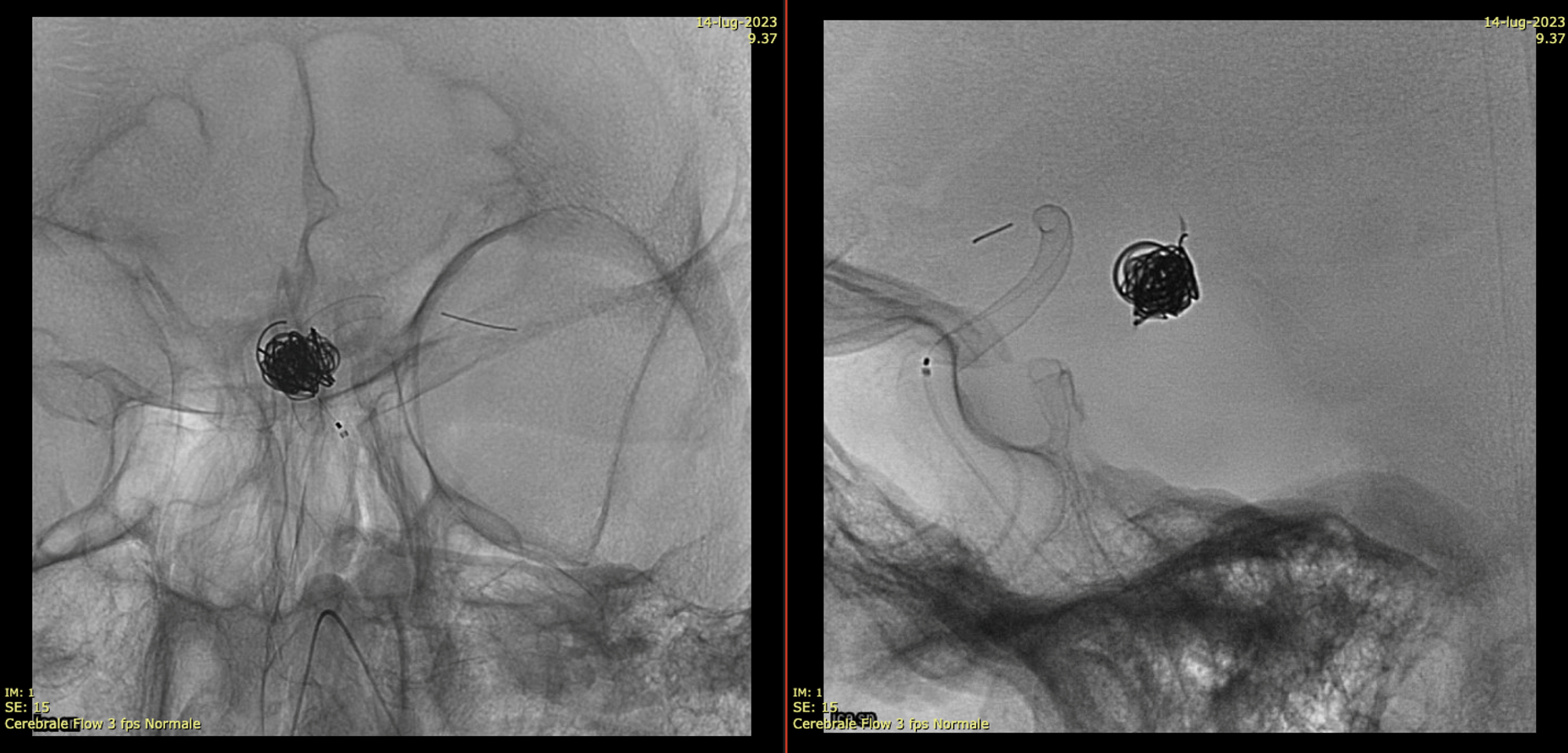
Immediately after the release of the SV, we saw a minimum movement of the distal end to fishmouthing
A Credo stent was used to keep the SV apposed to the vessel wall
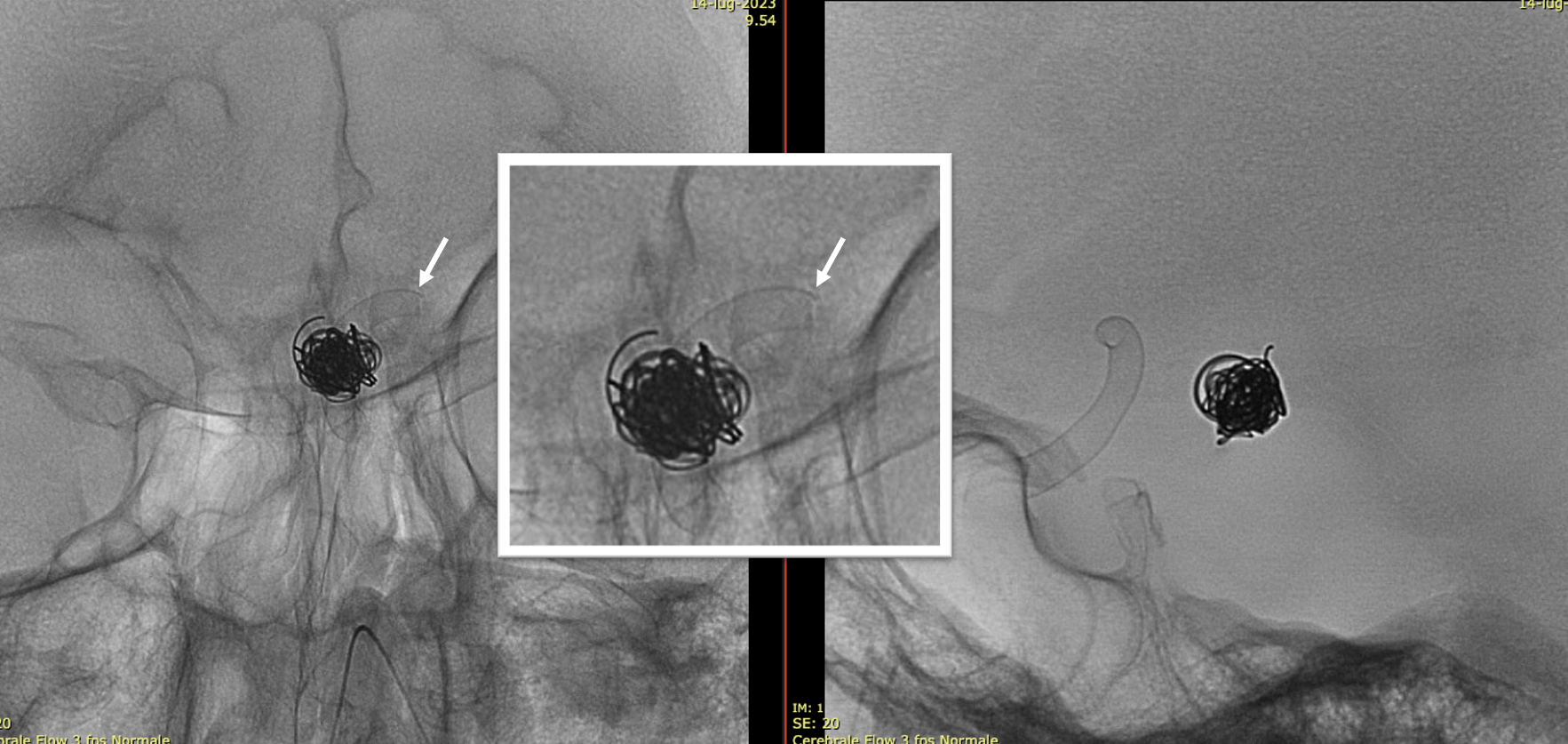
One month later the aneurysm was still growing — as they frequently do.
A Bentley Coronary Stent 3 x 8 mm was implanted, progressively inflated (even with a 3.5 PTA balloon) until no more contrast entered the aneurysm. The USA version of Bentley is the Papyrus — Bentley is better.
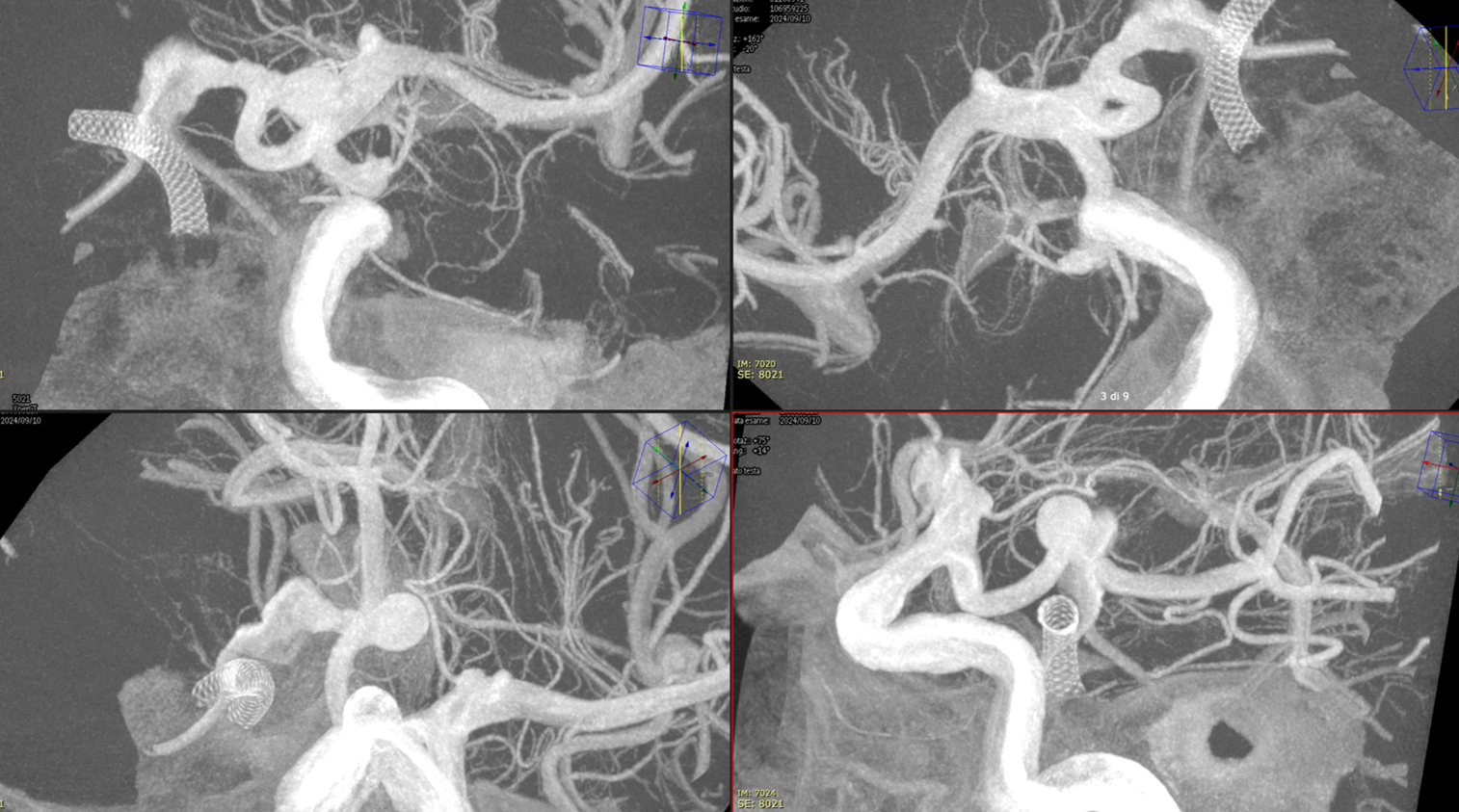
Noncontrast / dry Vaso-CT, 22 cm FOV 20 seconds acquisition, followed by a secondary reconstruction with 50% FOV and 5123 resolution; Thick MIP.
We can clearly see the three stents. The Credo seems too rigid and probably is not fully open in the curve. The Bentley (arrows) is a little bit overinflated (consider that at this level the coils reduce the image quality). SV is open with some irregularity.
This is the problem with using laser-cut stents for fishmouthing. Alternative is a relatively low coverage braided stent like Evo or LVIS Jr.
Beautiful simple images of aneurysm shrinkage and mass effect relief
Very Important Case of Aggressive Basilar Bifurcation Aneurysm
Unruptured basilar tip aneurysm treated in 2010 with PED between right P1 and basilar.
Make sure you don’t judge — we know much more about how these behave now than in 2010 — and many people today still coil these with laser-cut stents and mess up options for the guaranteed recurrence

The aneurysm was kept open by the left (contralateral) PCom — again, we know this much better now than in 2010. And its very important.
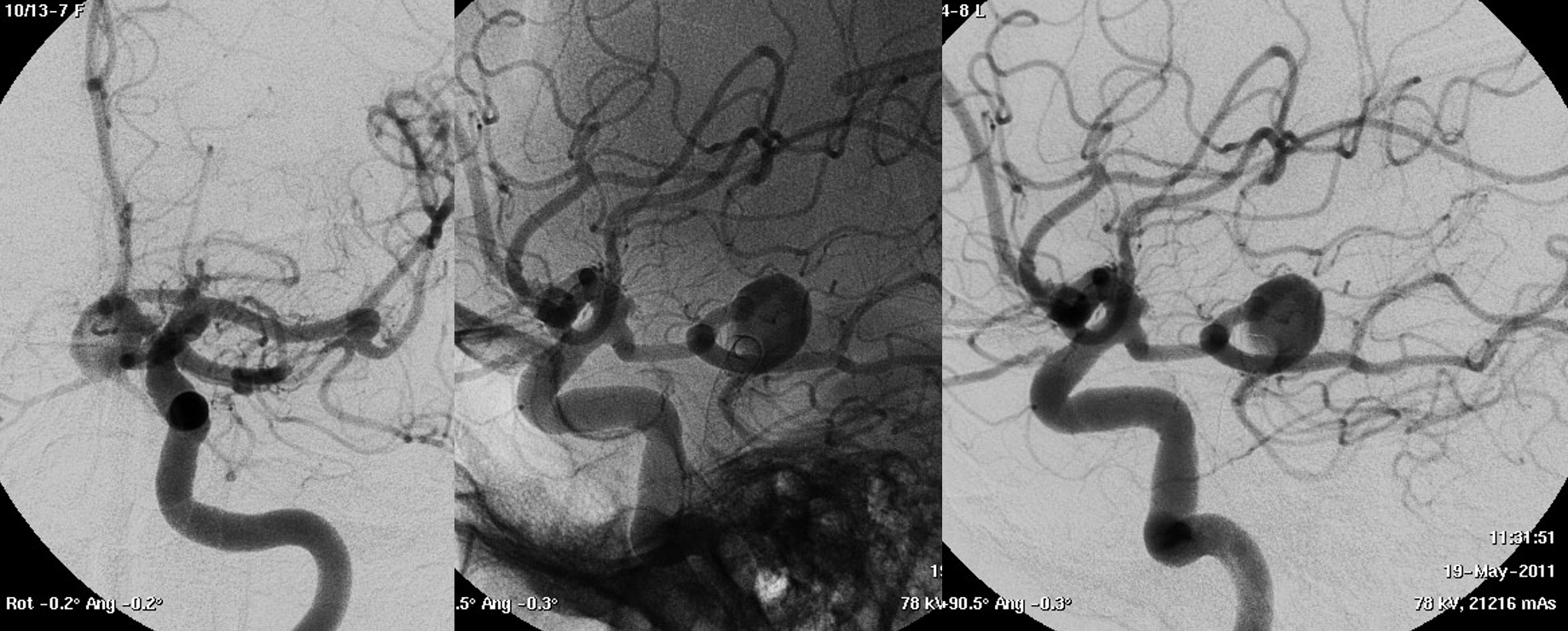
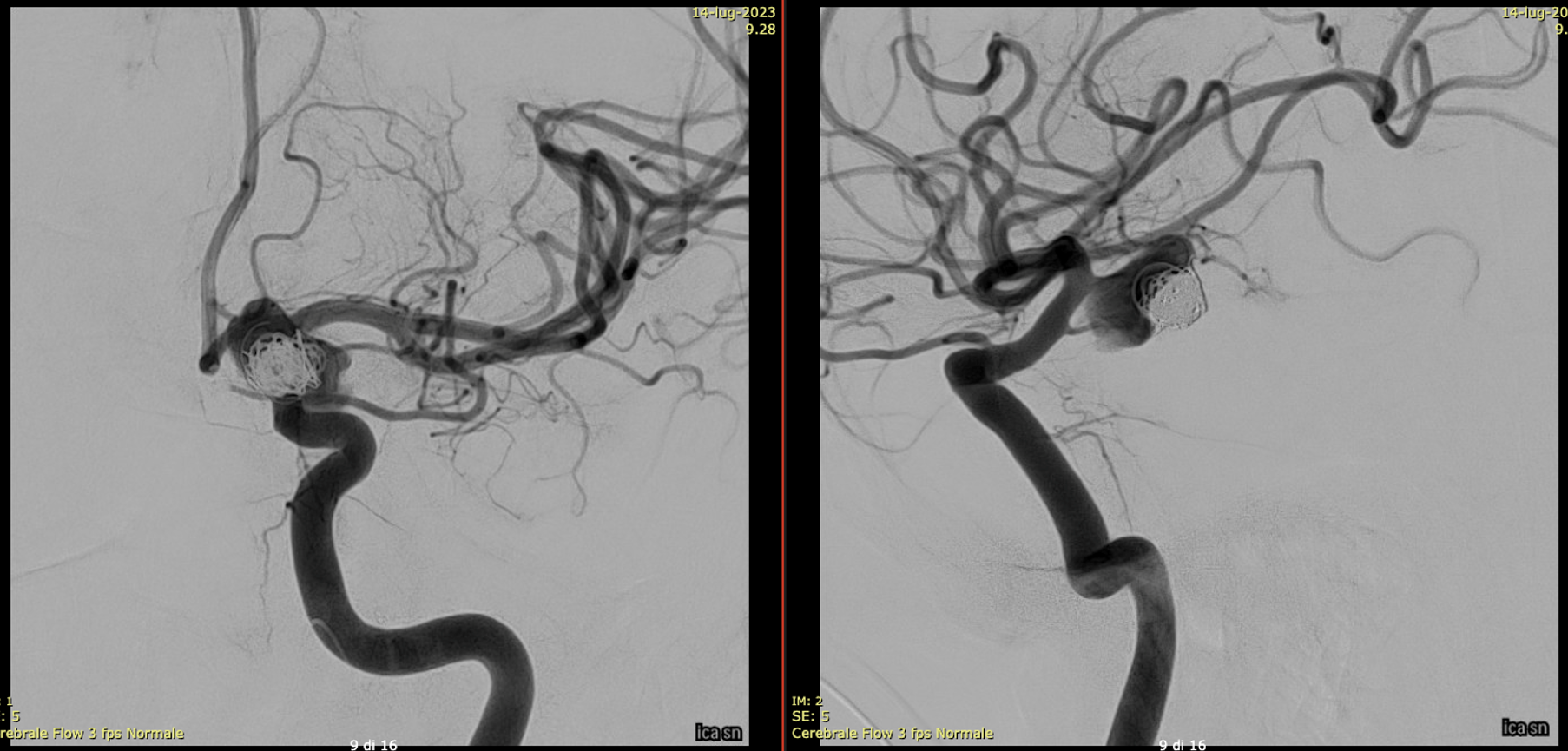
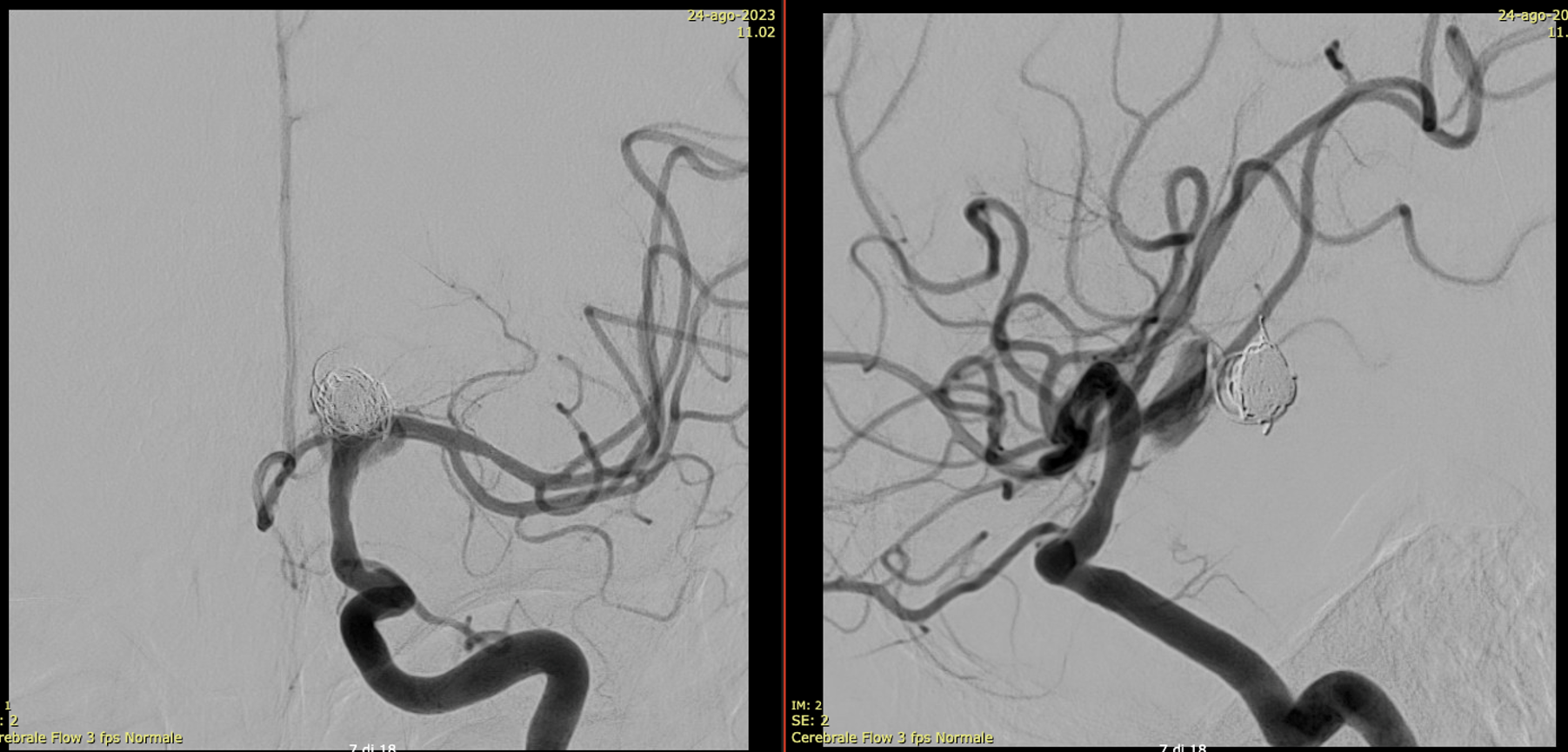
13 year later. The aneurysm was mostly thrombosed and was growing, becoming symptomatic. The good old analog Philips workhorse is gone… Welcome to the digital world or Azurion
With manual compression of the left carotid — look how important manual compression or Balloon Test Occlusion can be
Left ICA — the preferential supply to bilateral SCAs is clearly seen
3D reconstructions of the left ICA (3D 5 seconds acquisition, 22 cm FOV, manual injection of pure contrast – 300 mg/ml – with a 20 ml syringe, no secondary reconstructions). Both the SCAs are injected by the PCom and the right SCA origin is shaped by the PED in right P1. Now in left P2 there is a fusiform dilatation, not present before
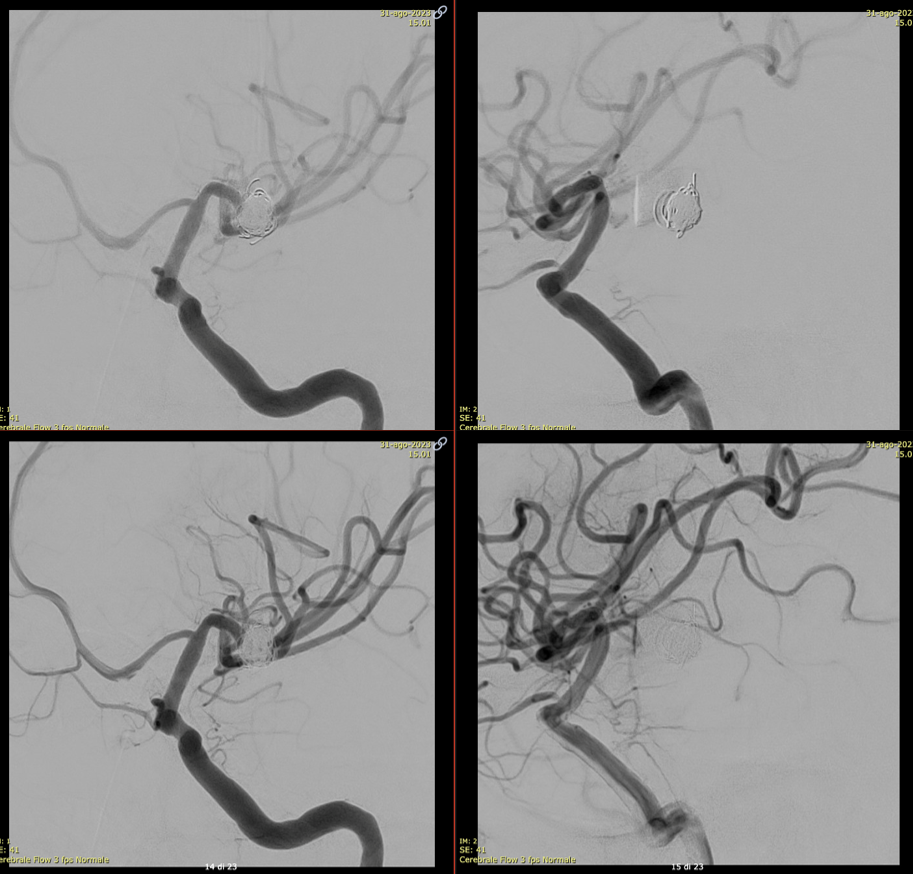
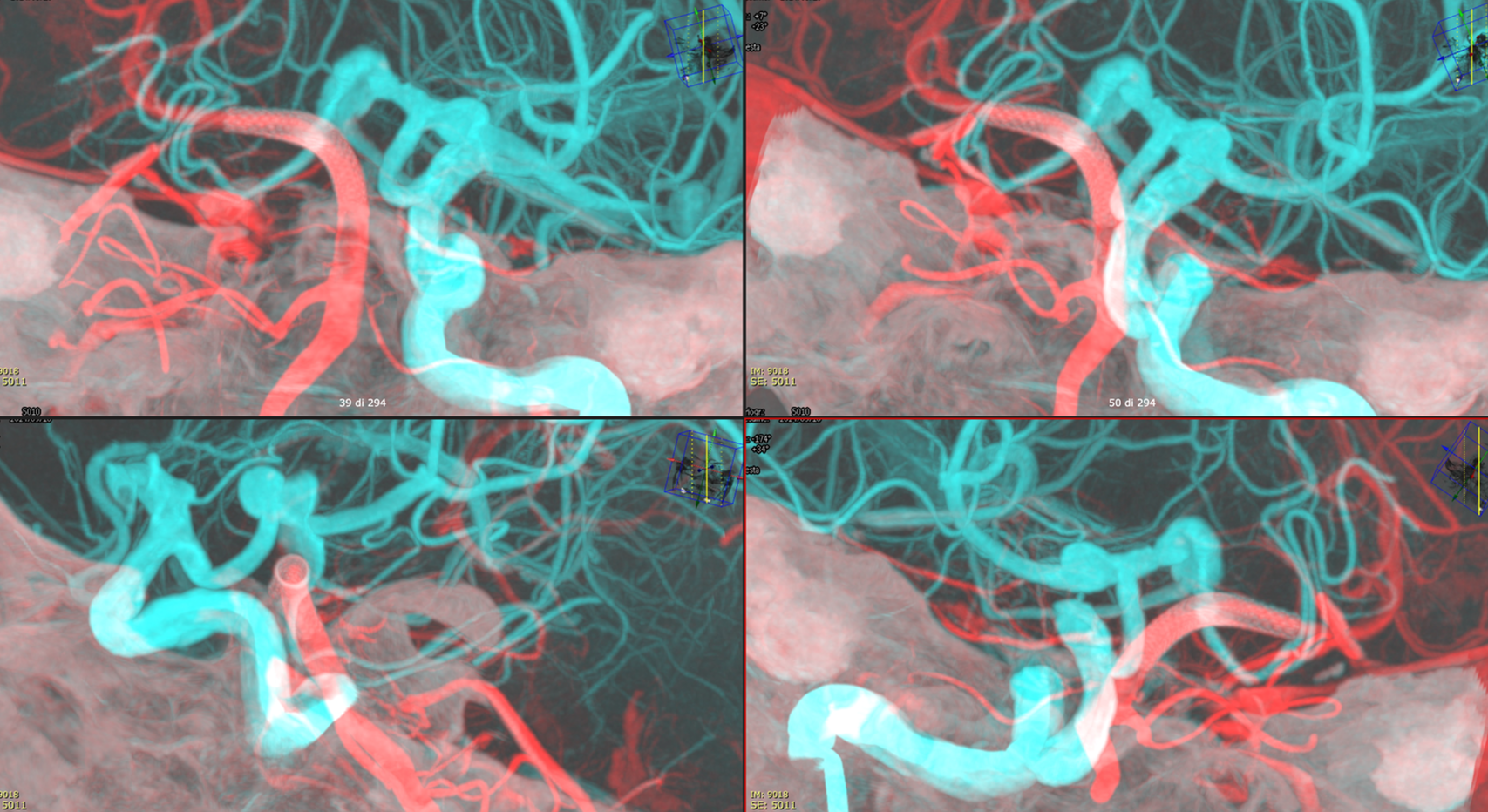
Vaso-CT, 22 cm FOV, 20 seconds acquisition, followed by a secondary reconstruction with 67% FOV and 5123 resolution; Pure contrast (300 mg/ml) manual injection in the left ICA. Thick MIP reconstructions
The protocol acquisition is the same of previous figure.
Fusion of the Vaso-CT of left ICA and posterior circulation (only one vertebral artery was injected, note the partial filling of the artery), thin sections; it helps in understanding the contribution of ICA and posterior circulation to the aneurysm (arrows) and the flow into the superior cerebellar arteries. The dashed arrows point to the wall of the thrombosed aneurysm.
To see how to make fusions, go to Philips AVM Fusions Embo and GK Targeting Page
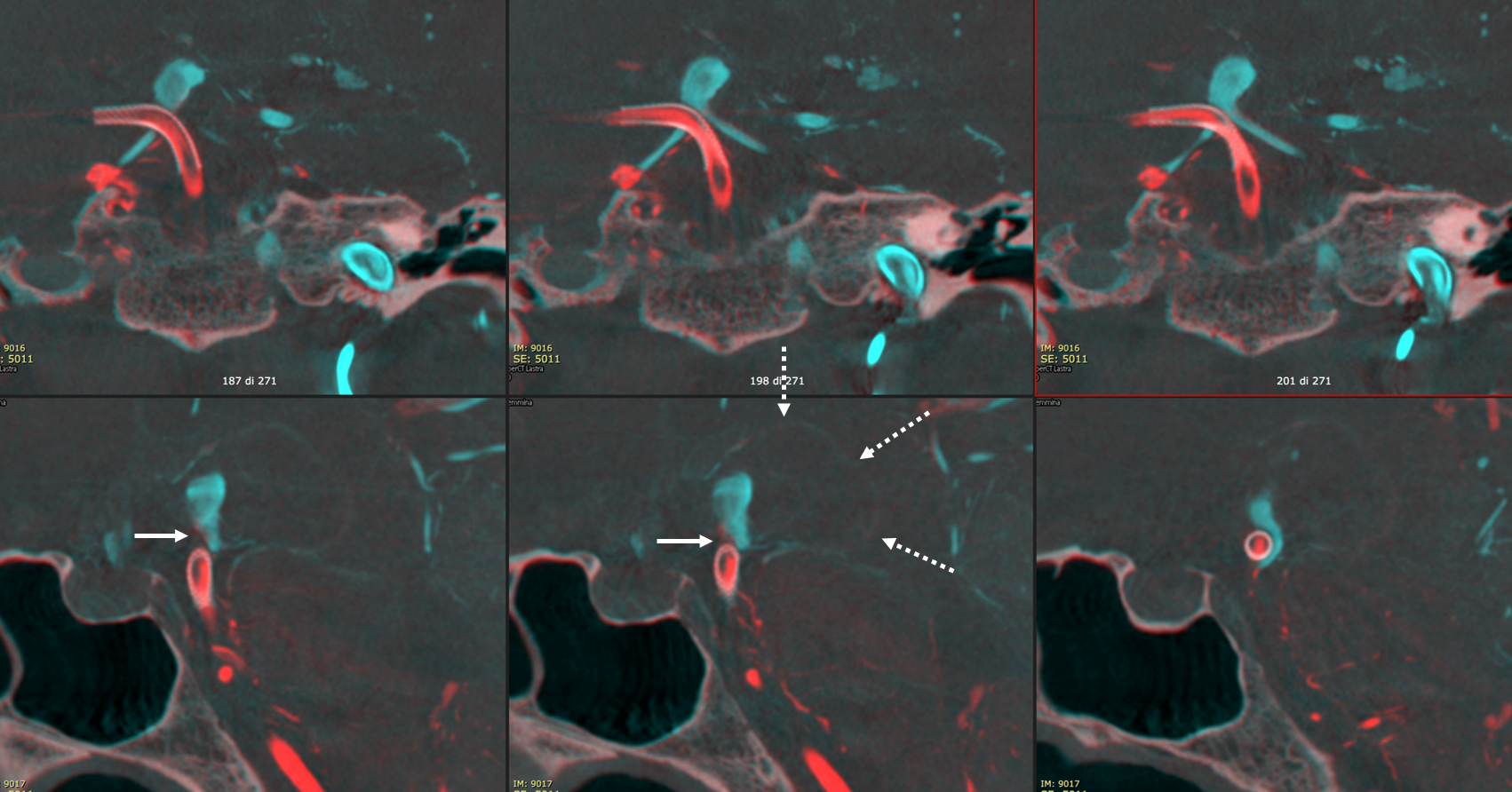
Thick MIP reconstructions of the previous fusion
Video
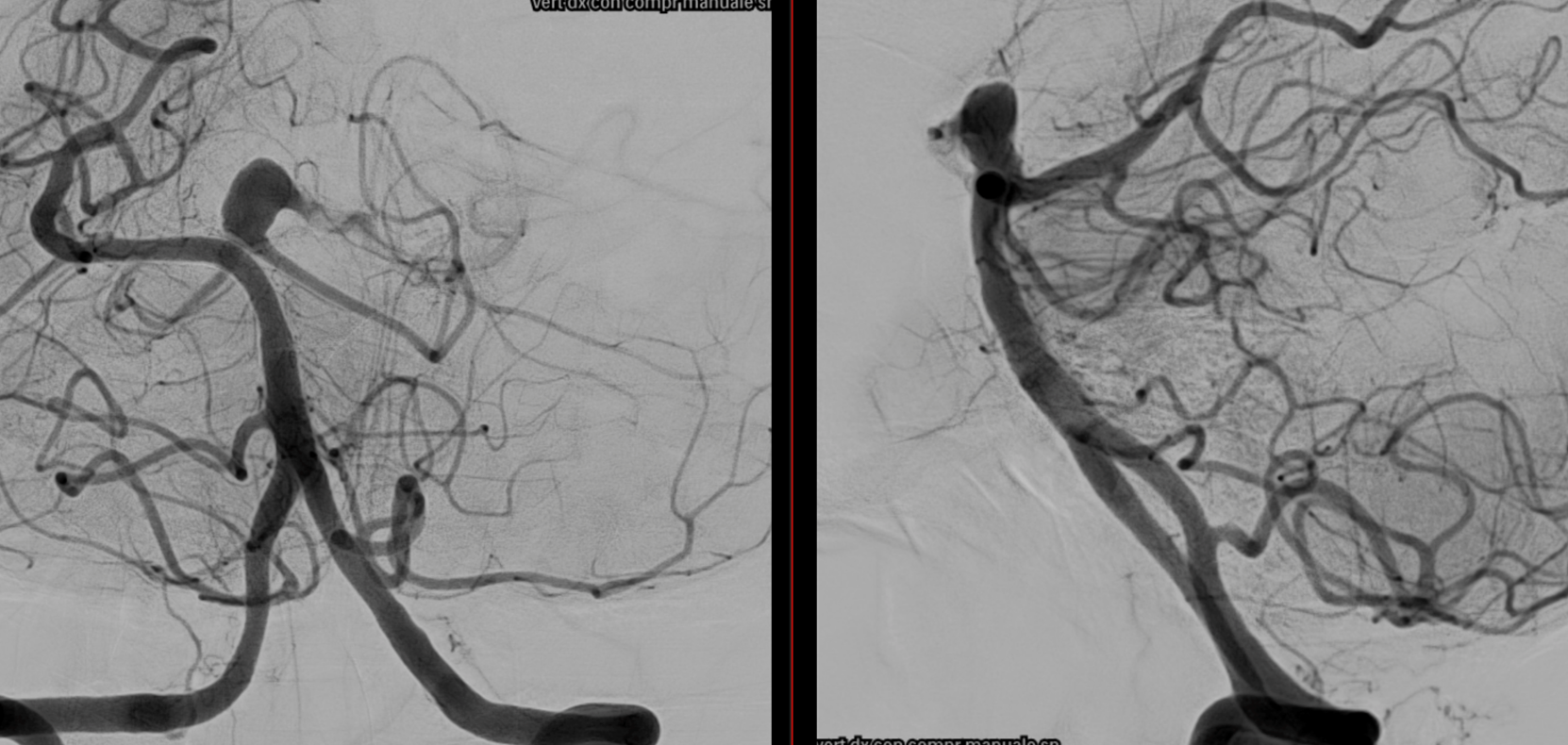
What to do? Treatment must control both SCA outflow…
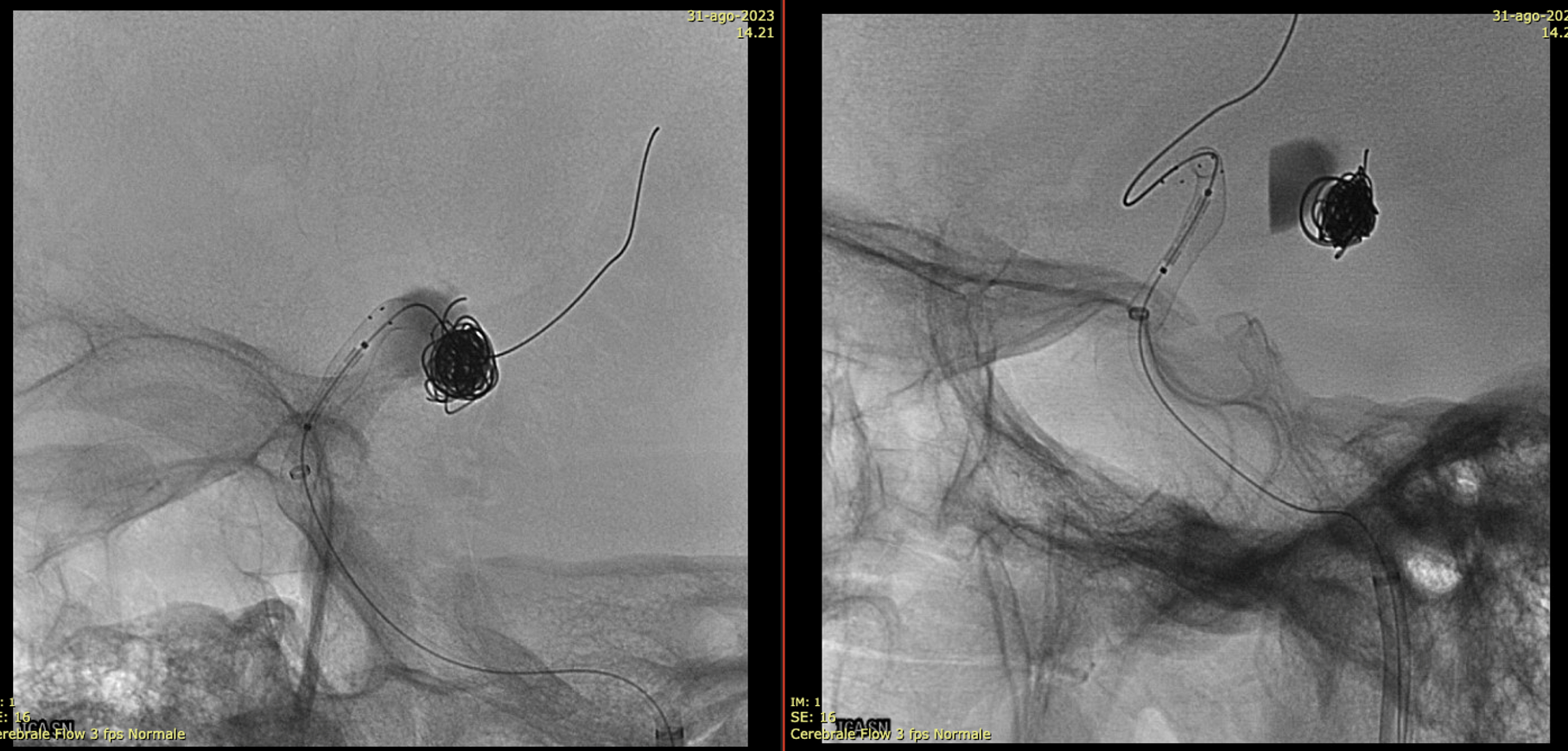
Noncontrast / dry Vaso-CT, 22 cm FOV 20 seconds acquisition, followed by a secondary reconstruction with 50% FOV and 5123 resolution; Thick MIP.
Two Lvis EVO have been used (in inverse Y or ? lambda shape). The first from the left PCom into the left SCA. The second from the left PCom into the right SCA. Another microcatheter in jailed in the aneurysm for the subsequent coiling.
There are no labels or arrows on any of the devices. If you are not sure what is going on, we suggest studying the images until you do.
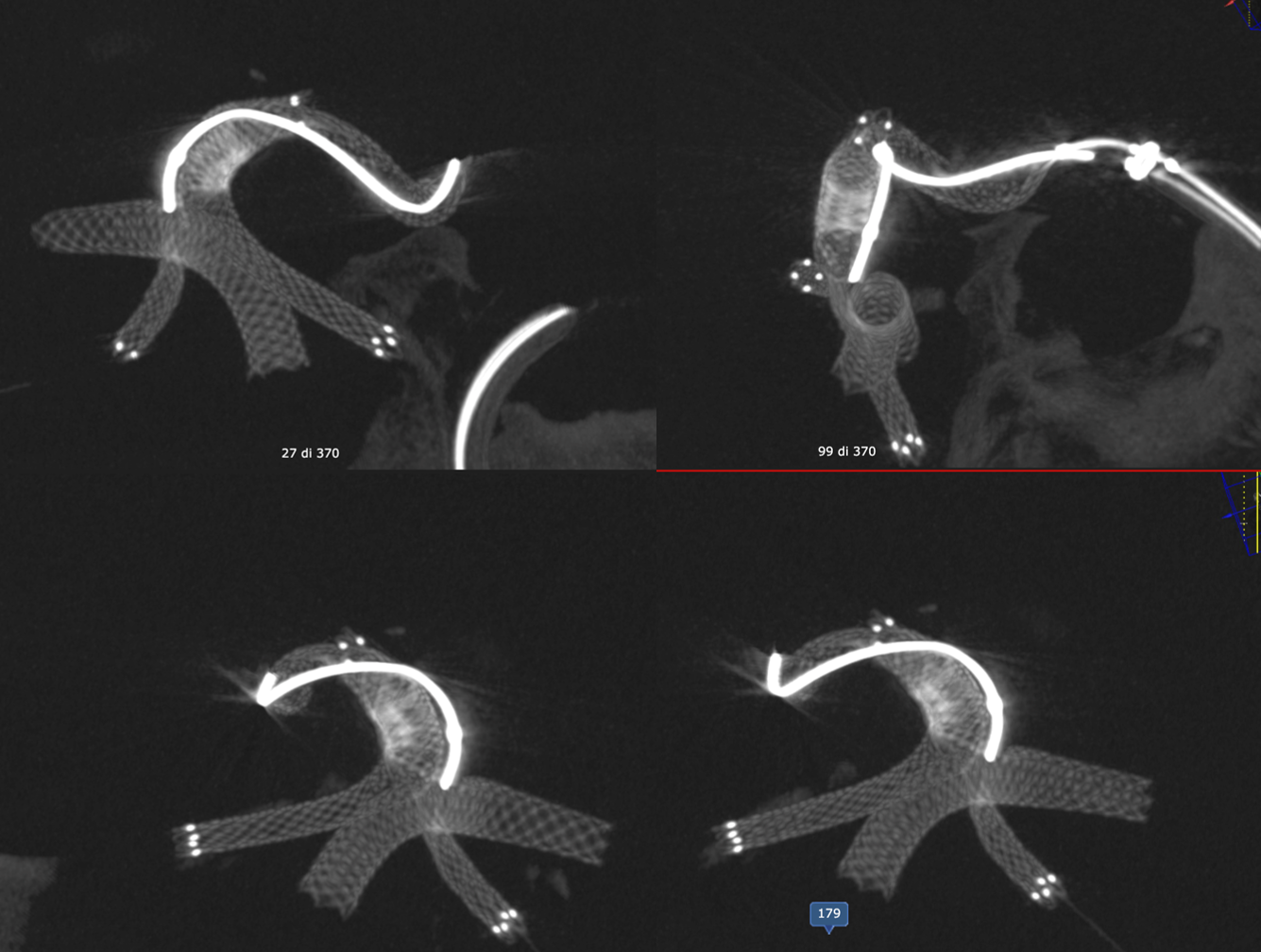
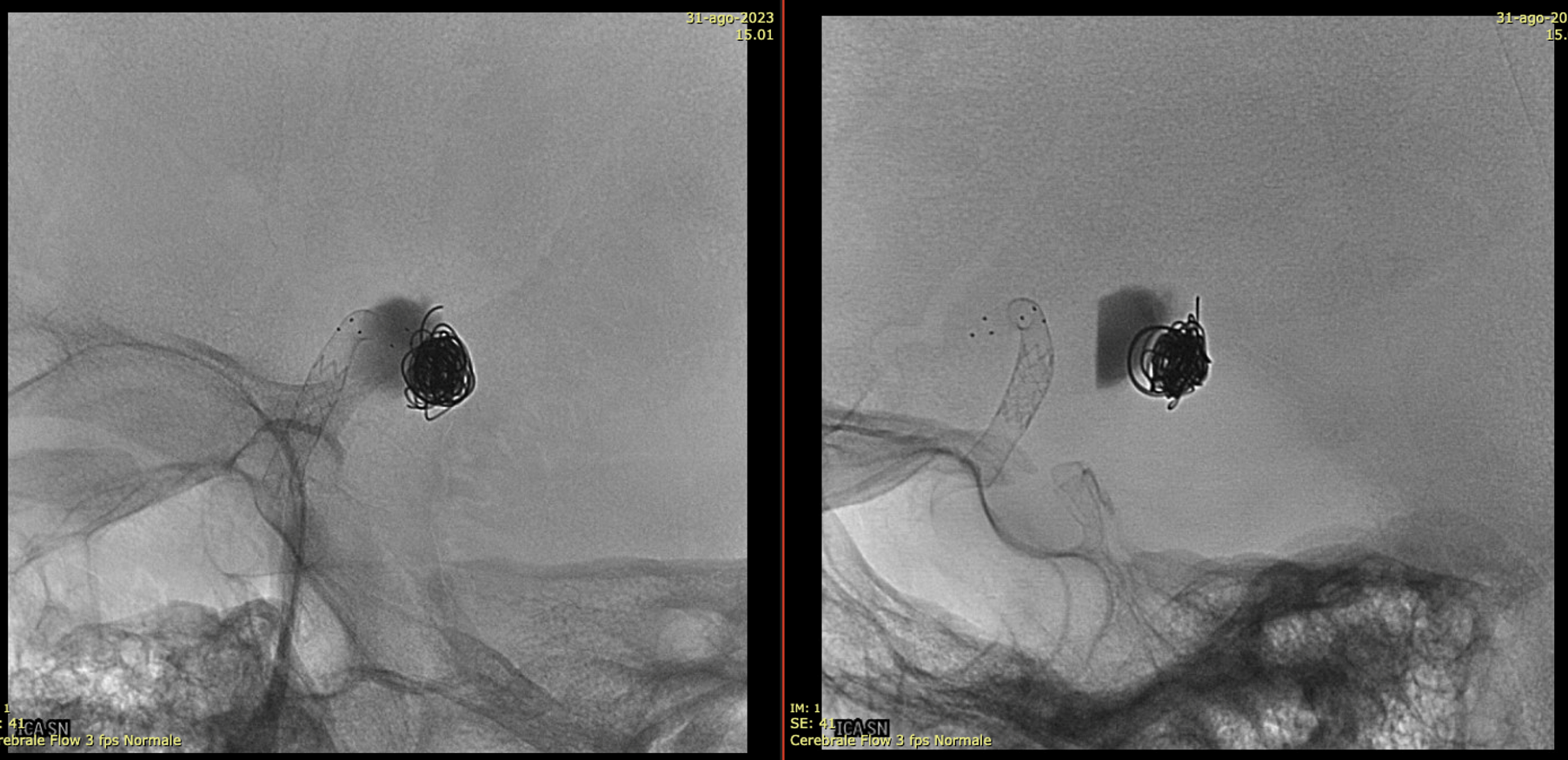
Thick MIP reconstruction of a Vaso-CT acquired with manual injection of right vert and left ICA at the same time. Vaso-CT, 22 cm FOV 20 seconds acquisition, followed by a secondary reconstruction with 67% FOV and 5123 resolution; Thick MIP.

The procedure finished with coiling of the basilar tip around the stents and PTA of right SCA stent at the crossing of the other stent
Vas is das? You figure it out…
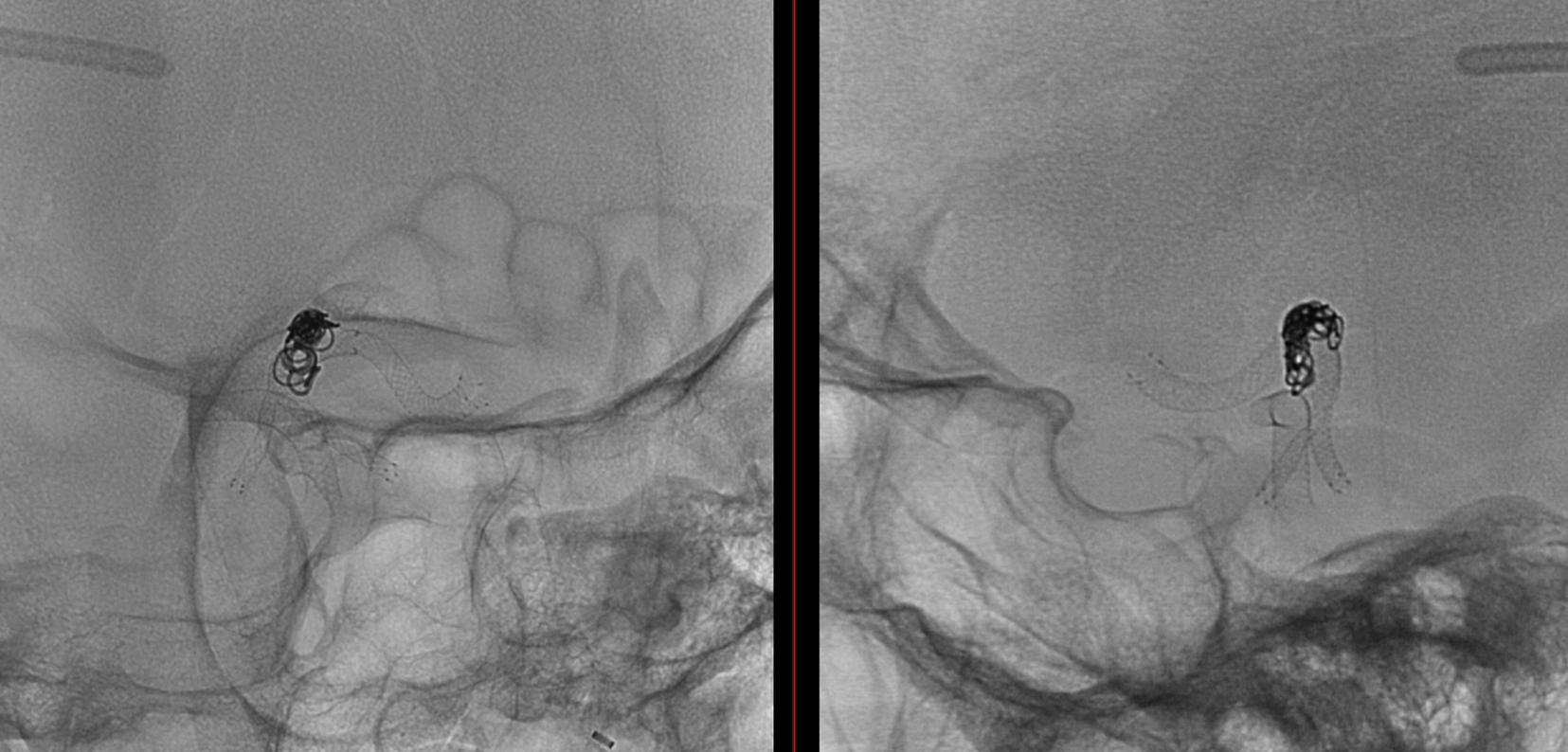
Post Rx. The key to this procedure, other than sophisticated understanding of the problem and the materials to be used, is a consistently effective antiplatelet state. Doing this without IIbIIIa in the lab for example risks major disaster.

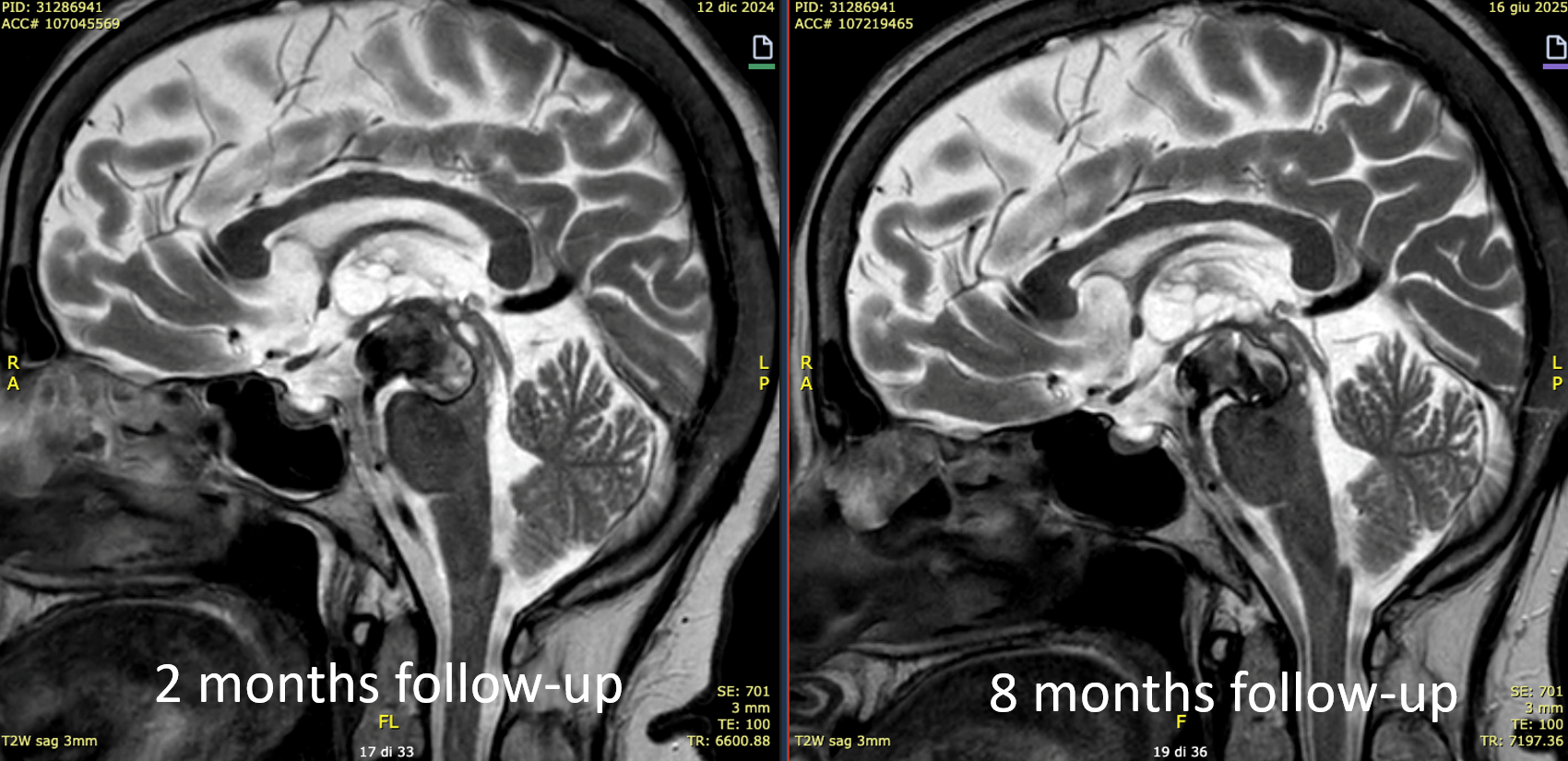
At the 8 months follow-up, after passing from DAPT to SAPT, the aneurysm became smaller, with corresponding clinical improvement.
This is a key point — the success of treatment in aneurysms of this type is judged by cross-sectional imaging, not angio. With aneurysm shrinkage a good angiogram is guaranteed, while there are many examples of good-looking angiograms with moribund patients.
For more of this, check out Case Archives section on Aggressive Aneurysms — the point being that aggressive aneurysms require aggressive solutions.
