Inferolateral Trunk (ILT):
The ILT arises as a single trunk or a collection of vessels from the lateral aspect of the horizontal cavernous carotid artery segment. It usually supplies adjacent dura and cranial nerves, and has extensive anastomoses with branches of the IMAX, middle and accessory meningeal arteries, ophthalmic arteries and the nearby MHT. Embryologically it can be considered as a remnant of the primitive dorsal ophthalmic artery (allowing for much debate in this neck of woods). The ILT and adult ophthalmic arteries are primary routes of ICA reconstitution following proximal ICA occlusion. The importance of understanding ECA-ICA collaterals of the ILT is paramount.
It is paramount to see vessels as part of a network, not isolated entities. This is the big picture of neuroangio. There is tremendous variability in size of ILT and everything else, the extent of territory it supplies etc — reflecting balance with neighboring territories. Often, the same connection seen from different vessels has different names. The spinosum branch of ILT and cavernous branch of MMA are the same vessel/network. Either end may be dominant, but all are part of a whole.
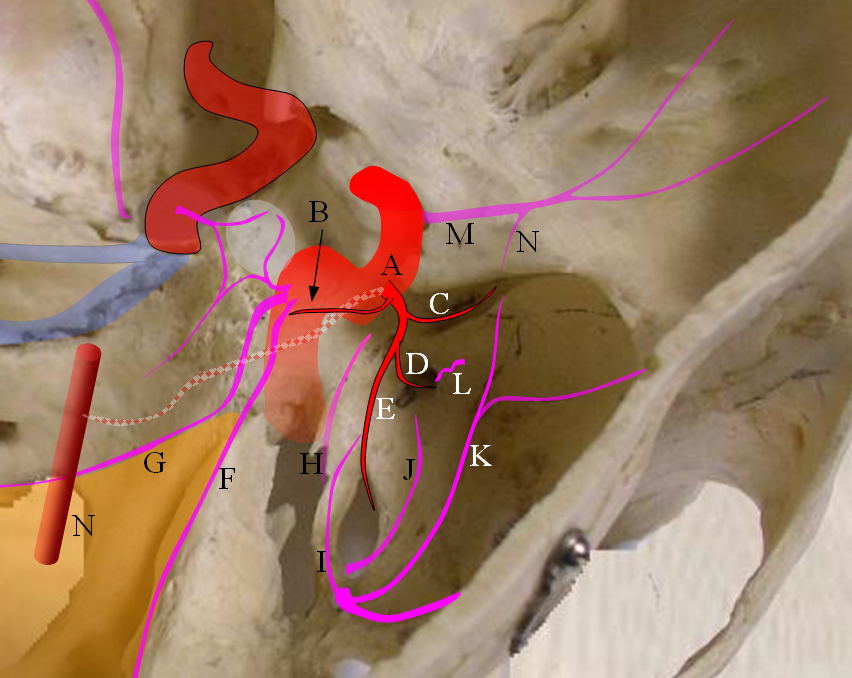
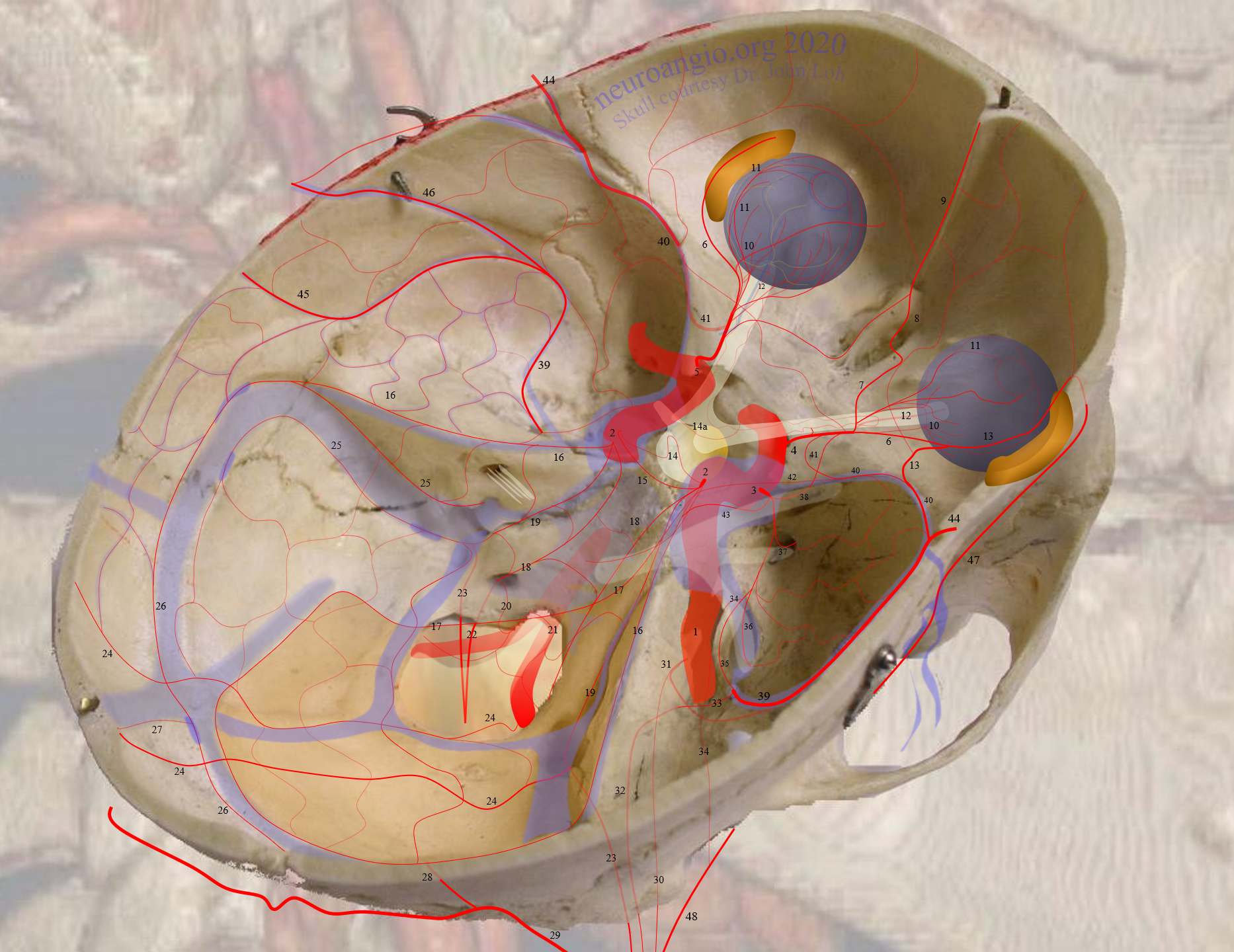
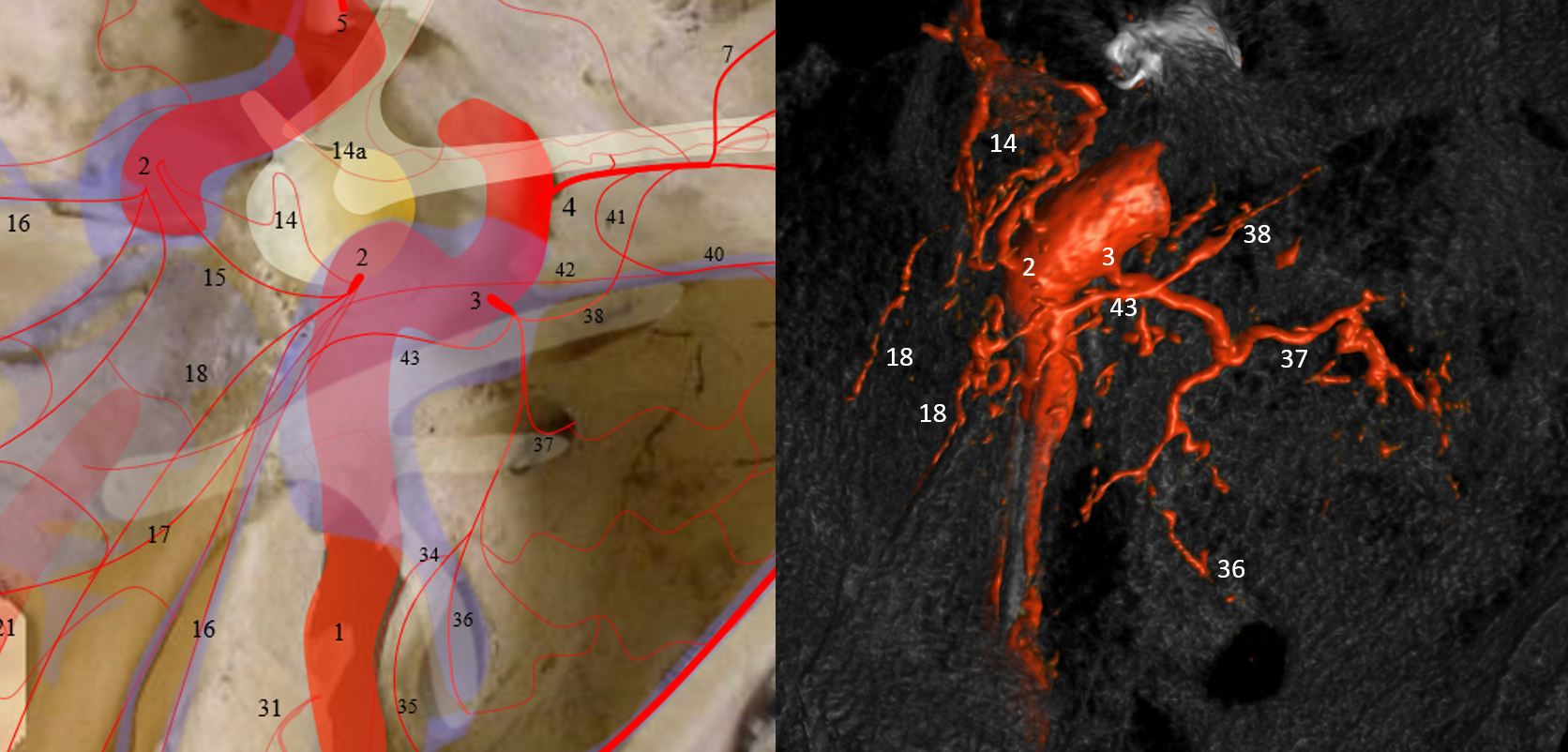
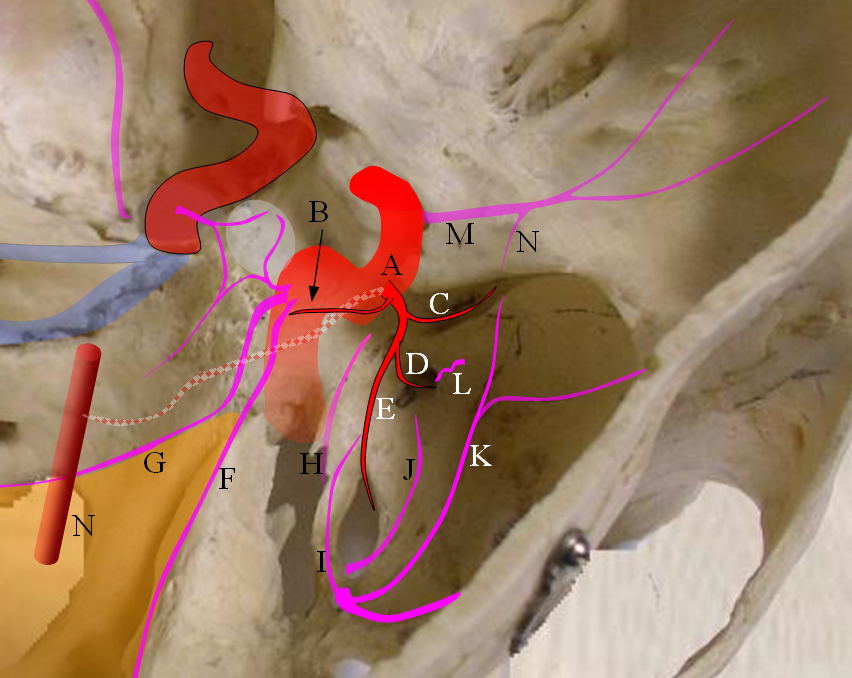
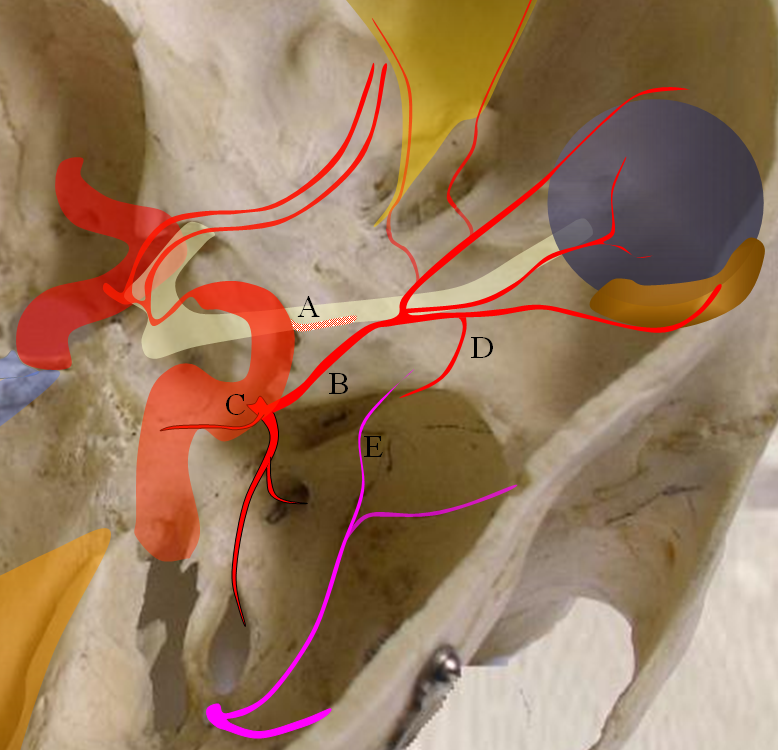
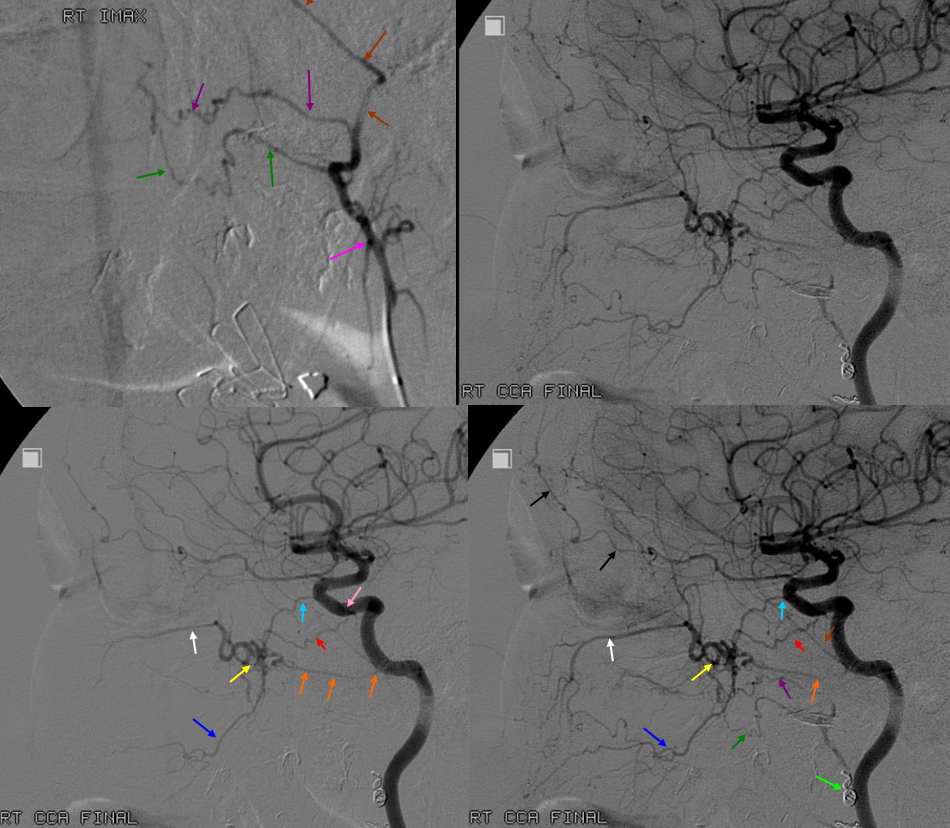
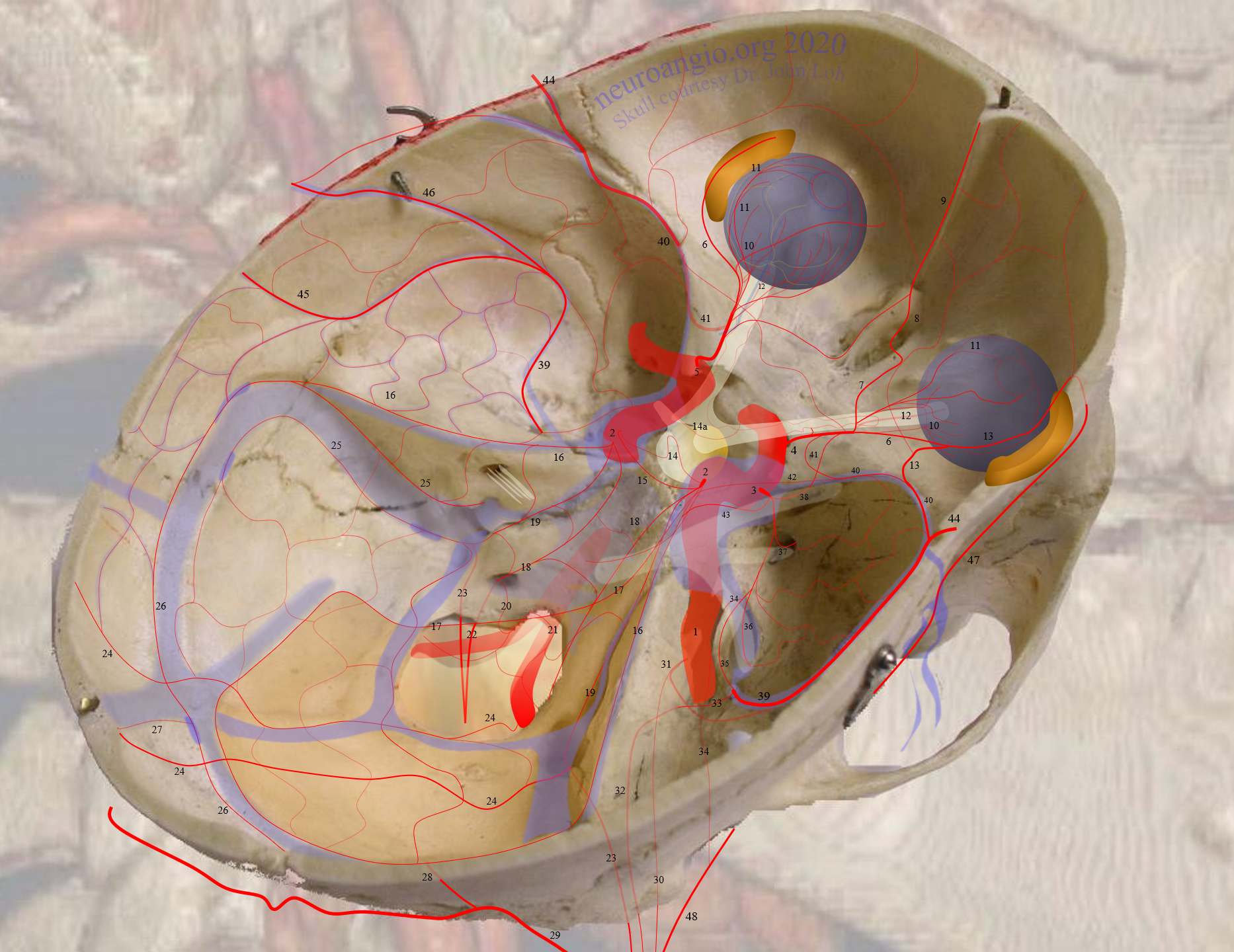
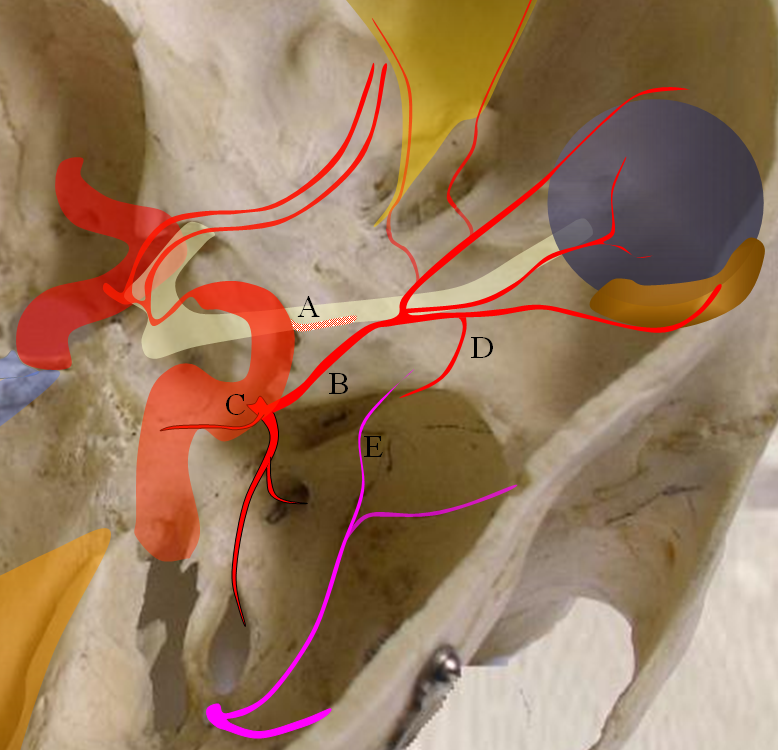
Figure 1: ILT and important anastomoses:
A) ILT
B) Recurrent branch of the ILT — courses along CN IV, and collateralizes with branches of the MHT. Not rarely it annexes the territory of marginal tentorial (G) or lateral tentorial (F) arteries which more commonly come off the ILT (see ILT).
C) Anteromedial branch — a very important branch, this is a vestige of the primitive dorsal ophthalmic artery which in very early embryonic life supplied the orbit together with primitive ventral ophthalmic artery. This artery is hemodynamic balance with the recurrent meningeal branch (N) of the ophthalmic artery (M). Very rarely, when proximal ophthalmic (M) is absent, this branch (C) can reconstitute the ophthalmic artery (see ophthalmic artery section), although more commonly the middle meningeal artery fulfills this role through its ophthalmic branch (K)
D) Artery to the foramen rotundum — another very important vessel supplying the nerve of the same foramen. It collateralizes with foramen rotundum branch of the IMAX (L), and is the primary route of ICA reconstitution via the IMAX
E) Foramen ovale branch — yet another important branch which supplies the appropriate foramen ovale nerve and collateralizes with the accessory meningeal artery (J) and also with carotid branch of the ascending pharyngeal artery (H) coming up through foramen ovale and cavernous branch (I) of the middle meningeal artery.
The checkered vessel anastomosing with the basilar artery (N) is the trigeminal artery, which sometimes originates from the region of the ILT.
Below are some examples of normal variability in ILT branches. The numbers always refer to the key skull base figure above.
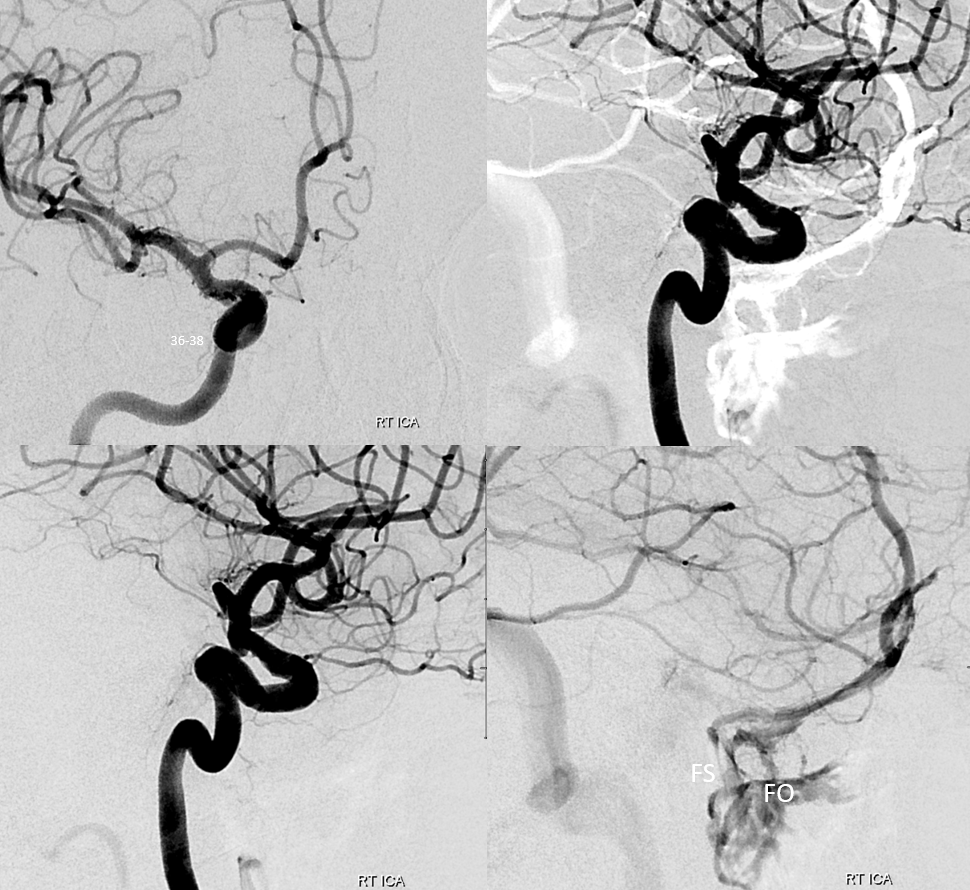
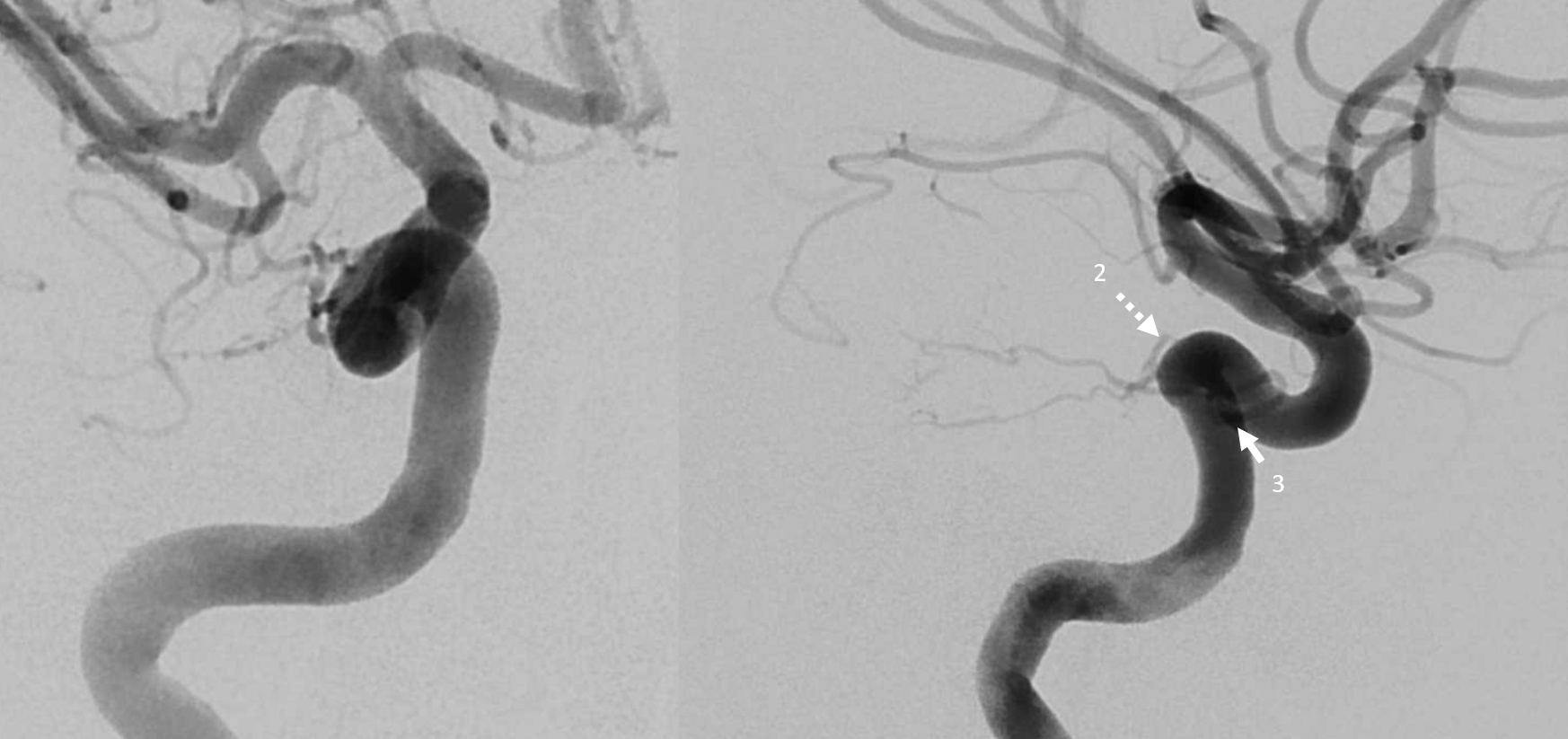
Well-seen anterolateral (38) and cavernous sinus (36) branches — going through Foramen Spinosum (FS) of ILT (3). The MHT (2) and its clival (18-19) branches are also well-seen.

How do we know its FS? Well, here is venous phase images with superficial sylvian veins draining into both Foramen Ovale (FO) and FS. Normally, this kind of drainage is into FO, but here it helps to outline FS as well.
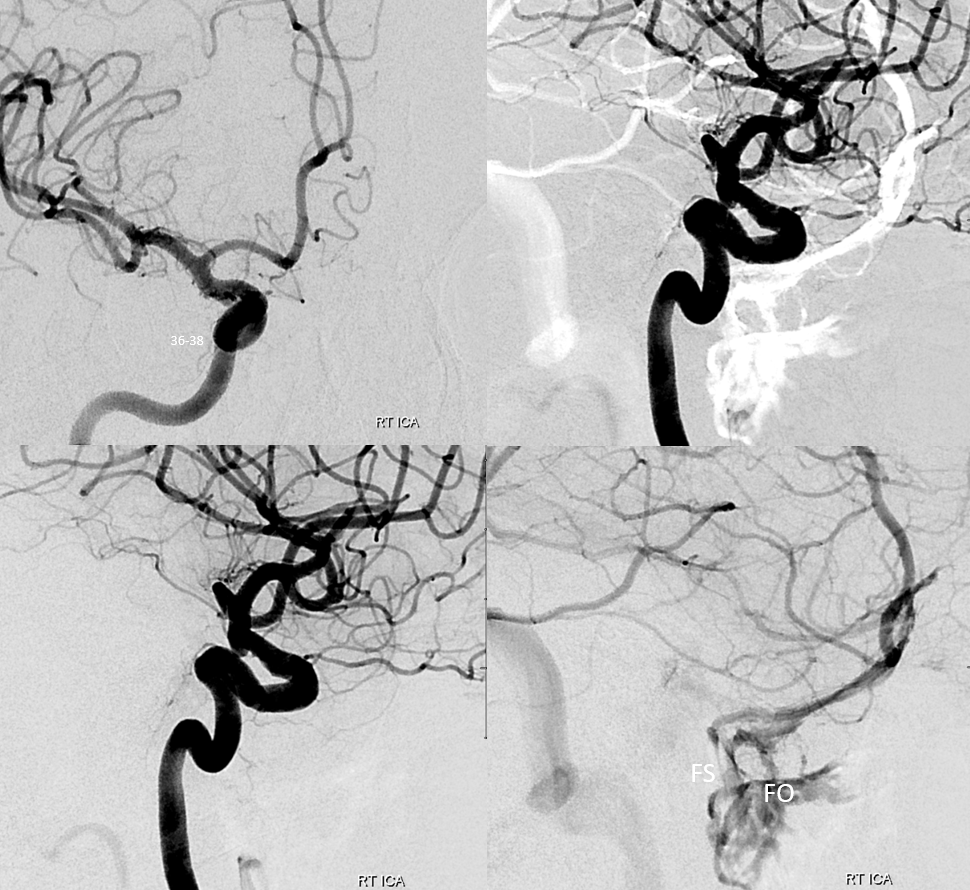
Frontal views show that this drainage is not cavernous sinus at all — it is a “paracavernous sinus” (arrows), with common carotid injection double mask image (lower right) also showing drainage into spinosum, as defined by the MMA.
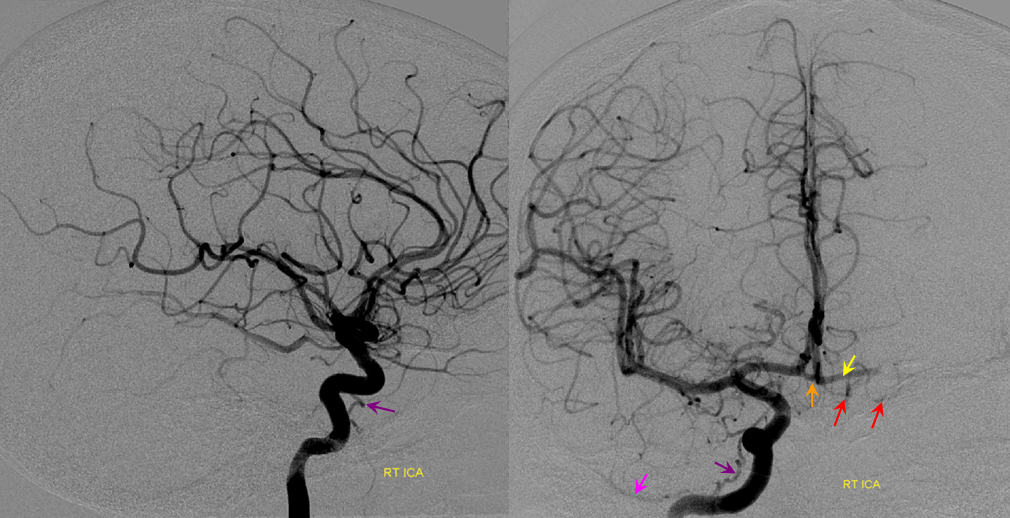
Prominent foramen ovale branch of the ILT supplies the accessory meningeal artery — again, its a network. Typically, the AMA is supplied by the IMAX and connects with ILT via foramen ovale branch — but it can occasionally be the reverse.
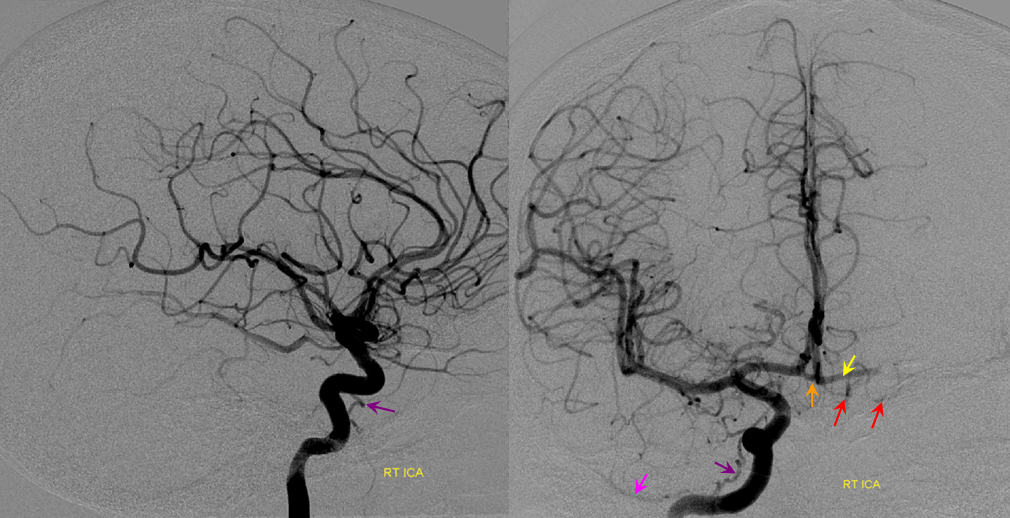
Purple=ILT; Pink=accessory meningeal reflux; orange=acom; red=left frontopolar branch; yellow=left A1
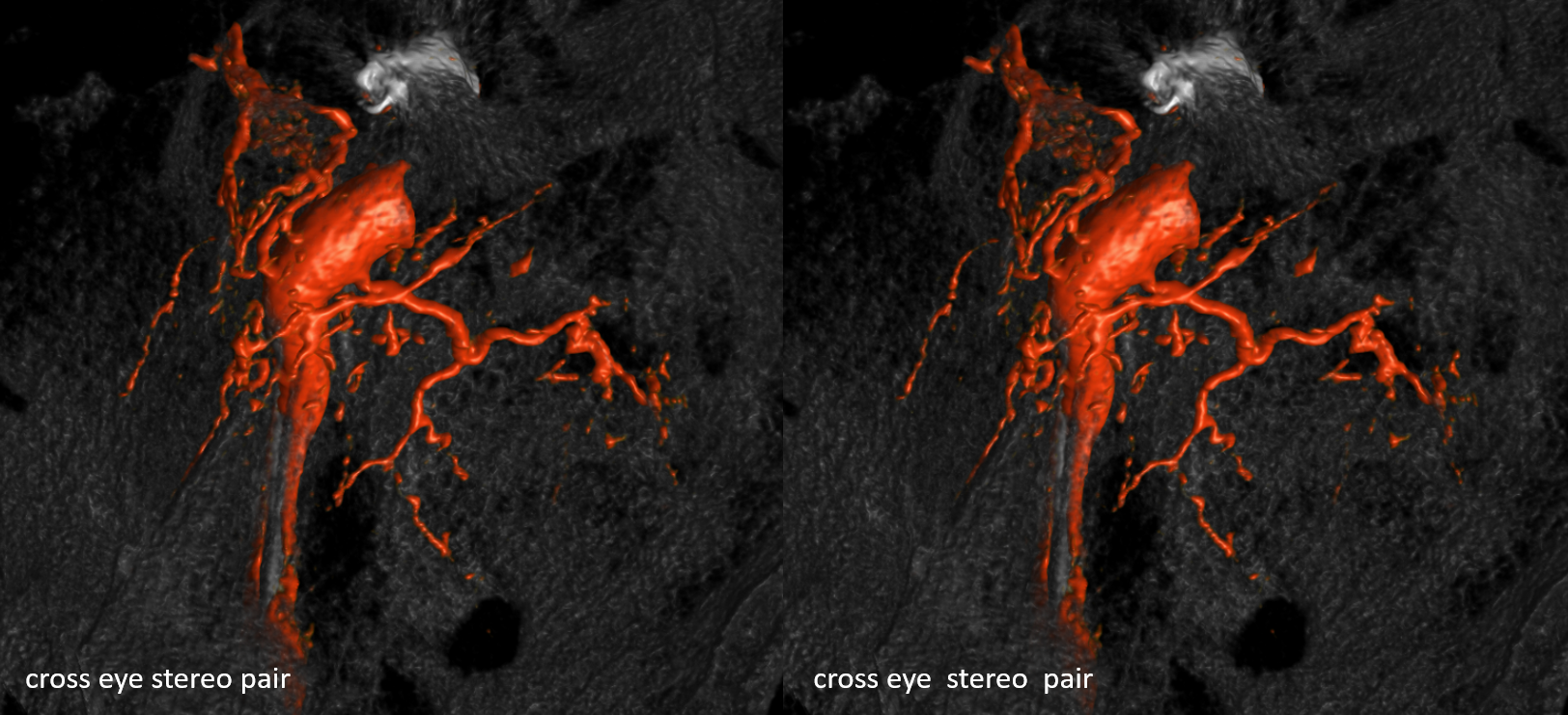
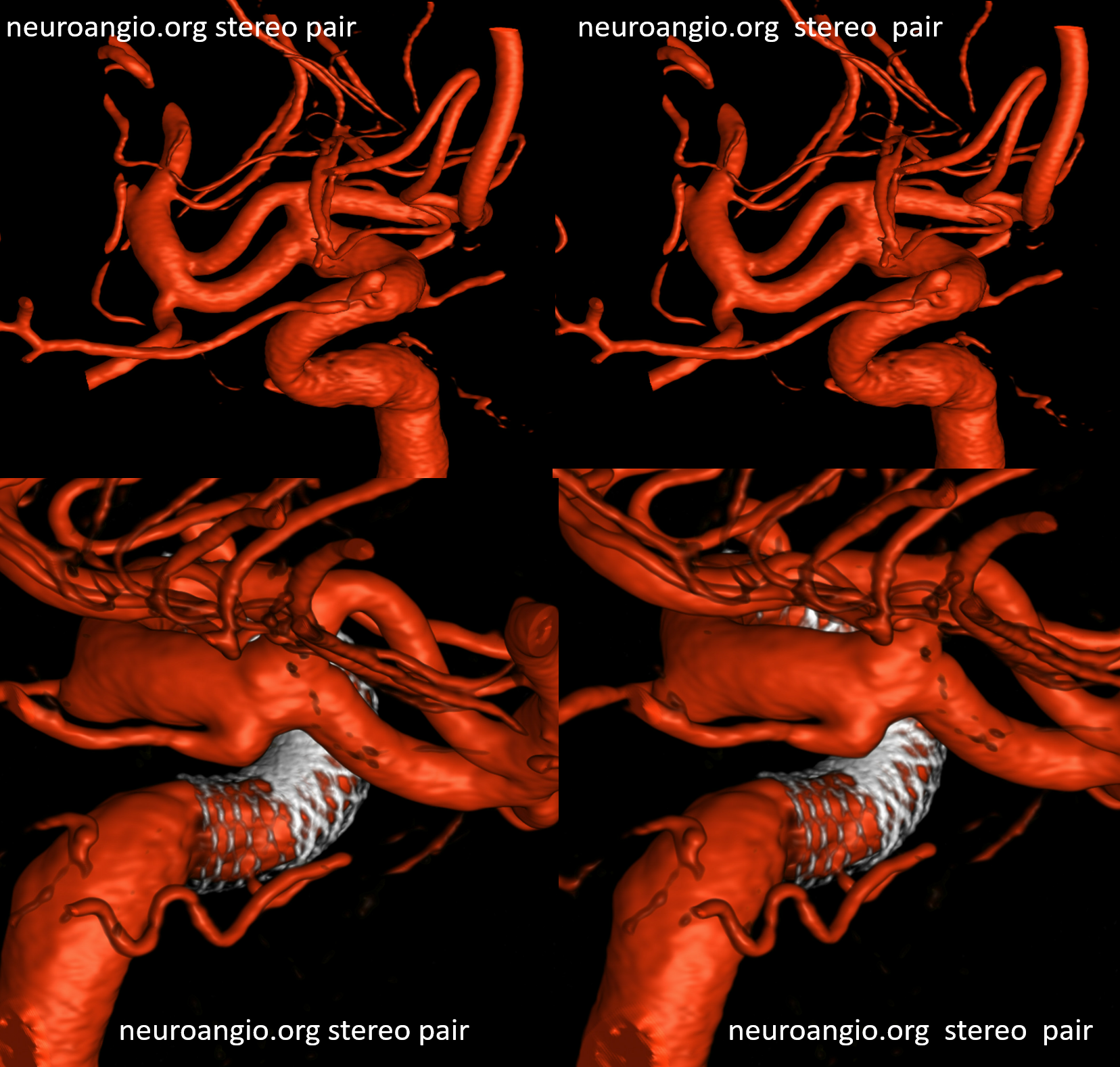
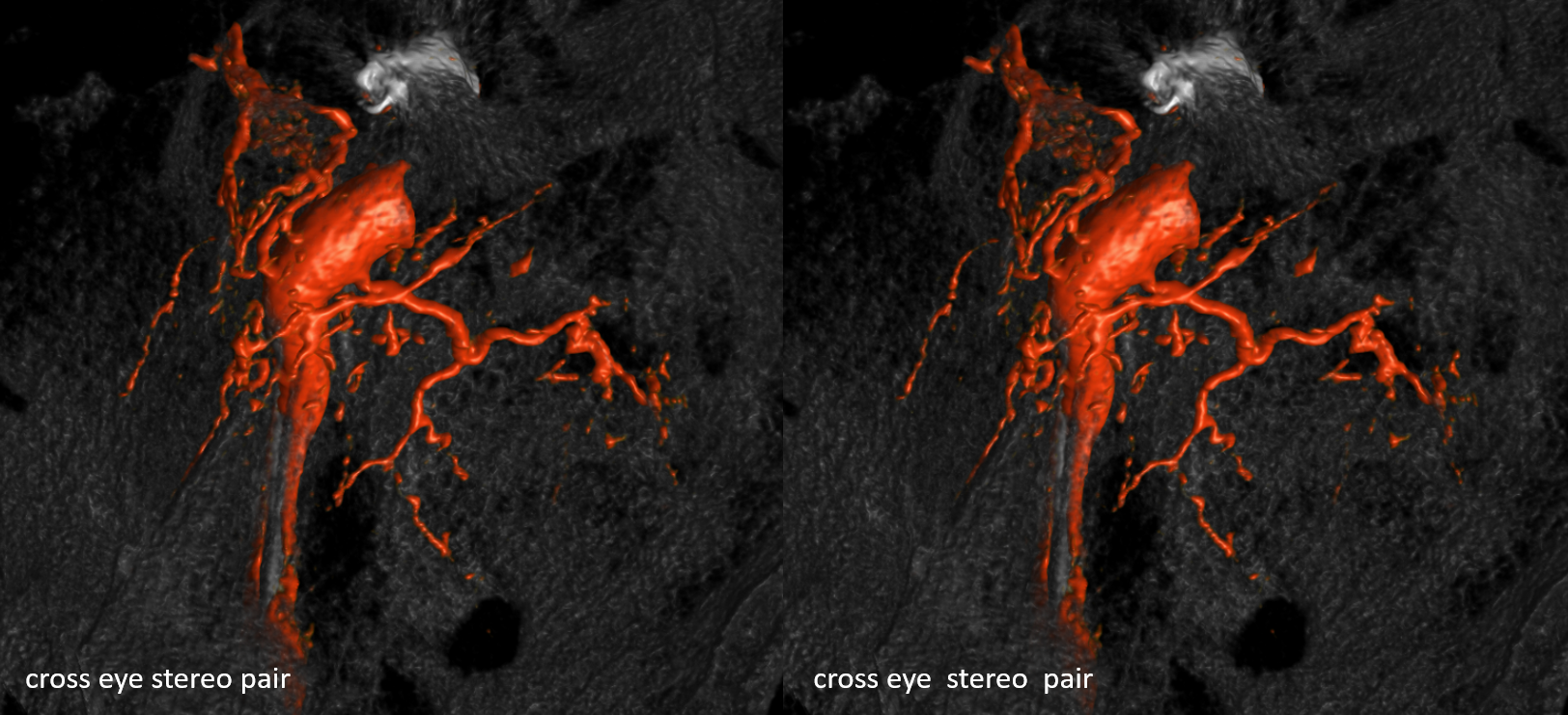
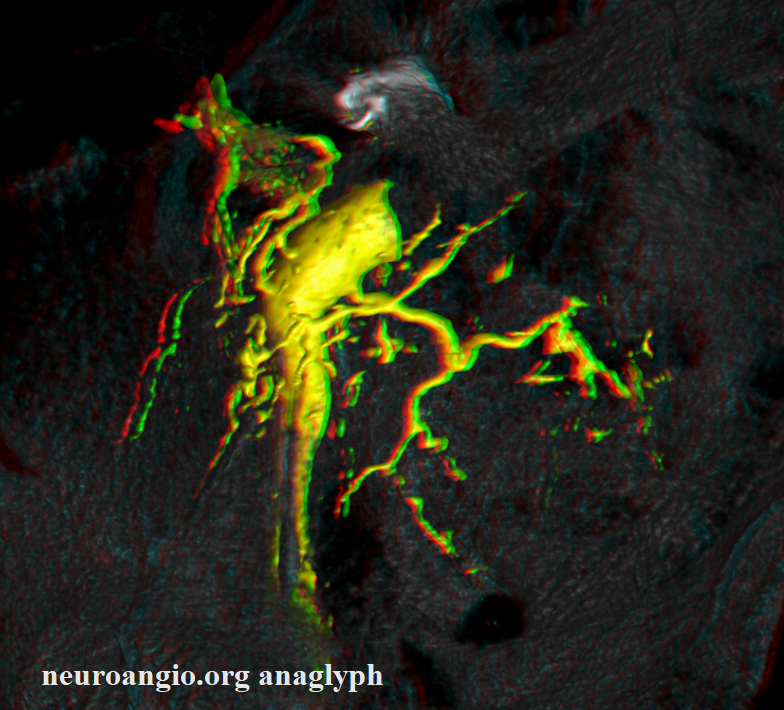
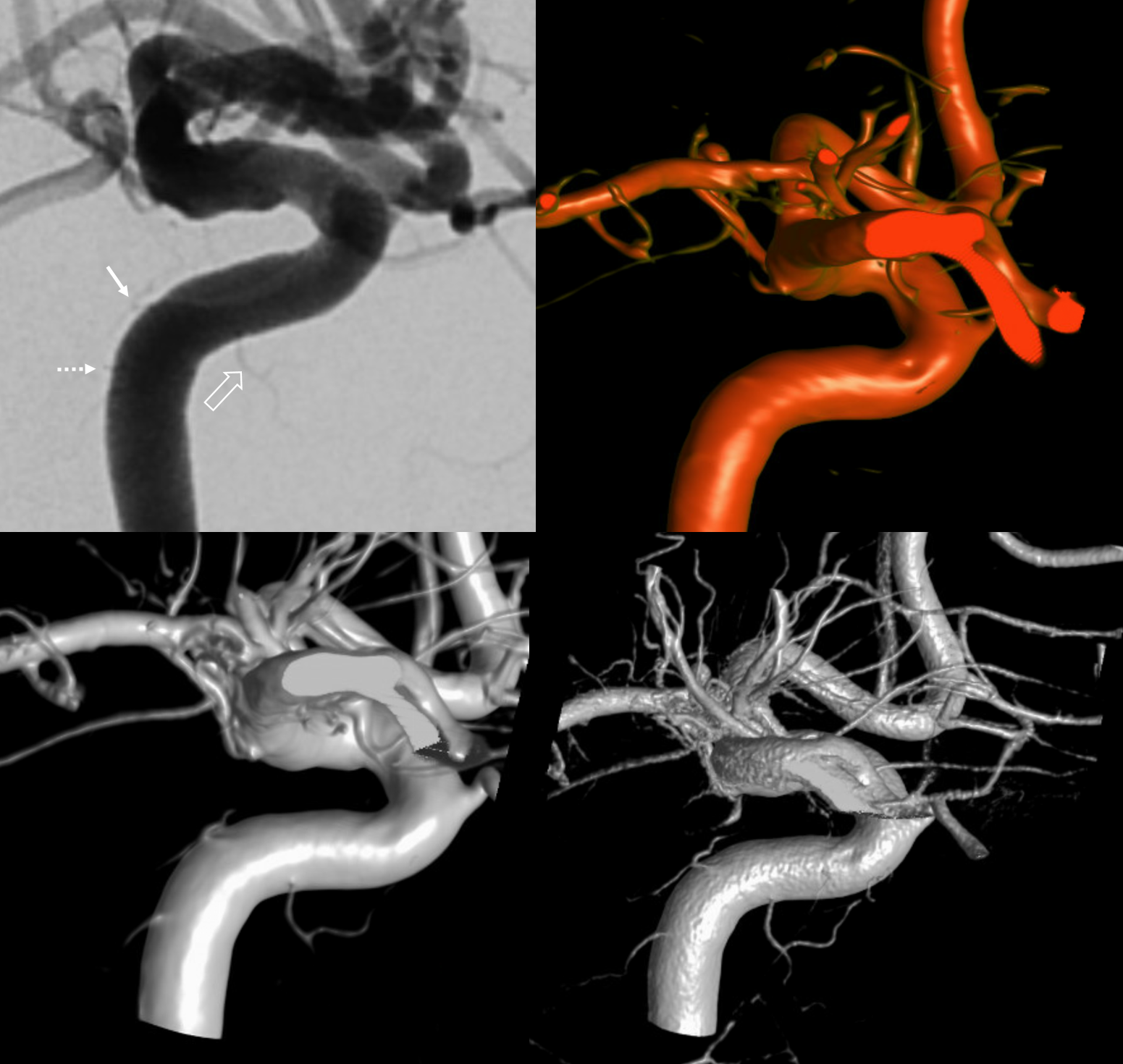
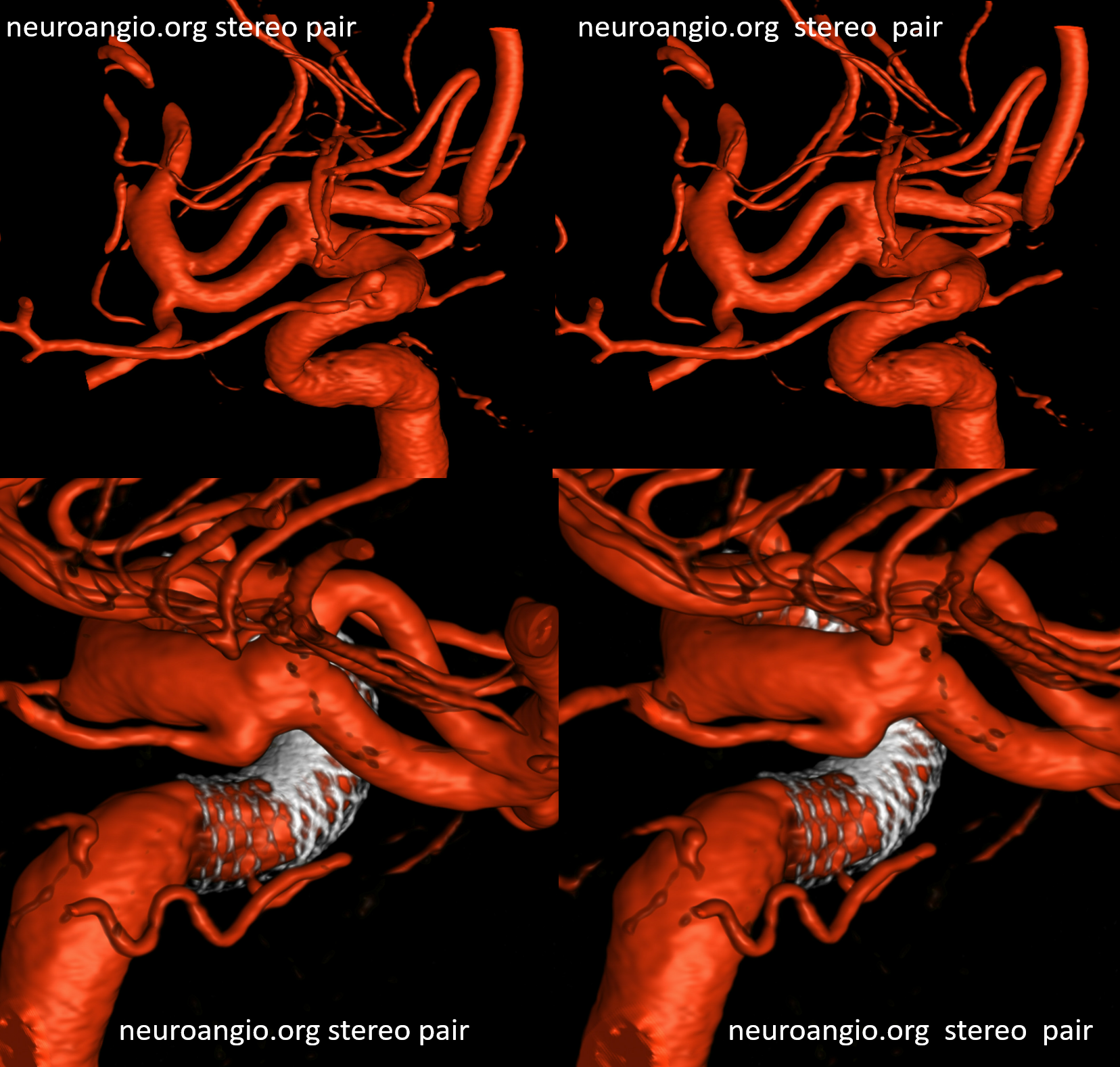
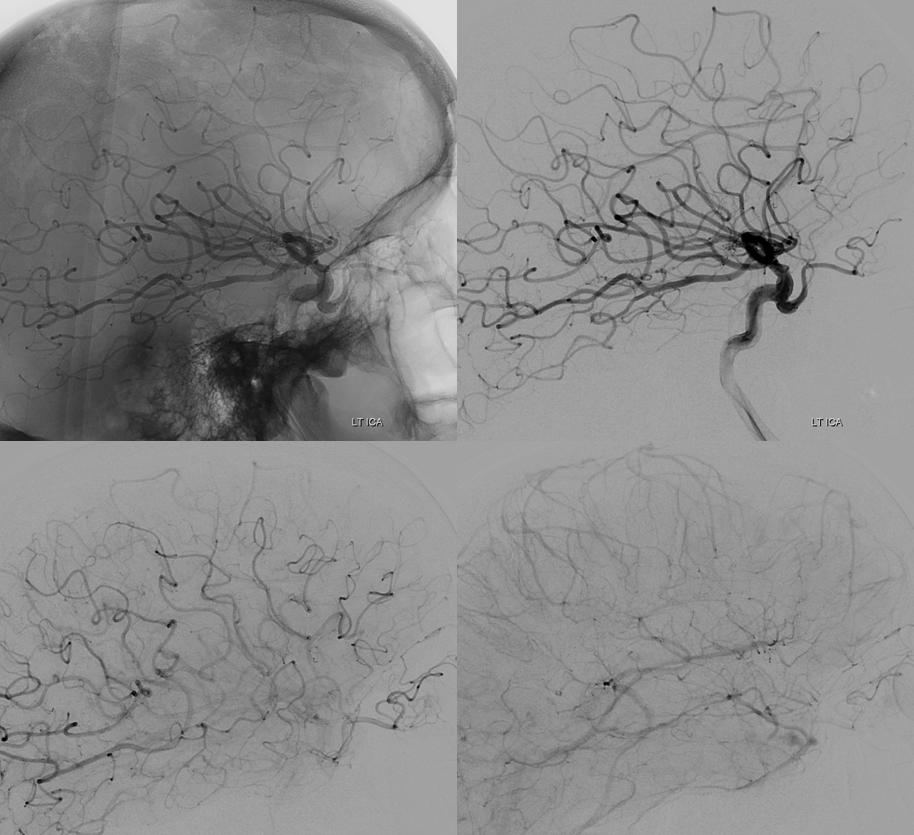
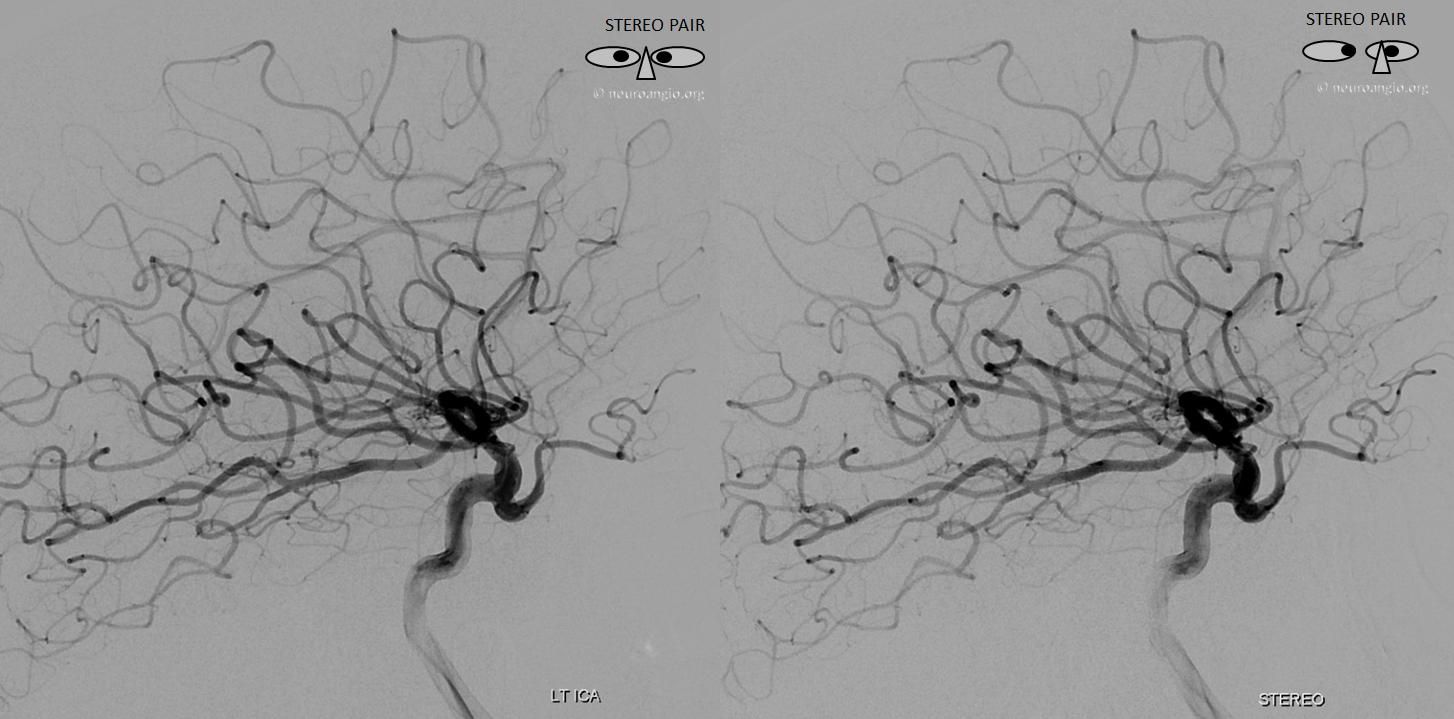
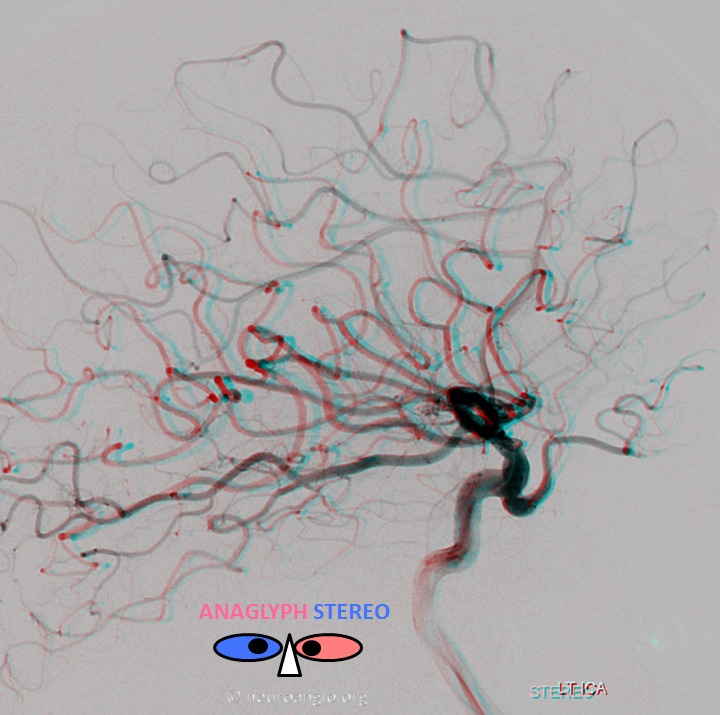
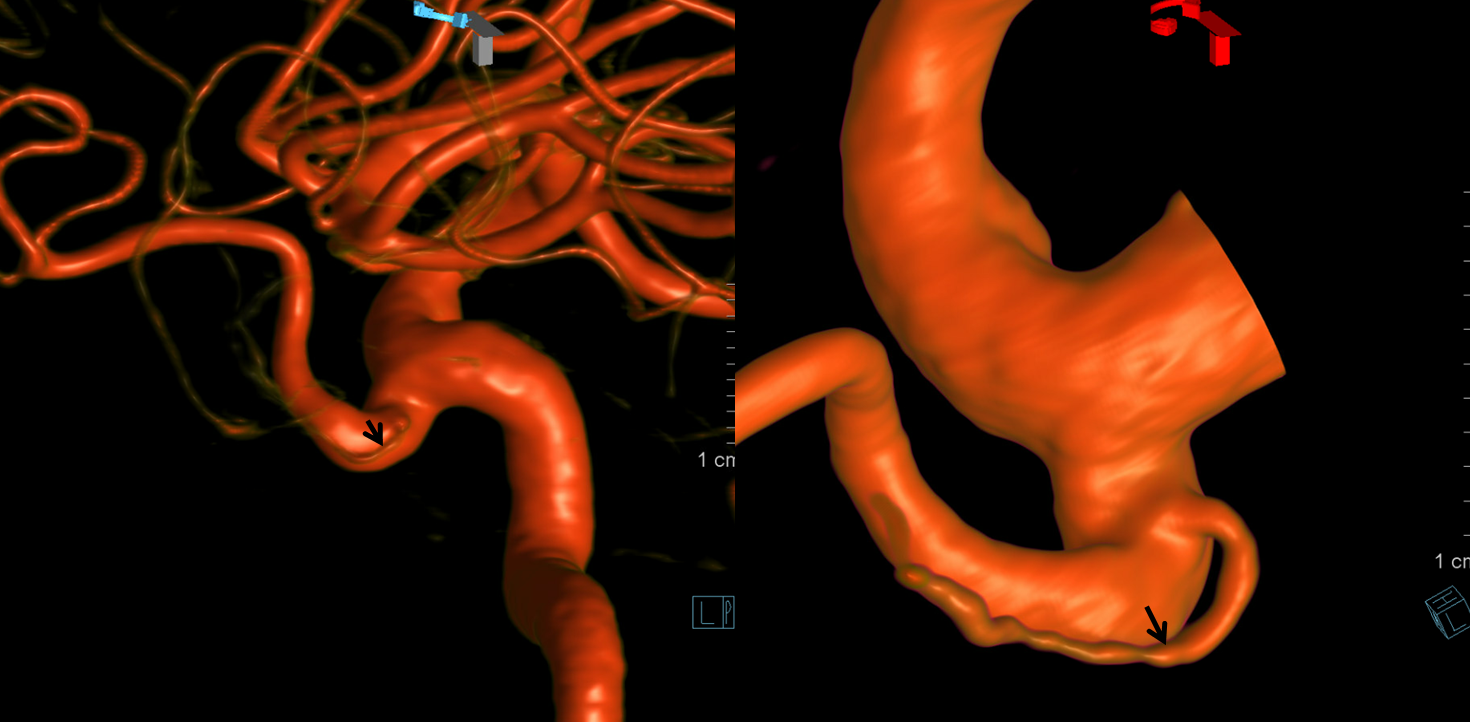
In the below case of a traumatic carotid occlusion at the clinoid segment, the blind stump of distal ICA allows for excellent visualization of MHT and ILT branches
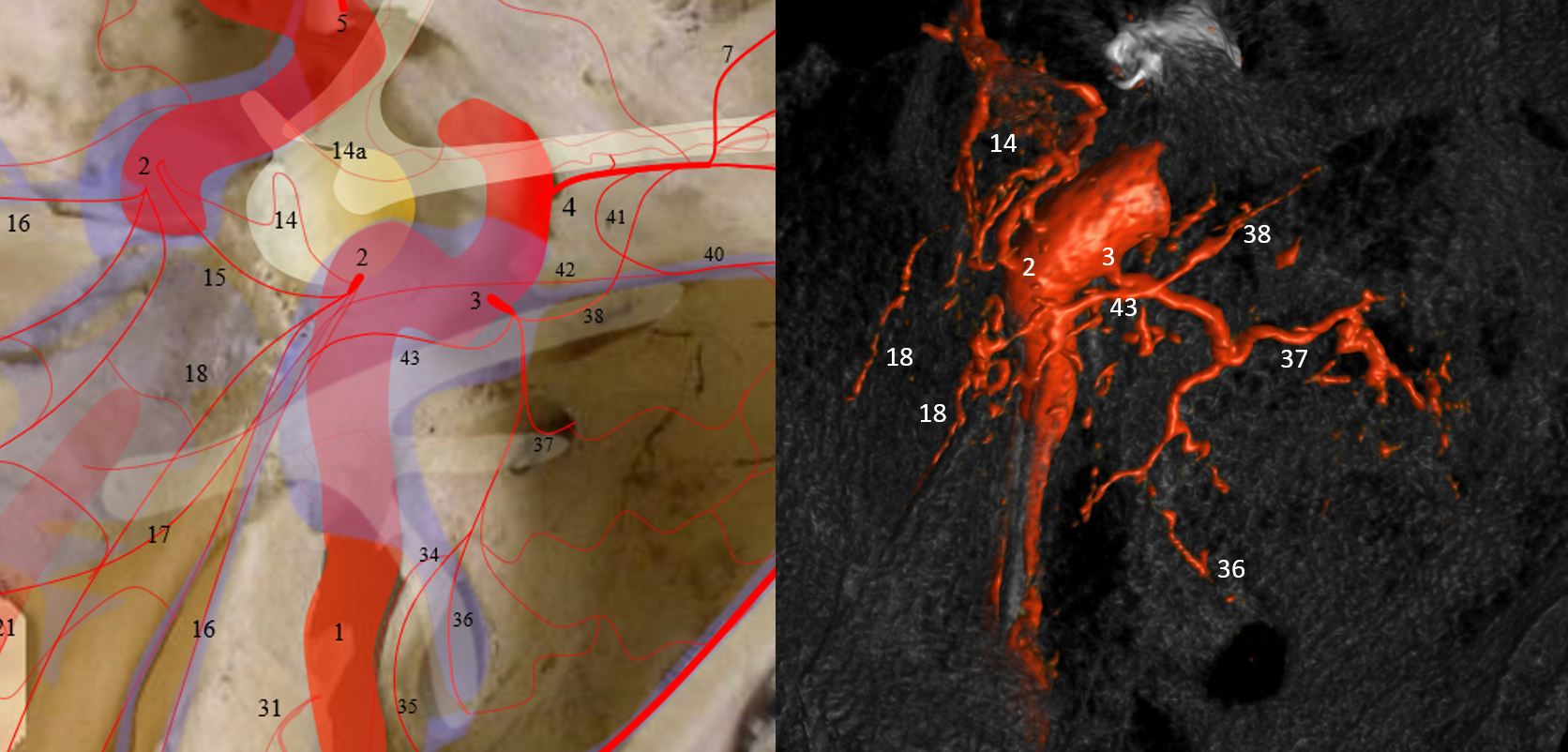
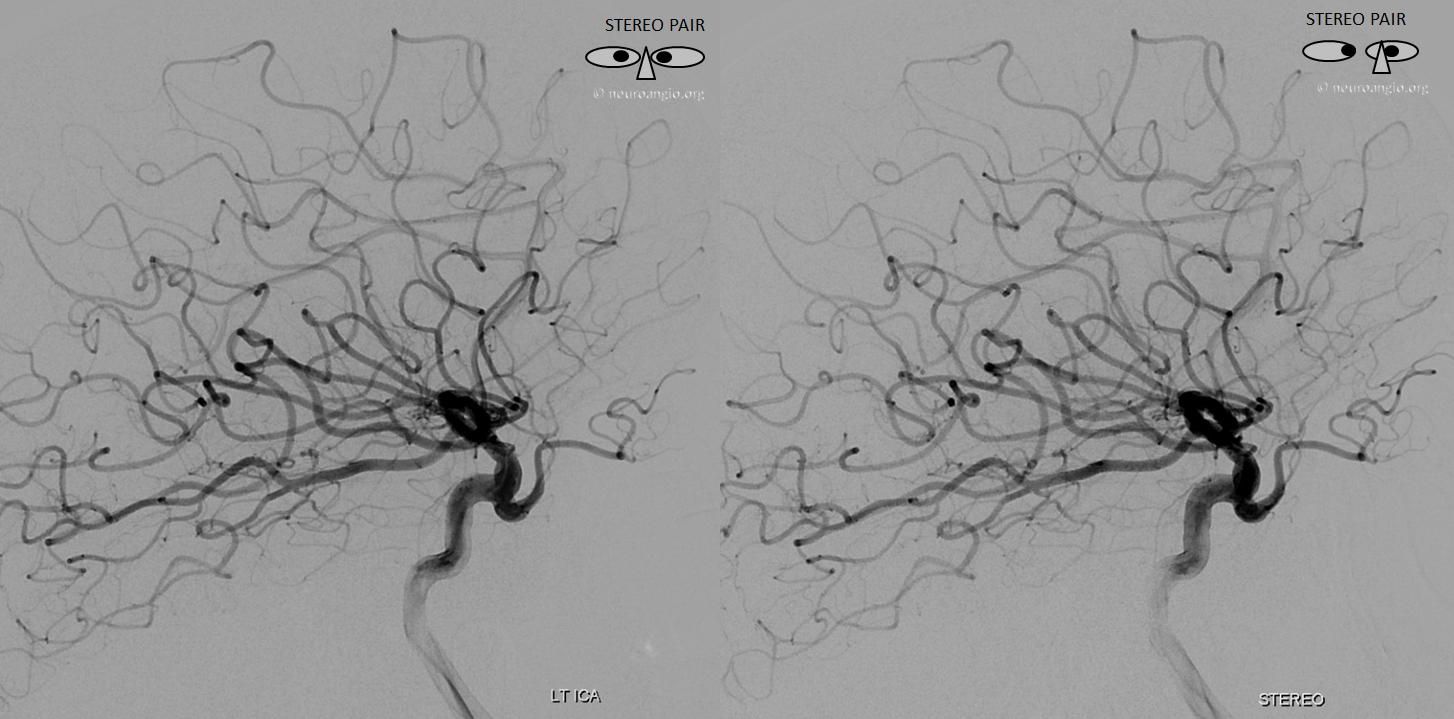
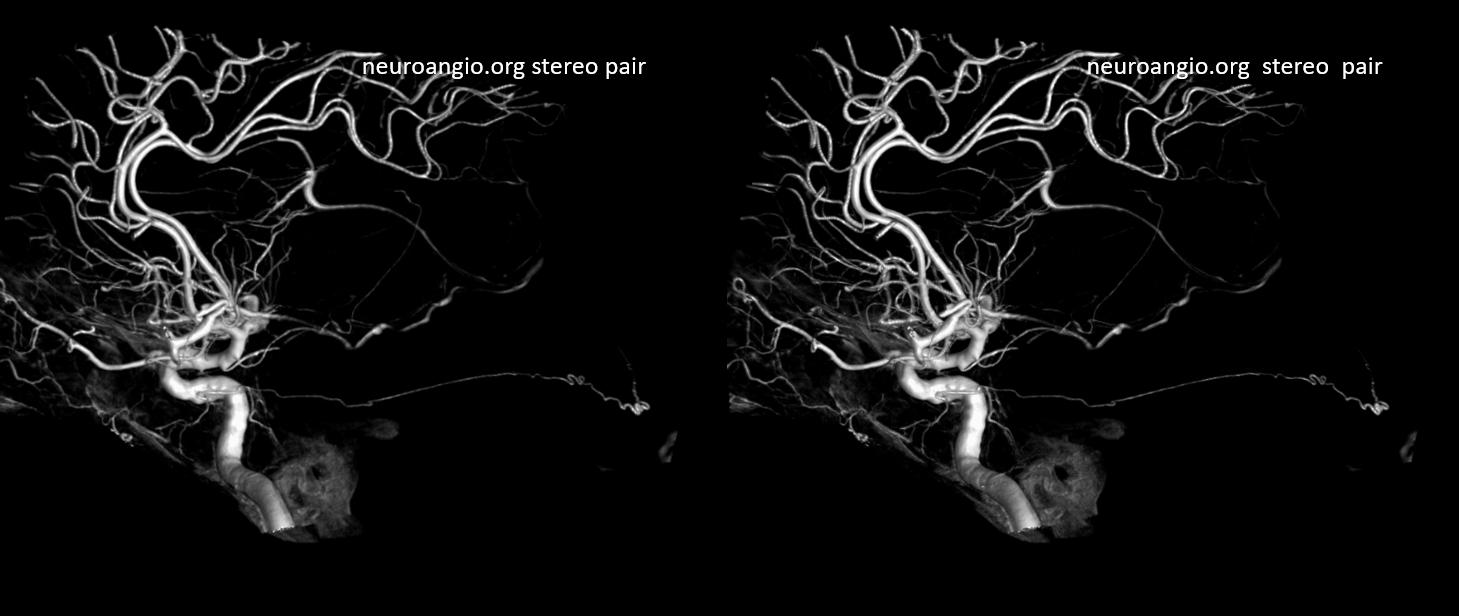
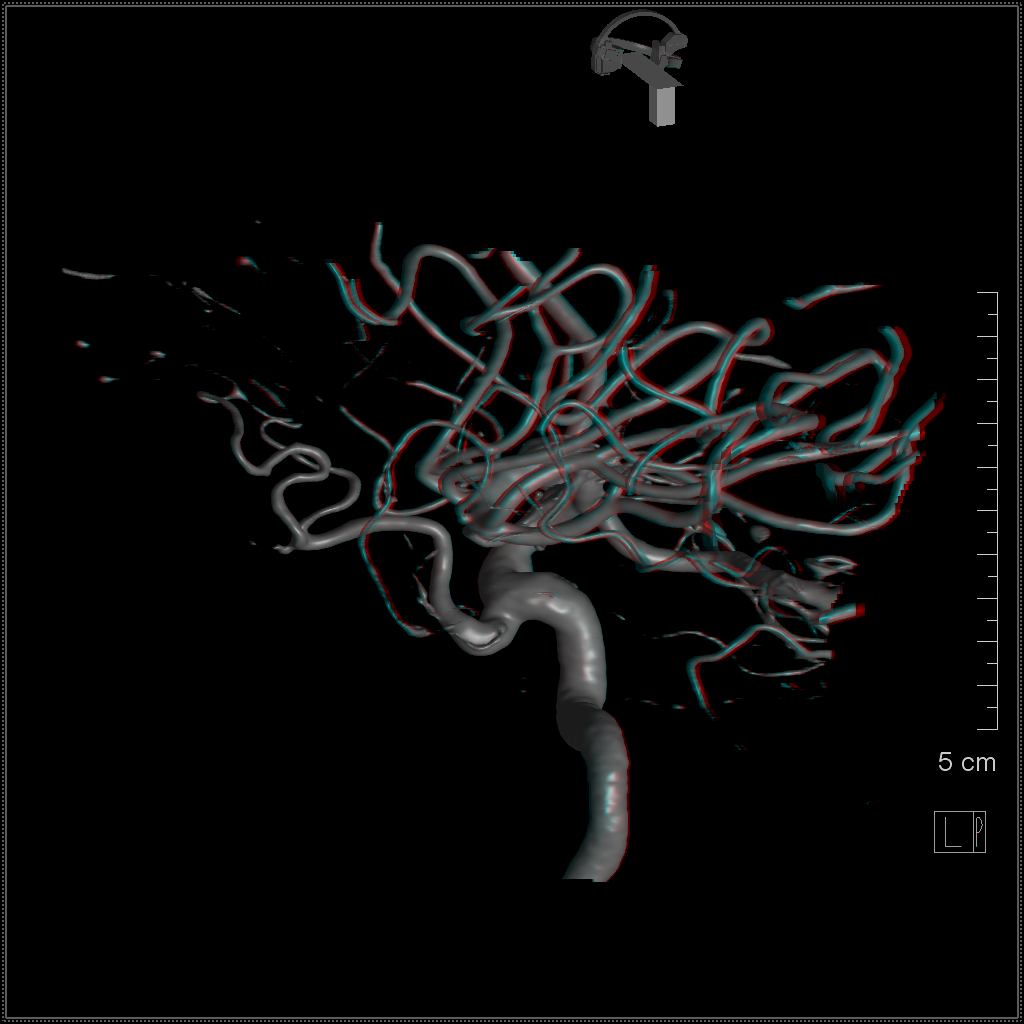
Cross eye stereo pair
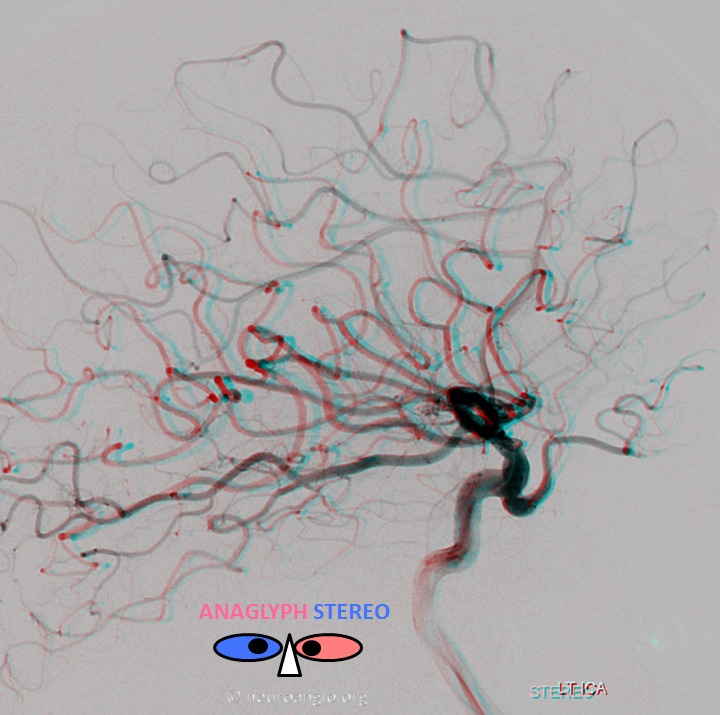
Anaglyph stereo pair
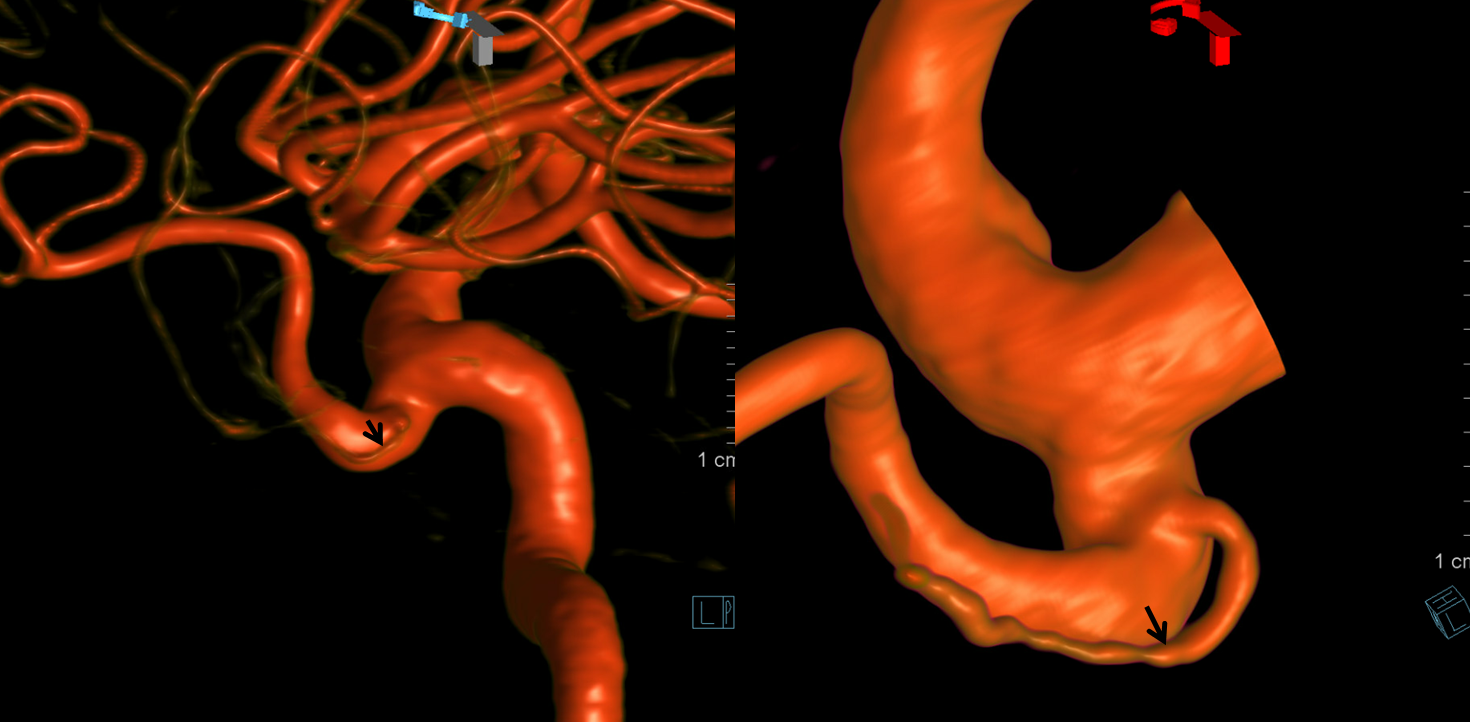
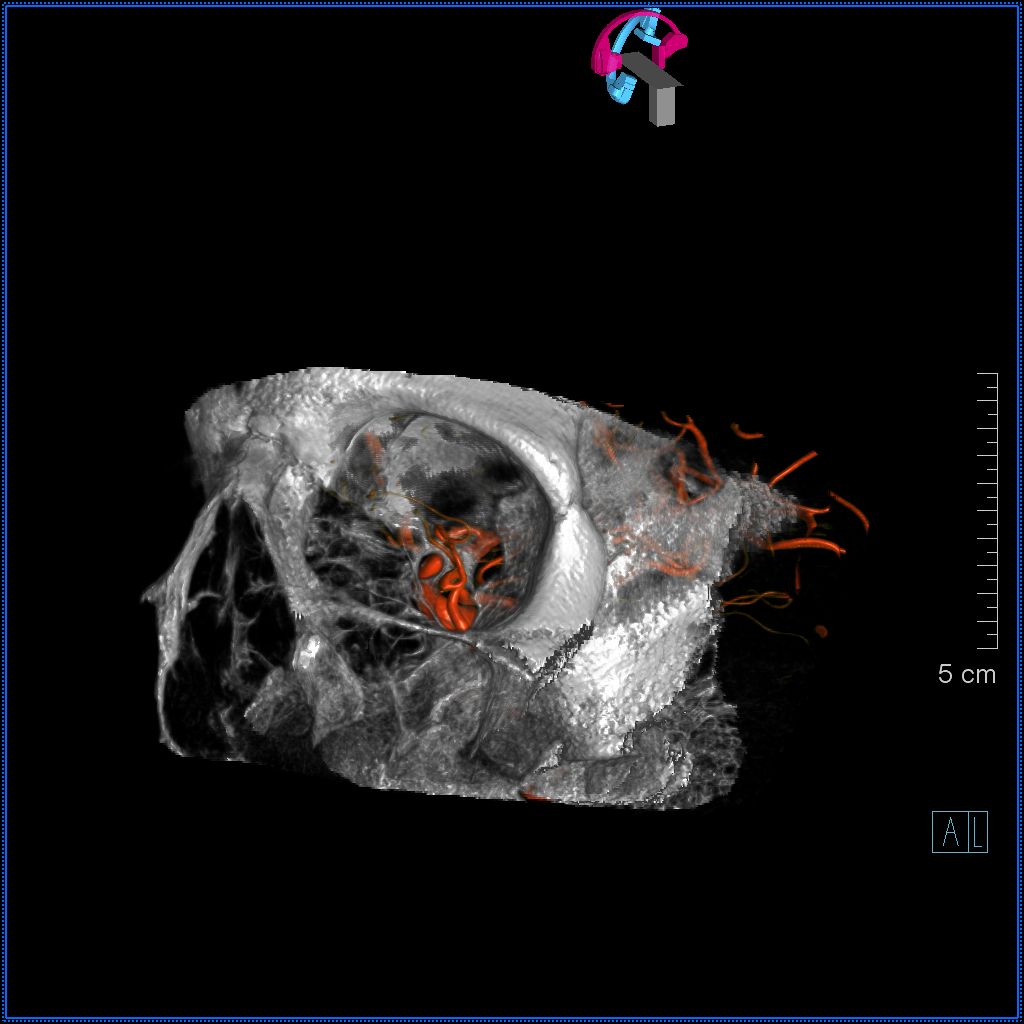
Another view — Volume Rendered (VR)

ILT = 3 = Solid Arrow; Anterolateral Trunk = 38 = arrowheads; Foramen Rotundum Branch = 37 = dashed arrows; Foramen Ovale Branch / Meningeal Branch = 34 = ball arrow; Recurrent Tentorial Arcade / Marginal Tentorial Artery = 34 = open arrows
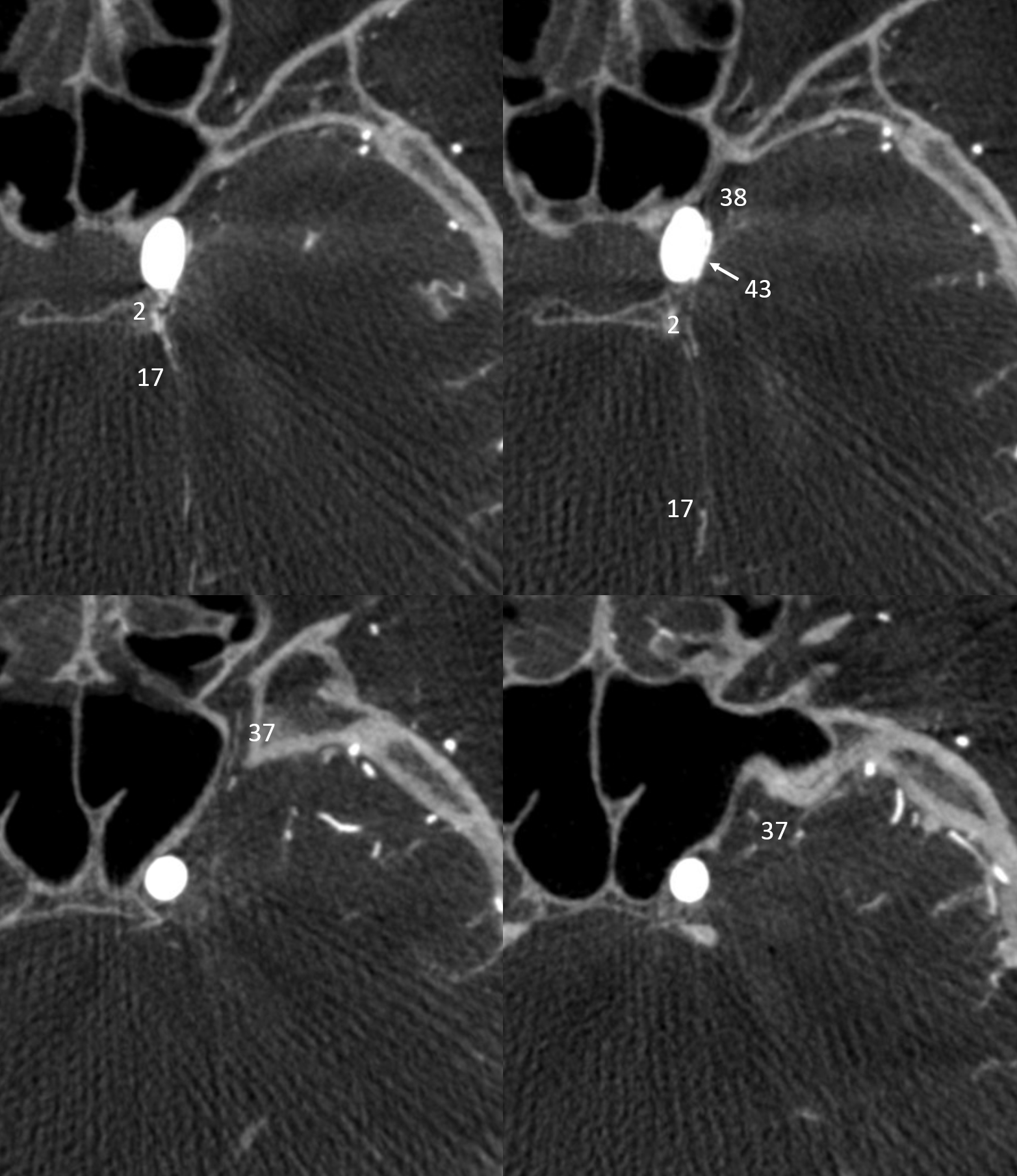
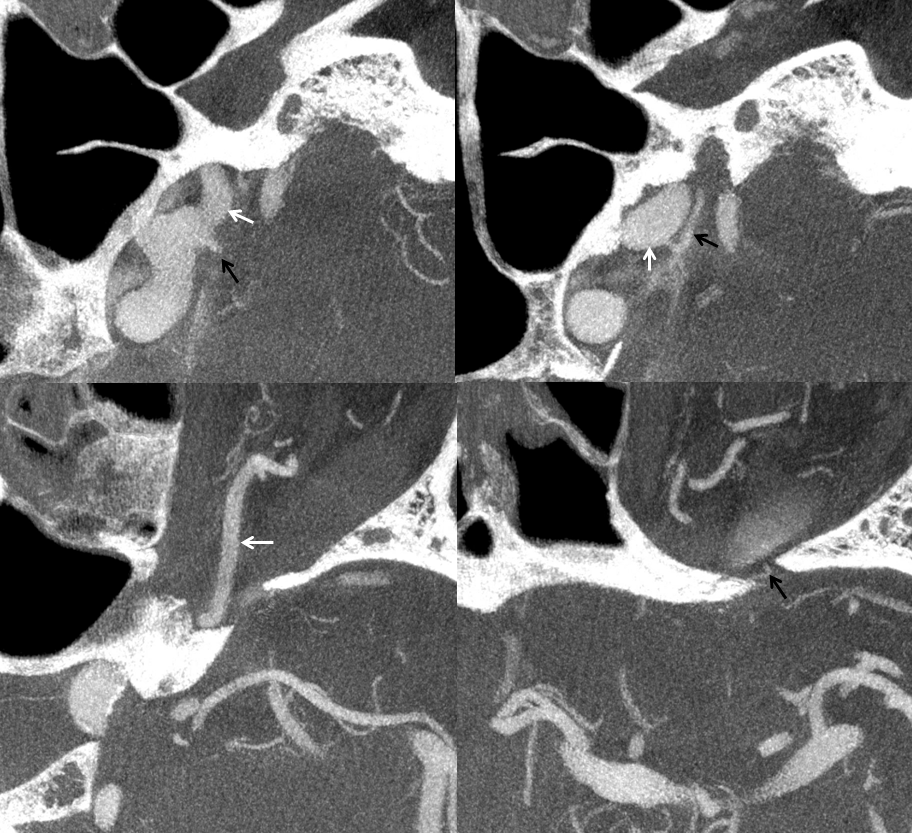
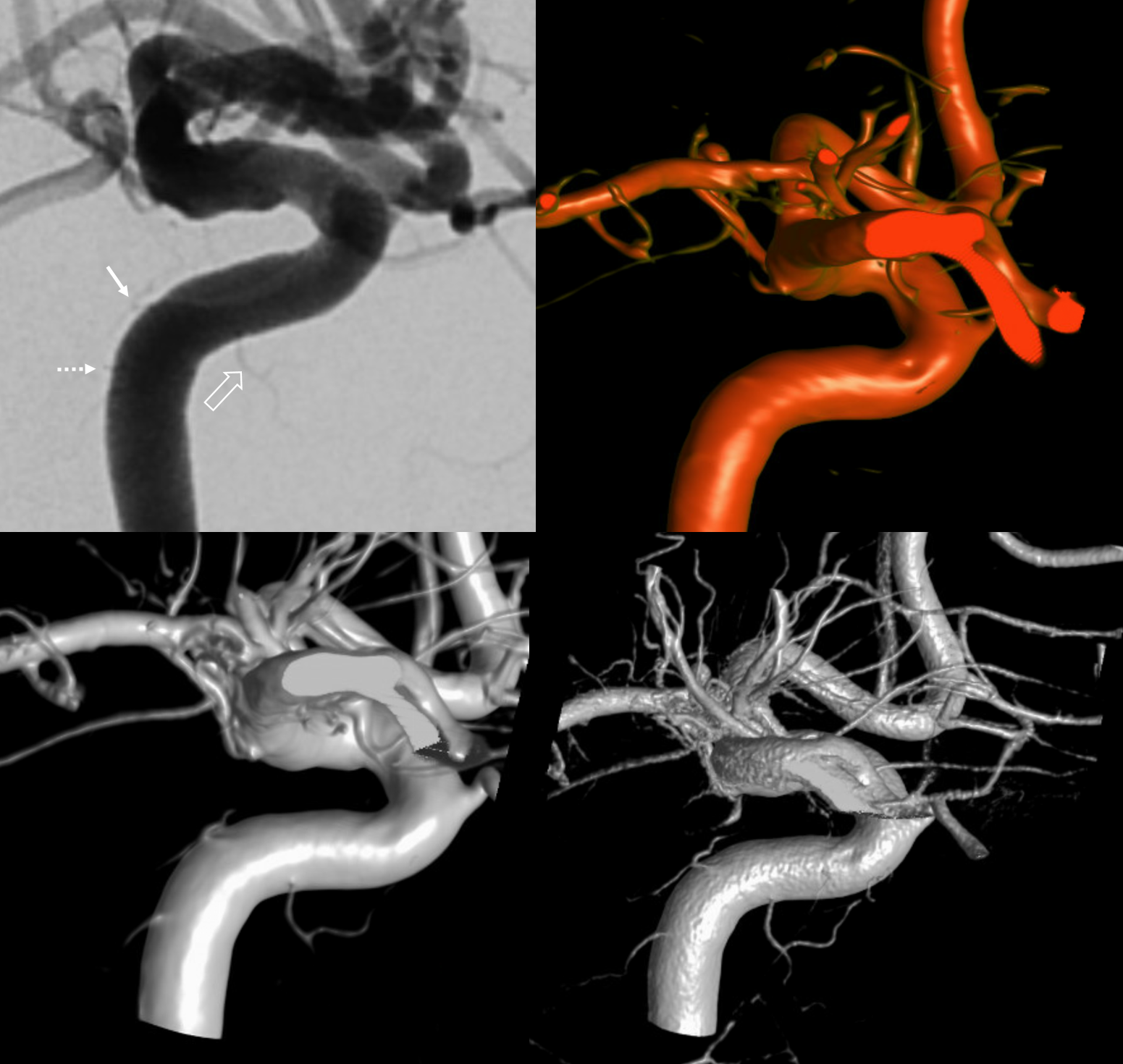
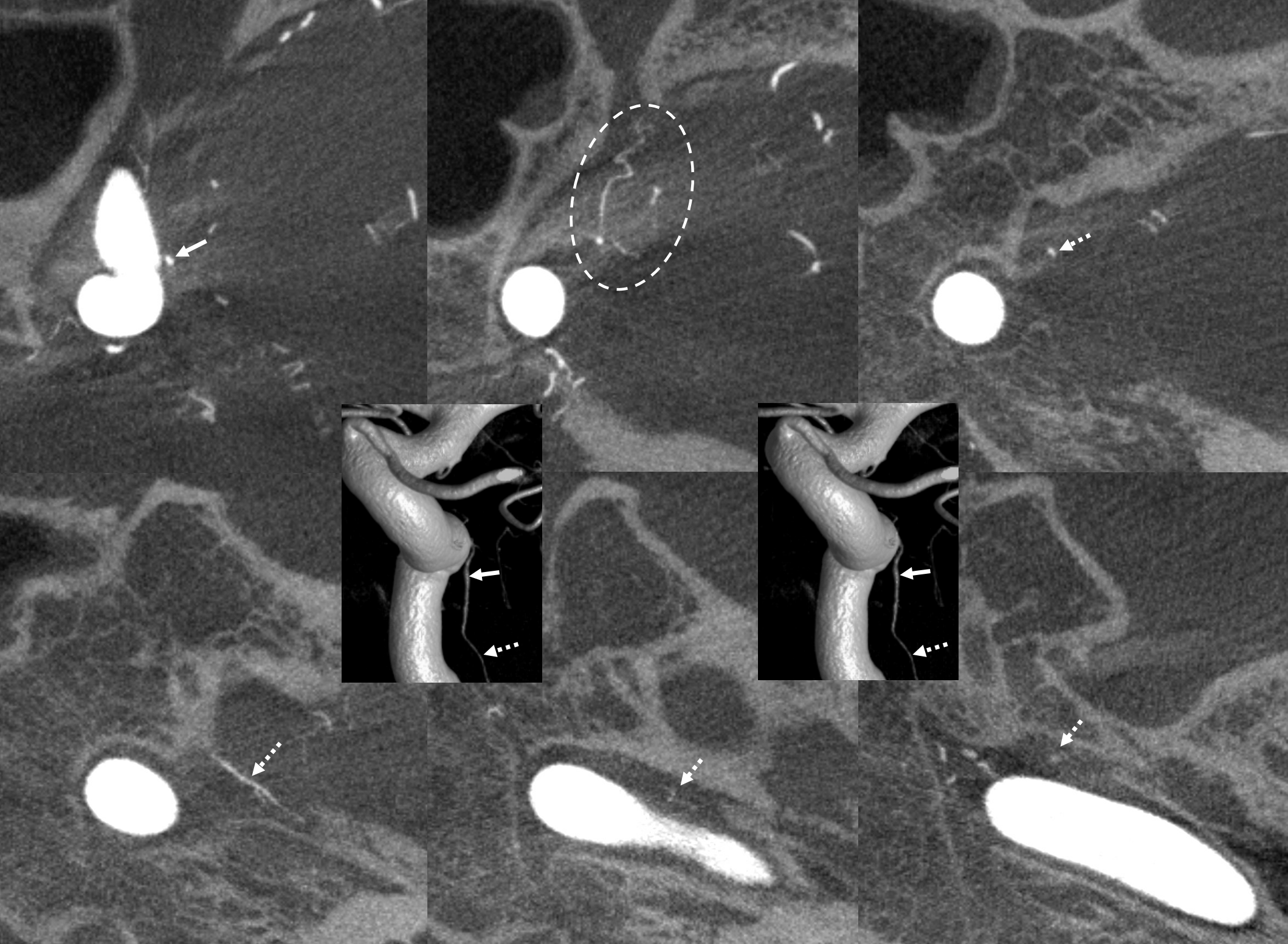
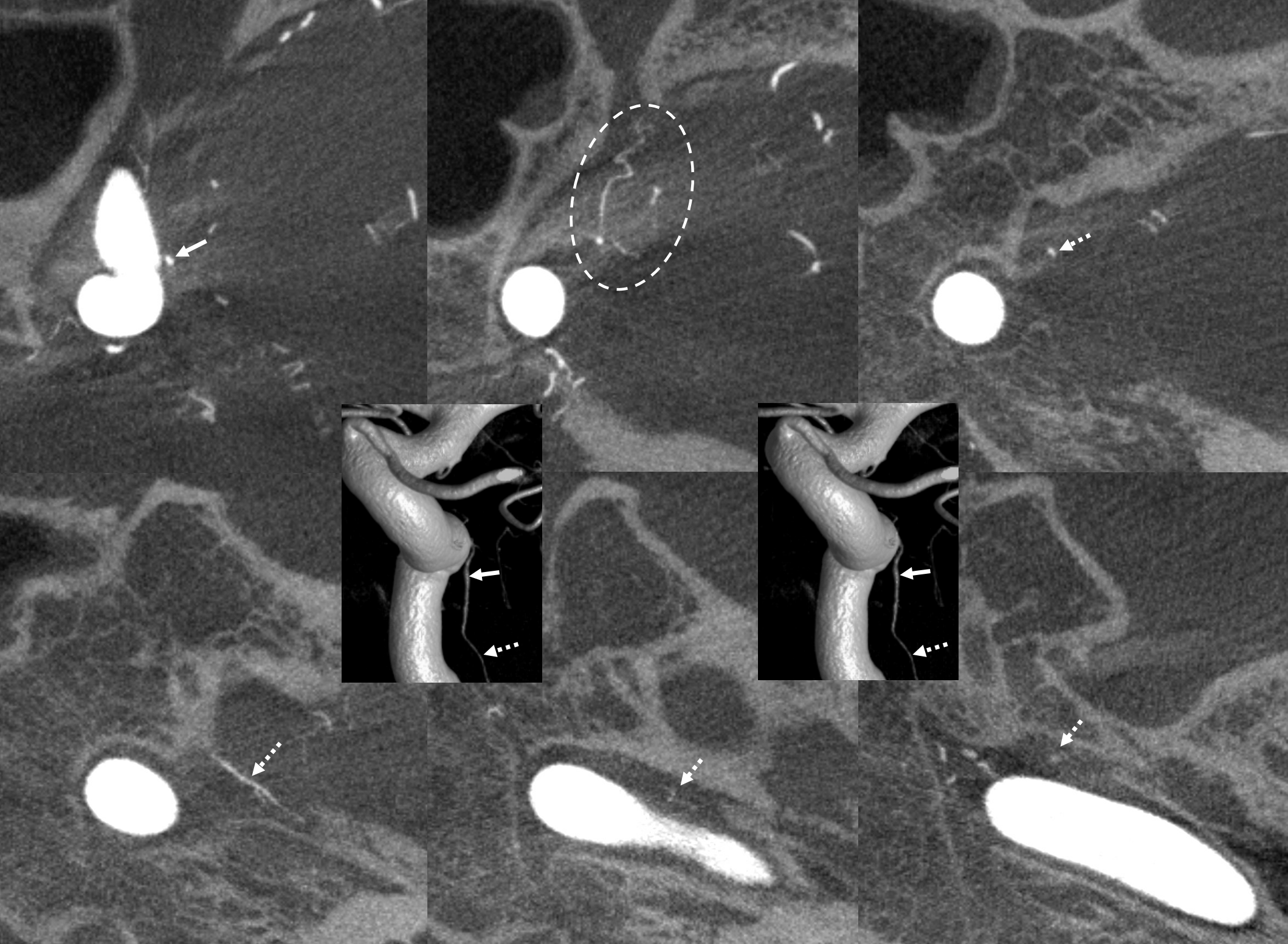
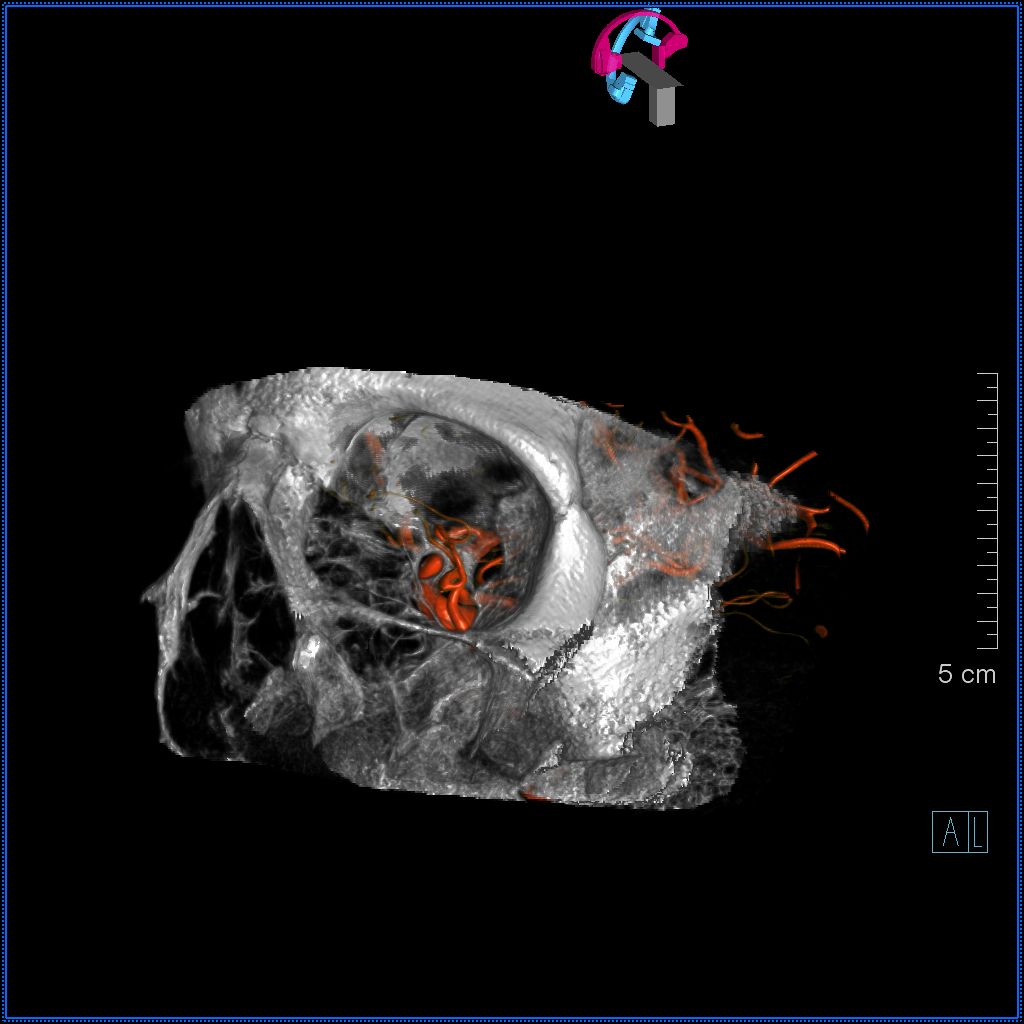
Visualization Depends on Technique
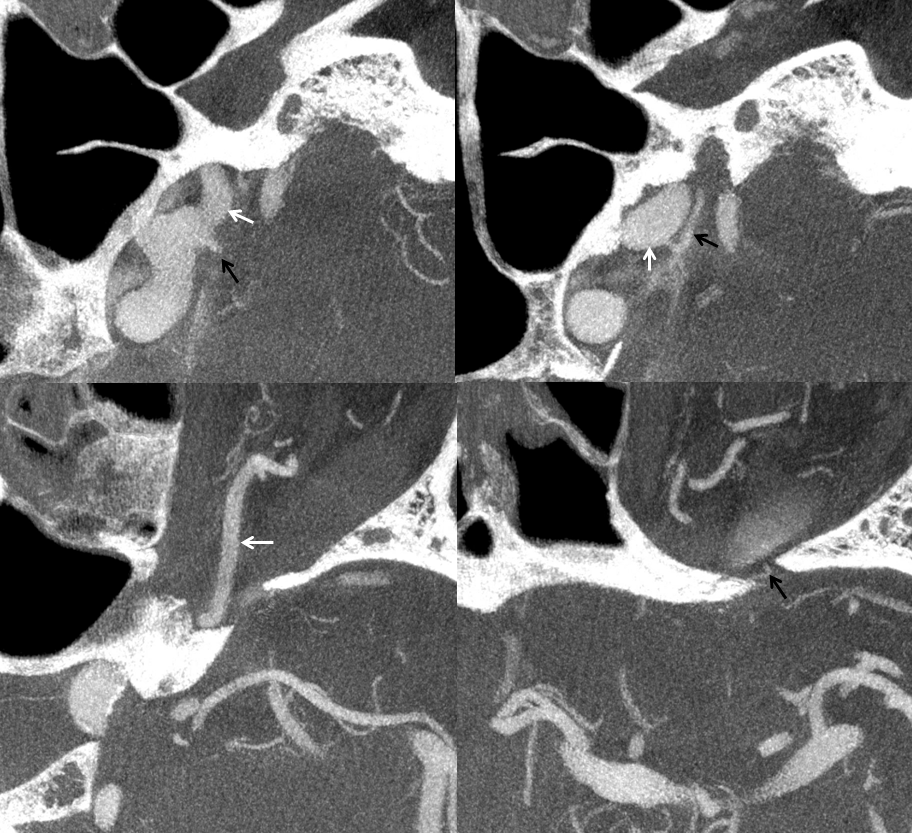
Same patient. Note presence of faintly visible MHT (solid and dashed arrows) and ILT (open arrow) branches on DSA. The same are not visible on a “subtracted” “3D-DSA” (top right). However, the same branches in the same patient are well seen on the “unsubtracted, natural fill” 3D-DSA (same acquisition, different algorithm, bottom left). Finally, the same are even better seen on a detailed “sharp” protocol reconstruction — bottom right. The point is that our techniques always change — but the fact is that ability to visualize something depends on optimal protocols and some patience.
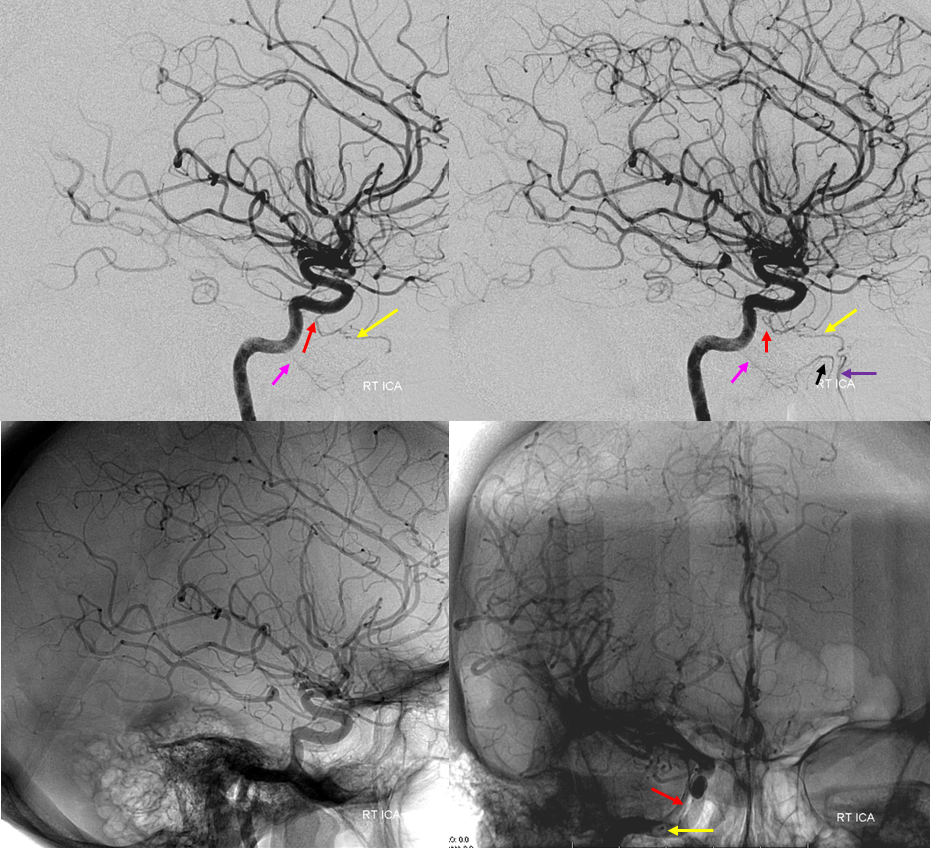
Prominent artery of the foramen rotundum
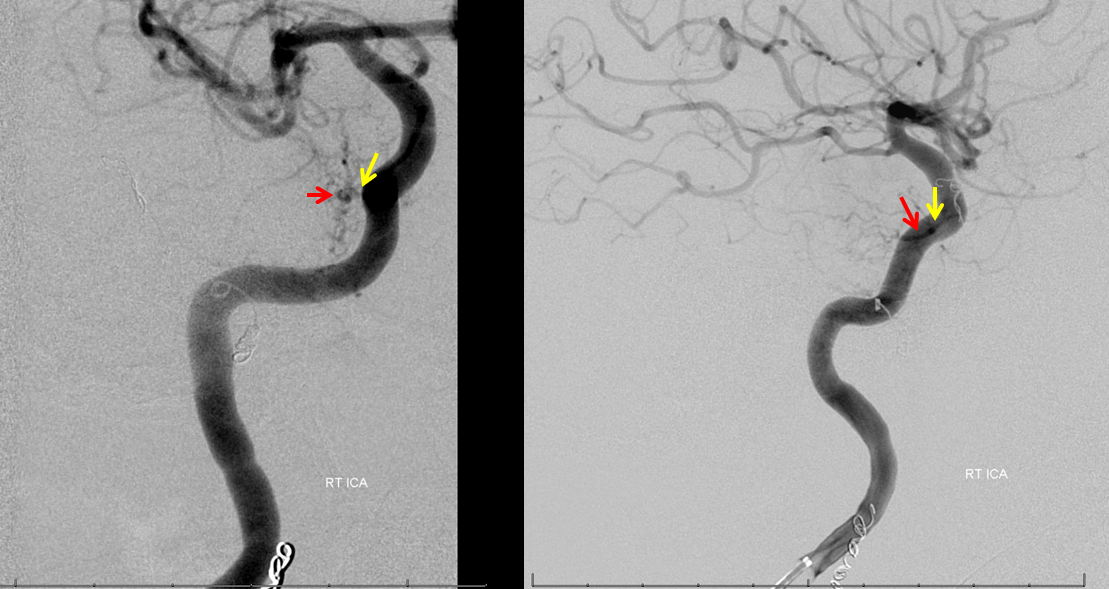
In this patient, a normally prominent ILT (red) supplies artery of the foramen rotundum (yellow), which supplies the roof of the nasopharynx, in combination with the also somewhat prominent Mandibulovidian Artery (pink) taking over the territory of the ascending pharyngeal in supply of the posterolateral nasopharynx (black). The greater palatine artery is purple. Notice the “down the barrel” view of the foramen rotundum artery within the foramen rotundum on the frontal native view (lower right).
Dominant artery of foramen rotundum in a smaller ILT
The other side of the coin — remember balance! If ILT is small, something else has to be bigger. Here the ILT is not really visible on angio — there is a visible MHT (2). Also has a well-seen usually tiny pterygovaginal artery (53)
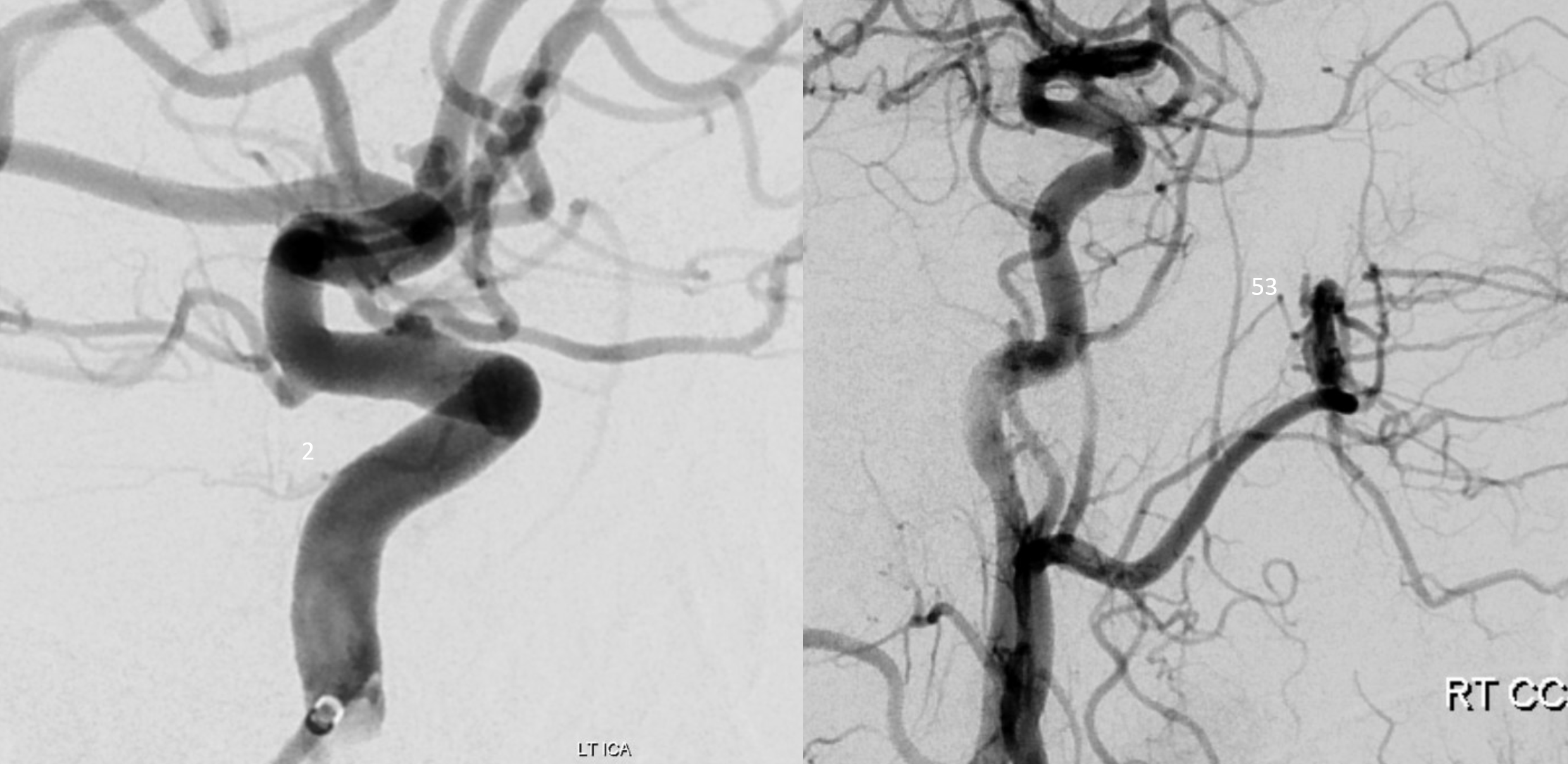
DYNA CT shows the full picture… MHT (2) supplies medial tentorial arcade (17). A small ILT branch nearly parallel to the ICA is the clival branch (43). There is a very tiny anteromedial branch to the SOF (38). The balance is here is that ILT is small, so something else has to be bigger. In this case its the artery of foramen rotundum (37) which sends two small branches towards middle cranial fossa floor (37, lower right image)
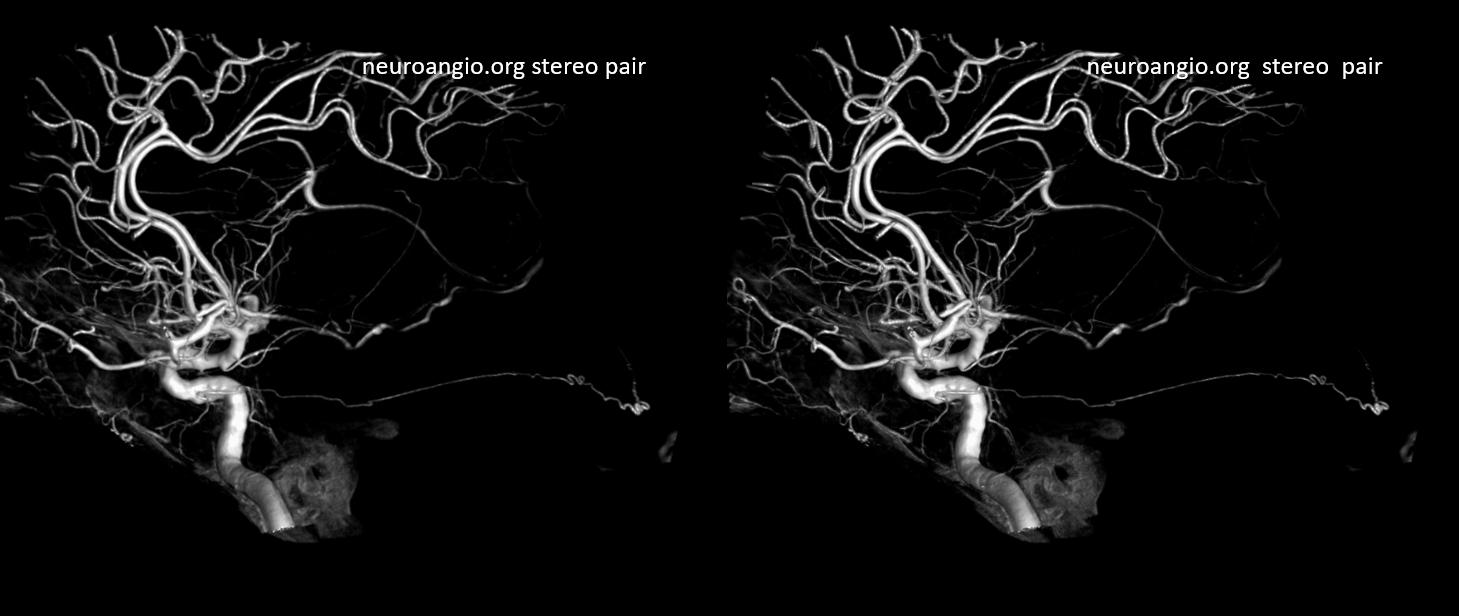
Another patient (ruptured anterior choroidal aneurysm, stereo pair) with normal well-visualized ILT and MHT. The anteromedial branch (black) and either rotundum or ovale branche (purple) are seen from the ILT. The lateral tentorial arcade (blue) and inferior clival branch (white) are from the MHT
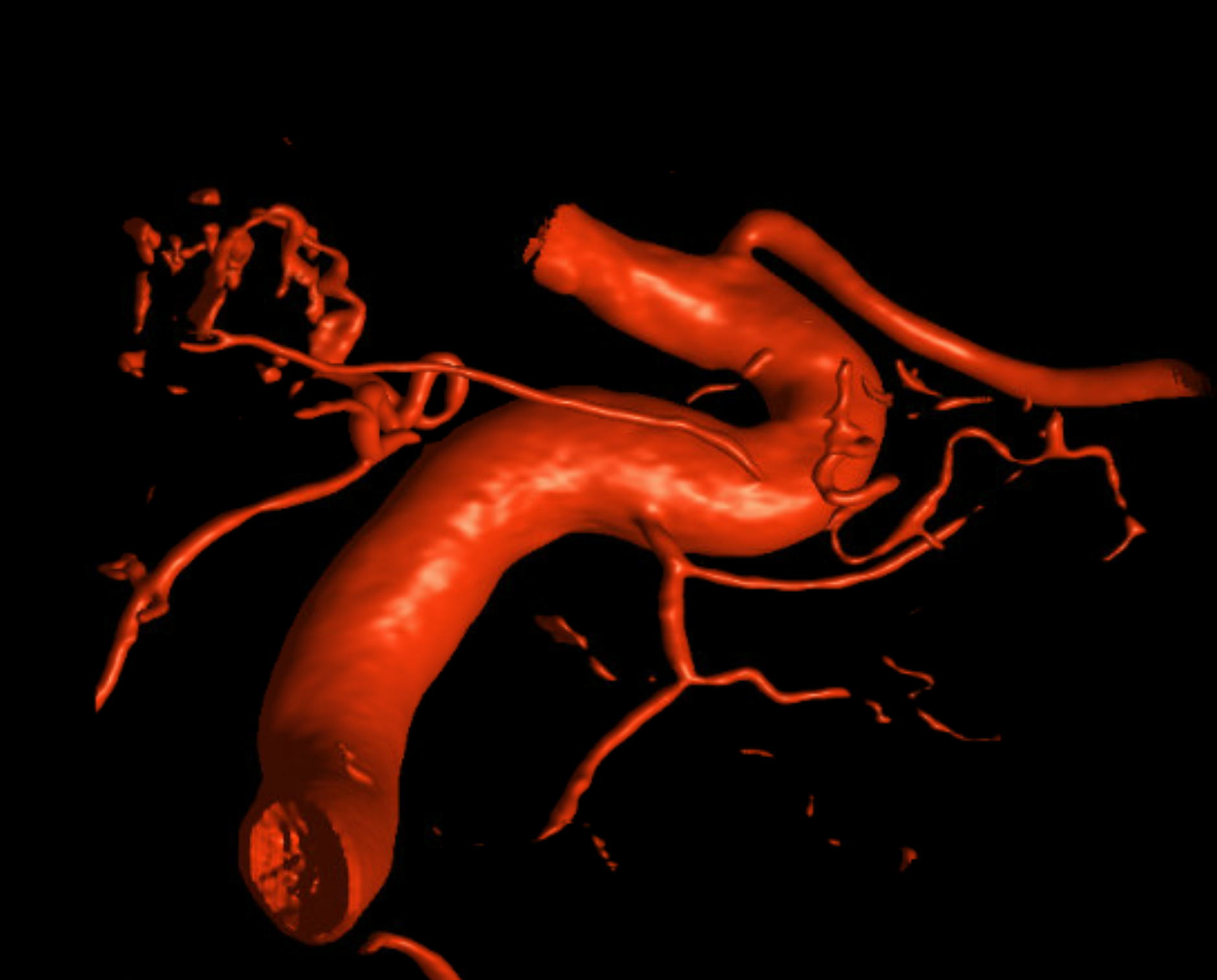
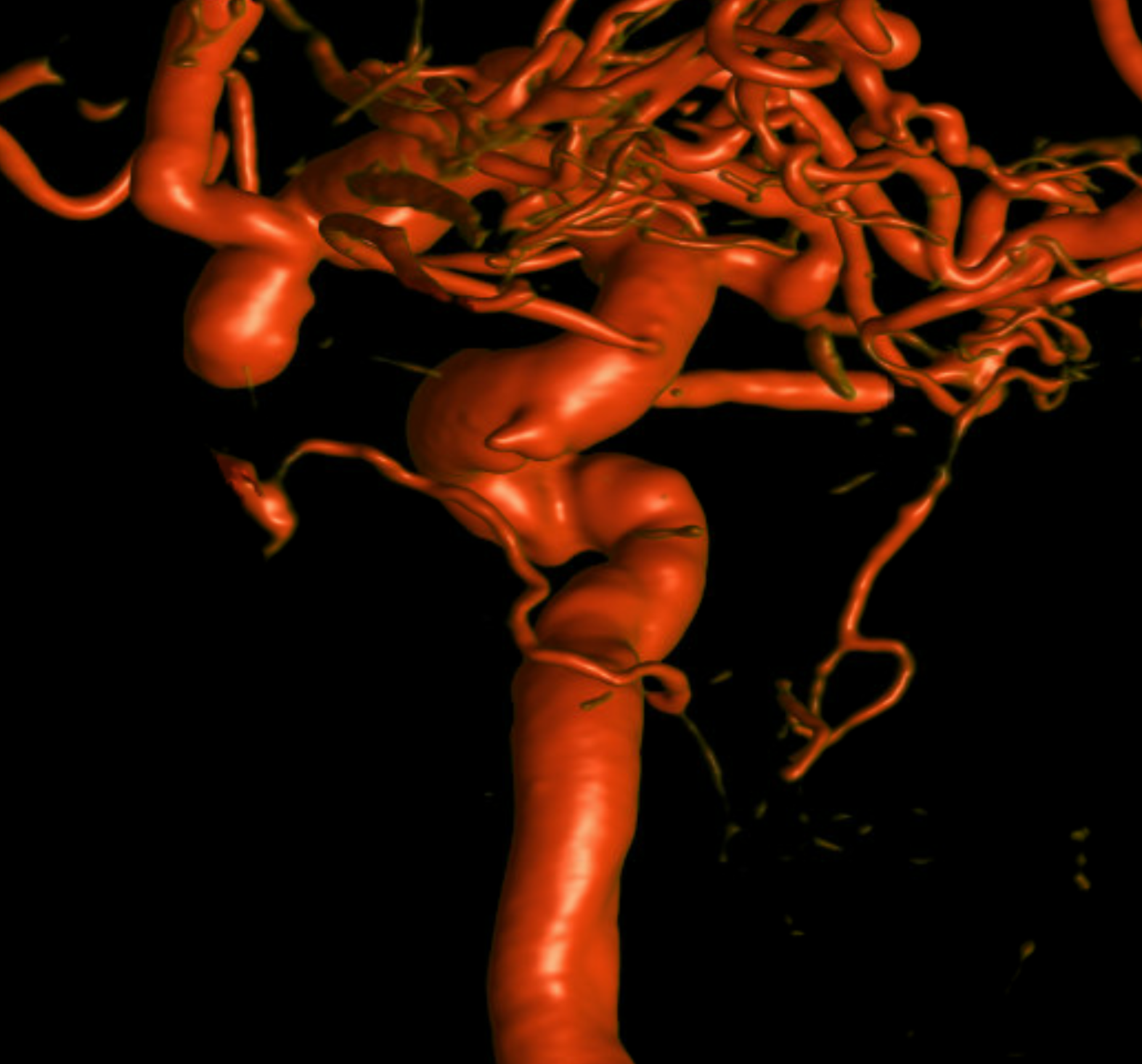
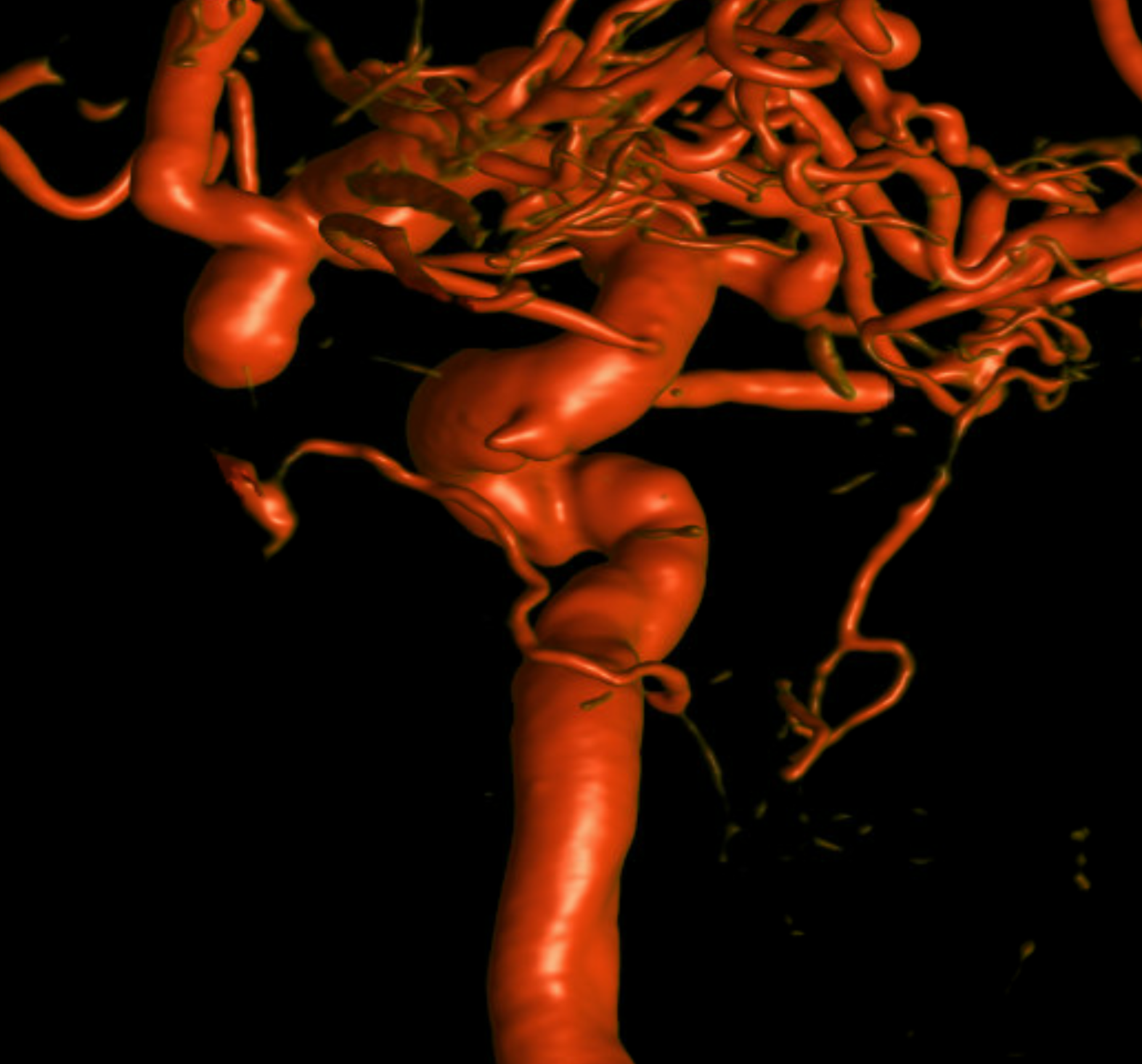
ILT — Ascending Pharyngeal Balance
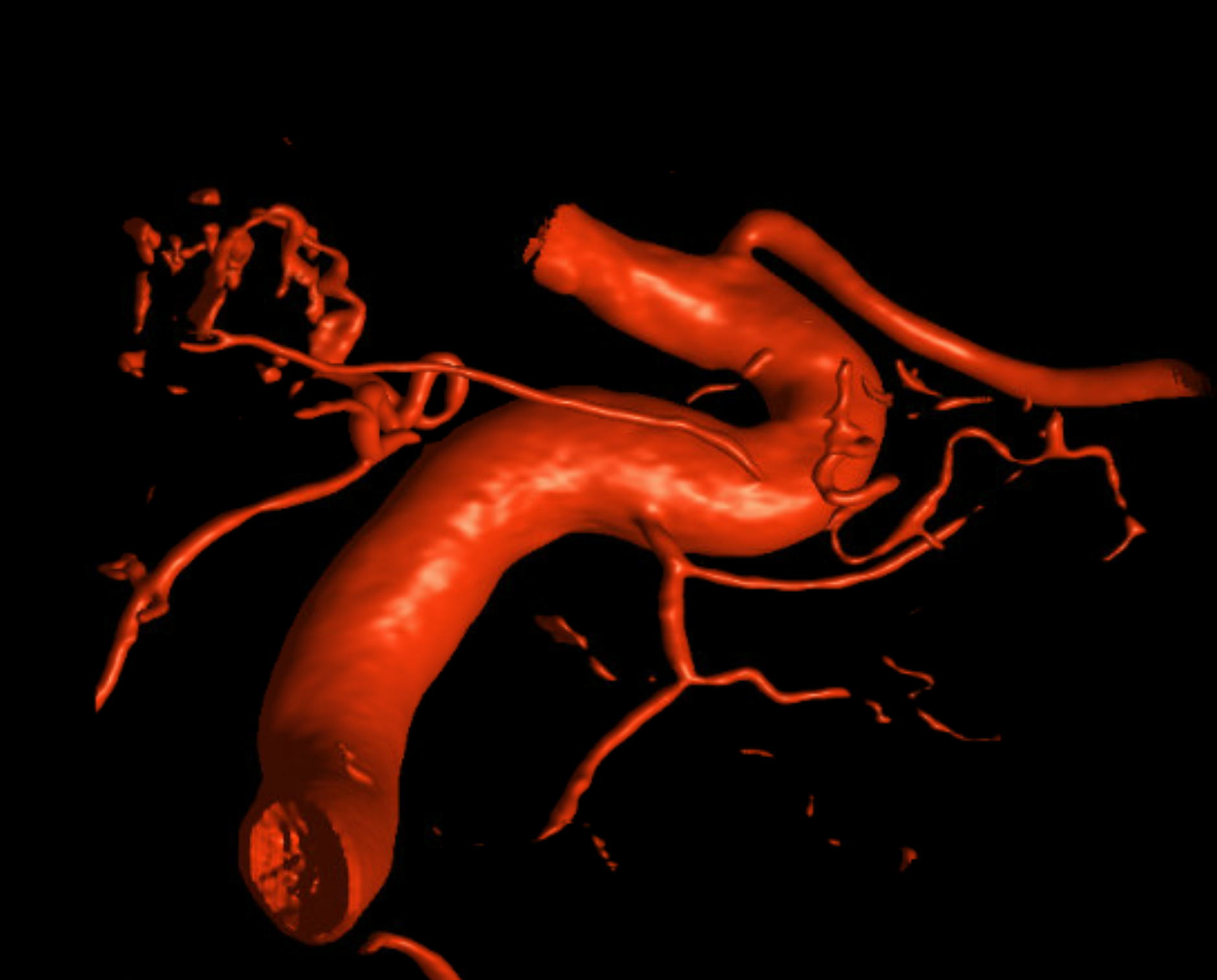
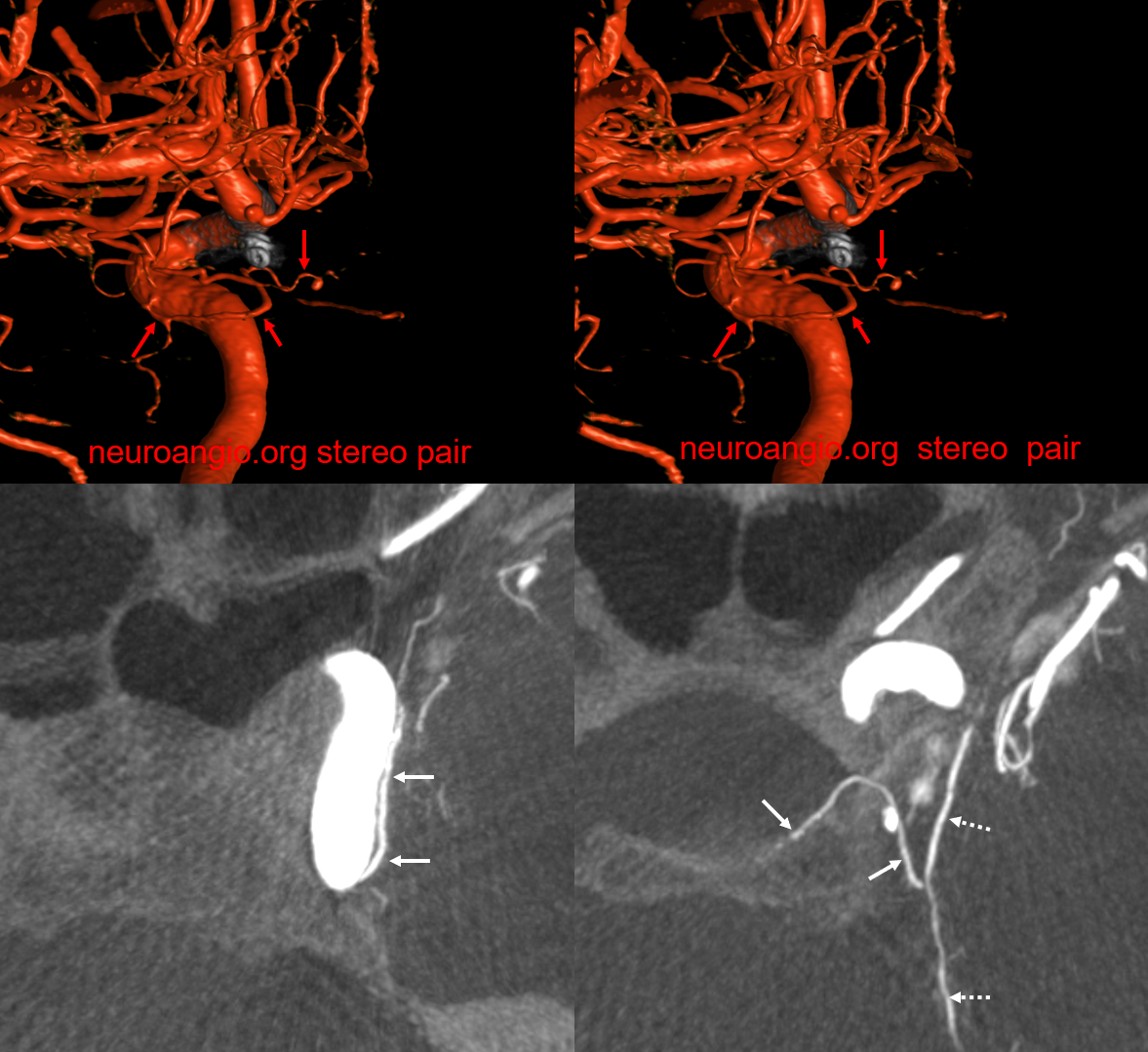
Although there are several potential connections between the neuromeningeal trunk of the AP and the ICA (“dangerous anastomoses”), the pharyngeal trunk of the AP is not without hazard either. The carotid branch of the pharyngeal trunk (superior division mostly) potentially connects with the ICA via the inferior branches of the ILT. The carotid branch reaches the ILT via foramen lacerum — a curious thing for the fake foramen. In the below example (think balance and spectrum), the reverse is true — the ILT (white arrow) has a prominent extension (dashed arrows) below the rotundum branches (ovals), into the carotid canal and foramen lacerum. The middle VR images are stereo pairs.
Patency After Pipeline Embolization
Not something explored much. But interesting. Quite a few MHTs and ILTs stay open after flow diversion with Pipeline. One might think that dura has rich collaterals, similar to ophthalmic, and therefore we can expect ILT and MHT to close frequently. Does not seem to be the case.
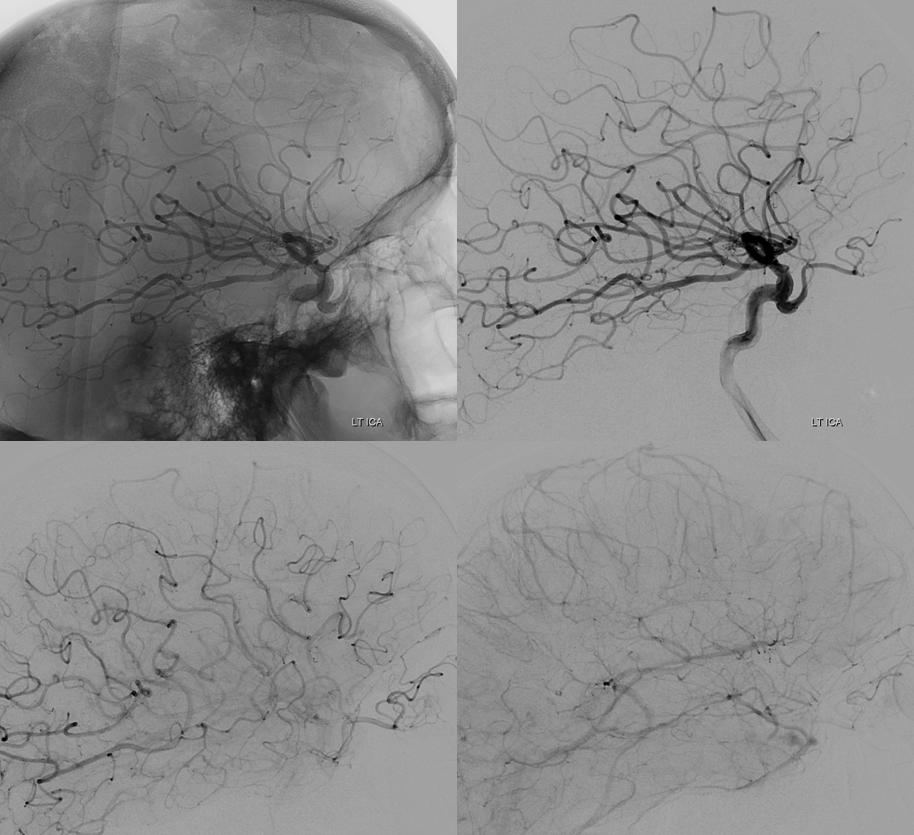
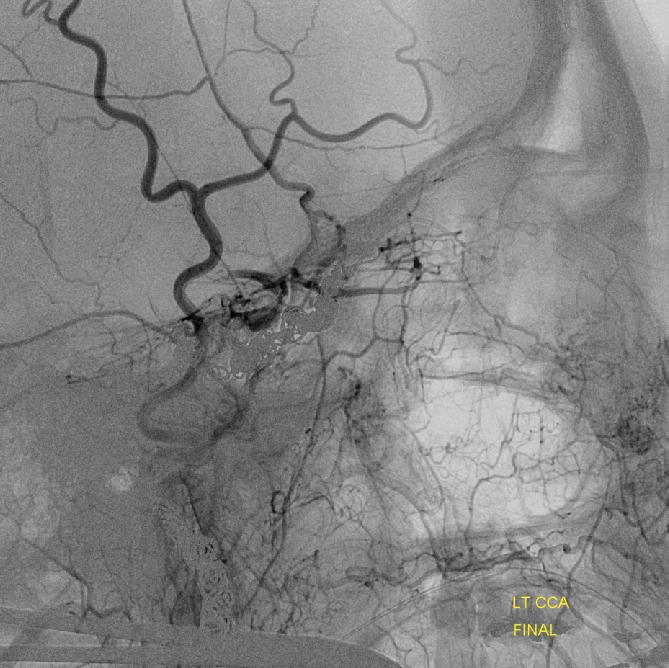
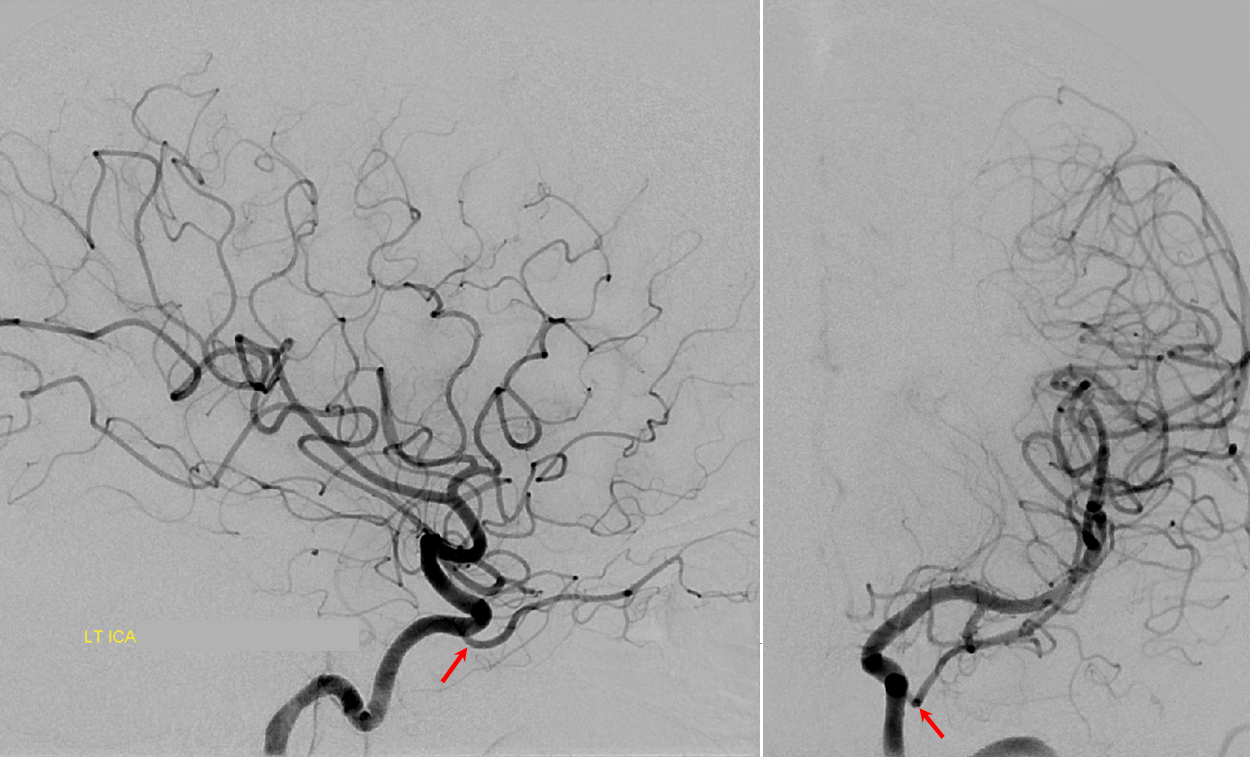
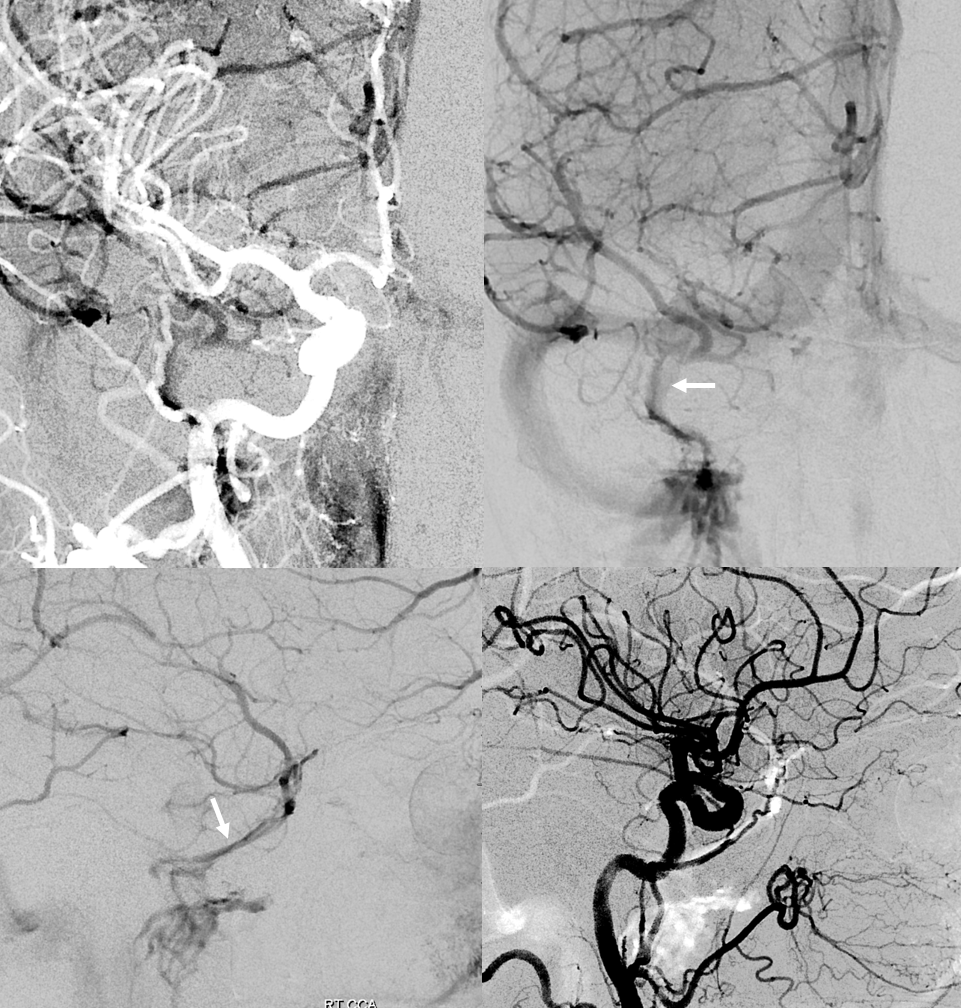
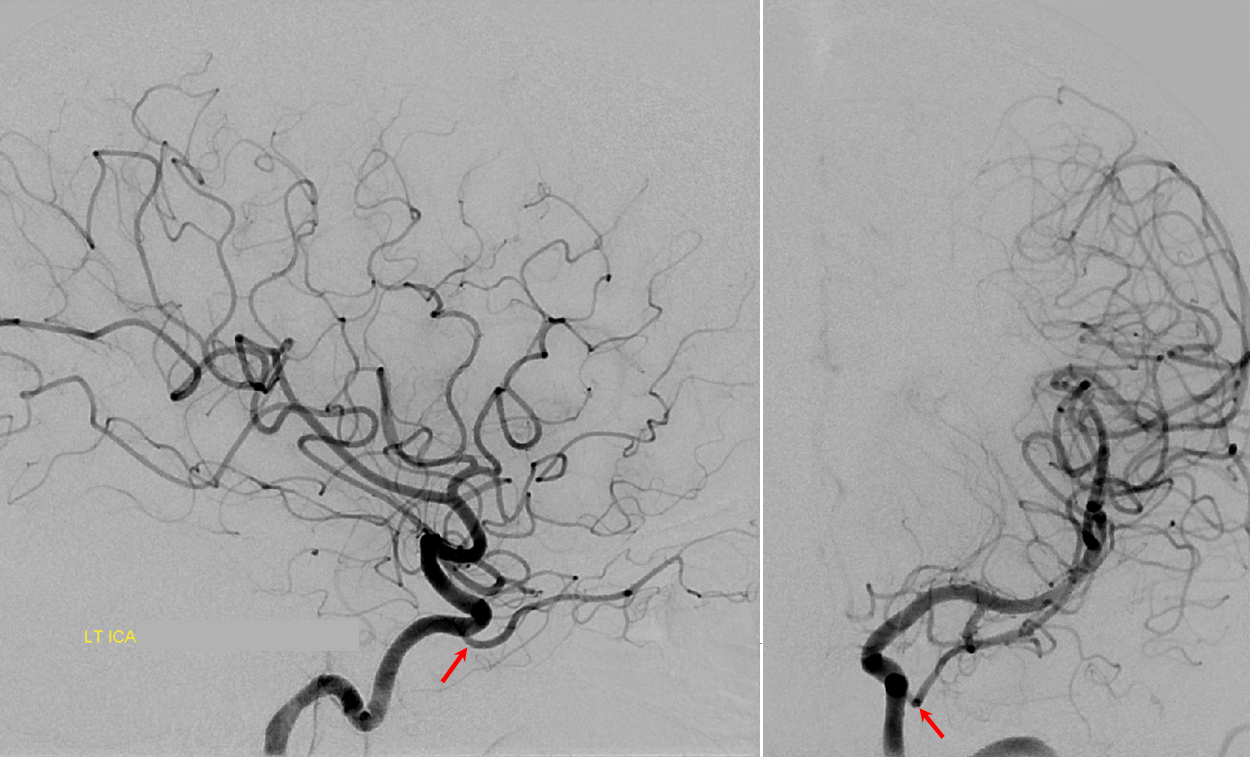
ILT reconstitution of the ICA
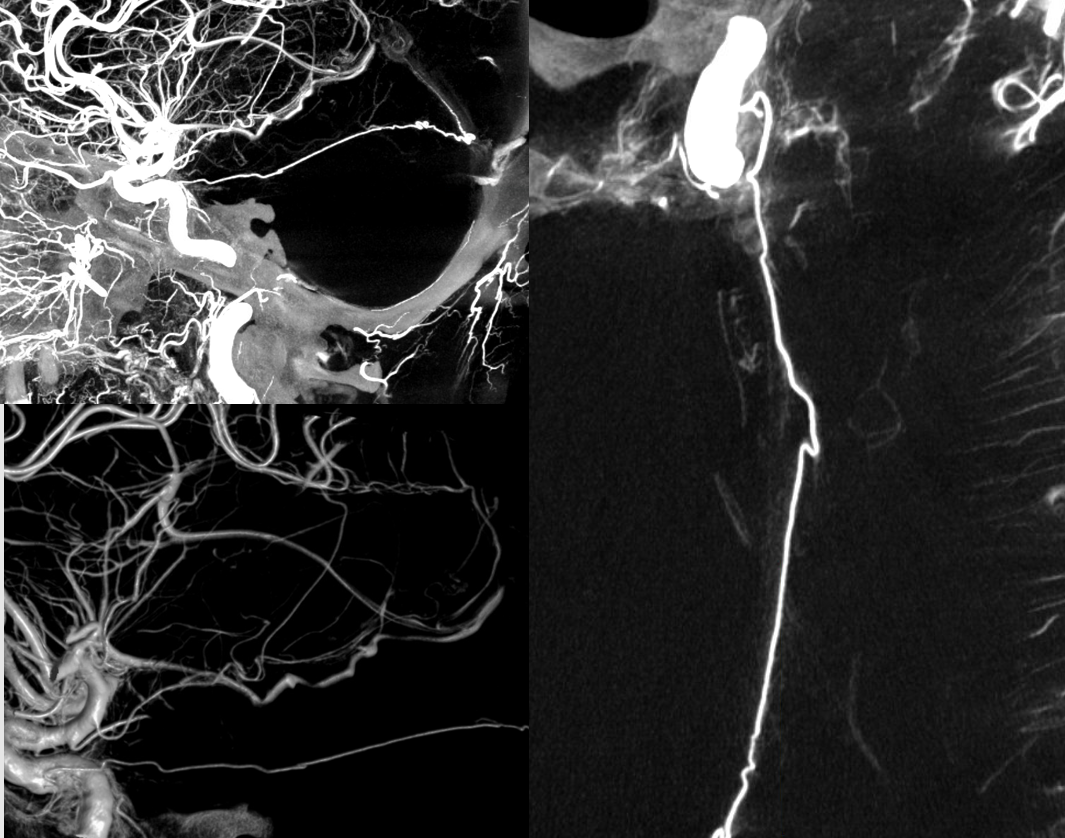
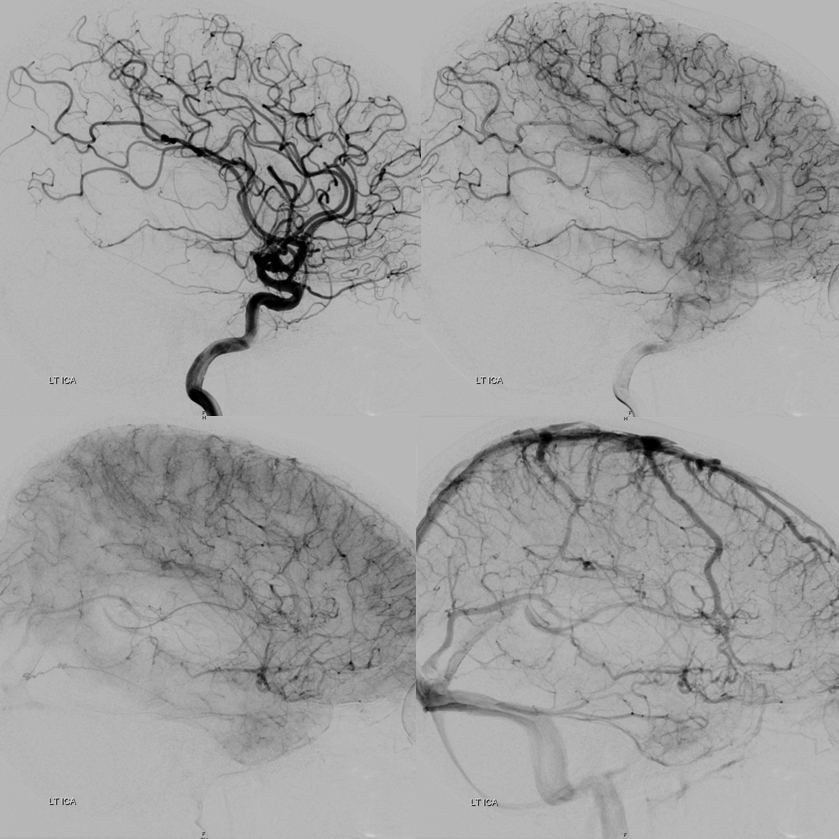
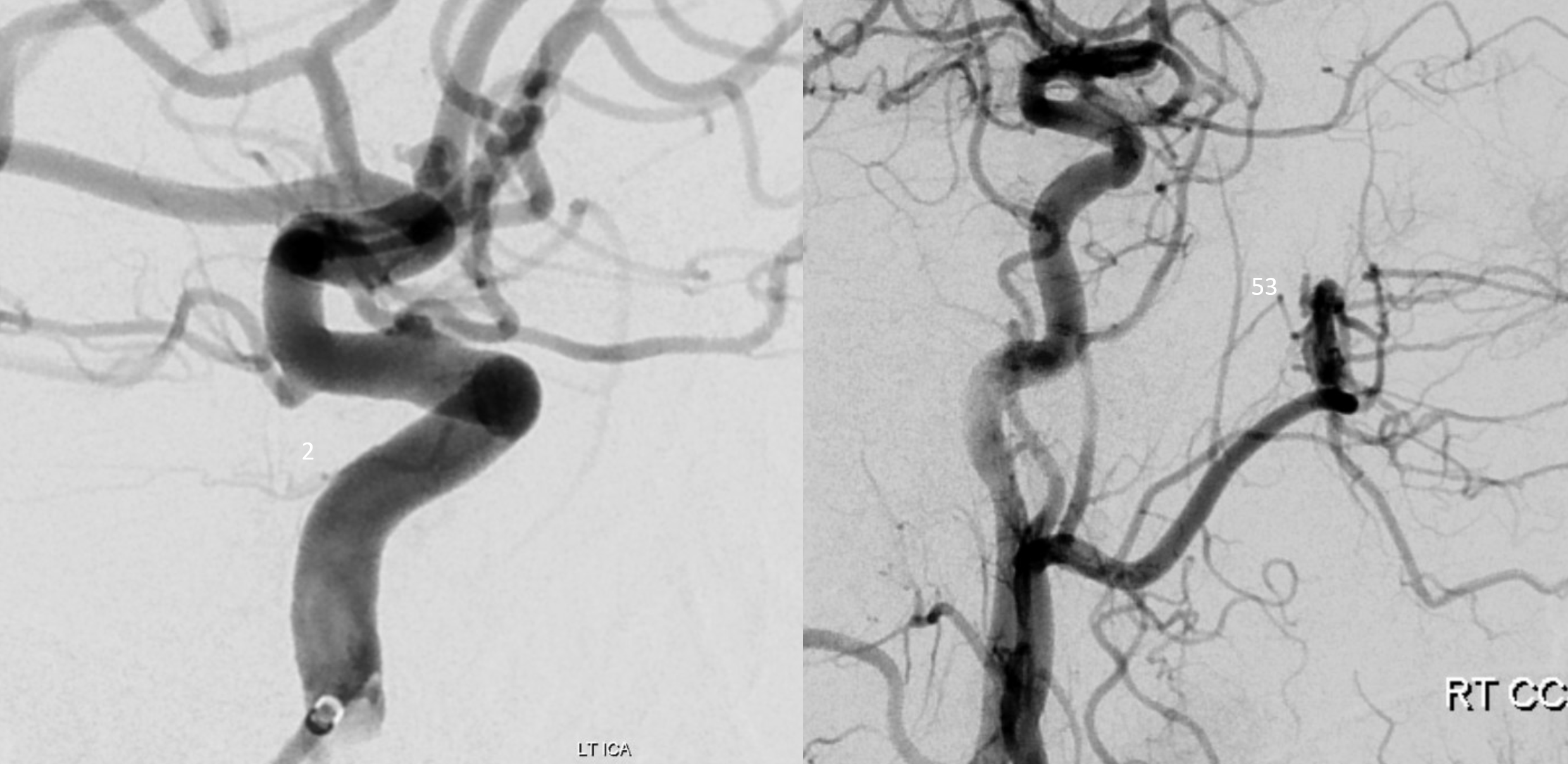
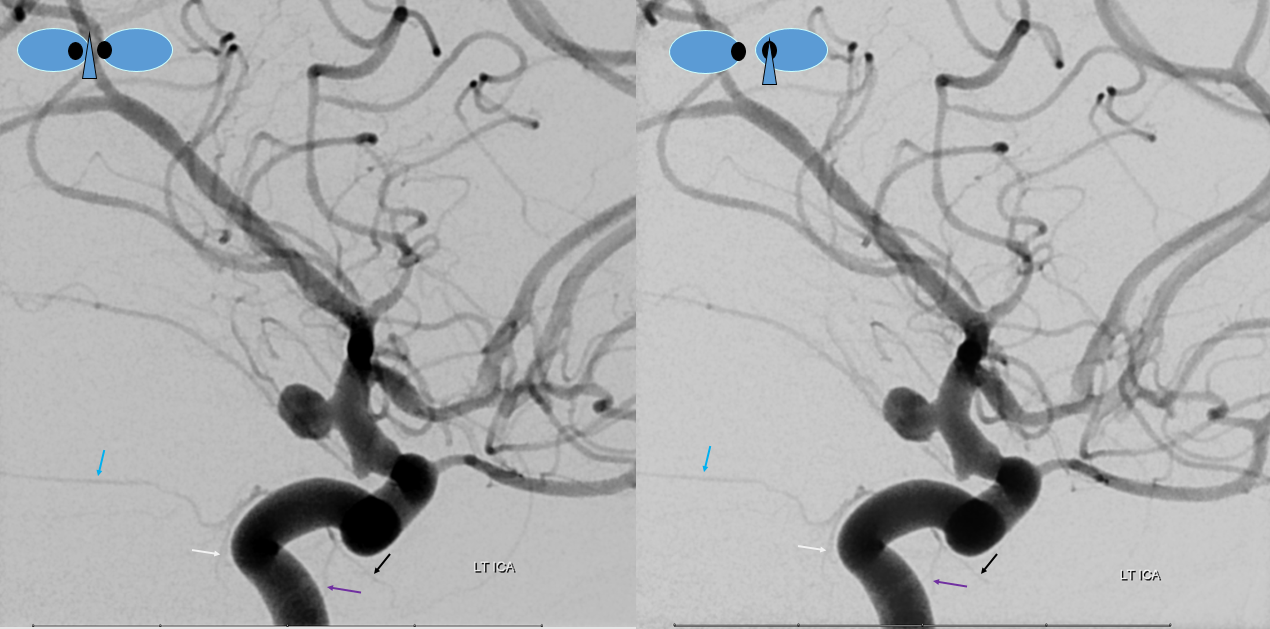
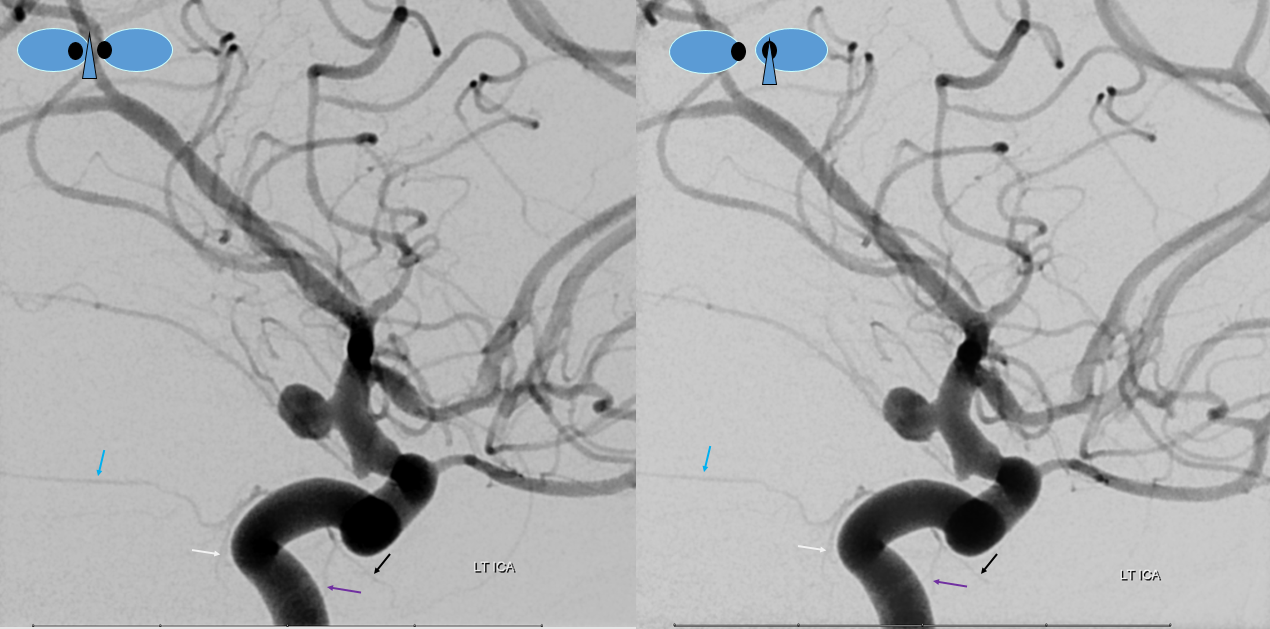
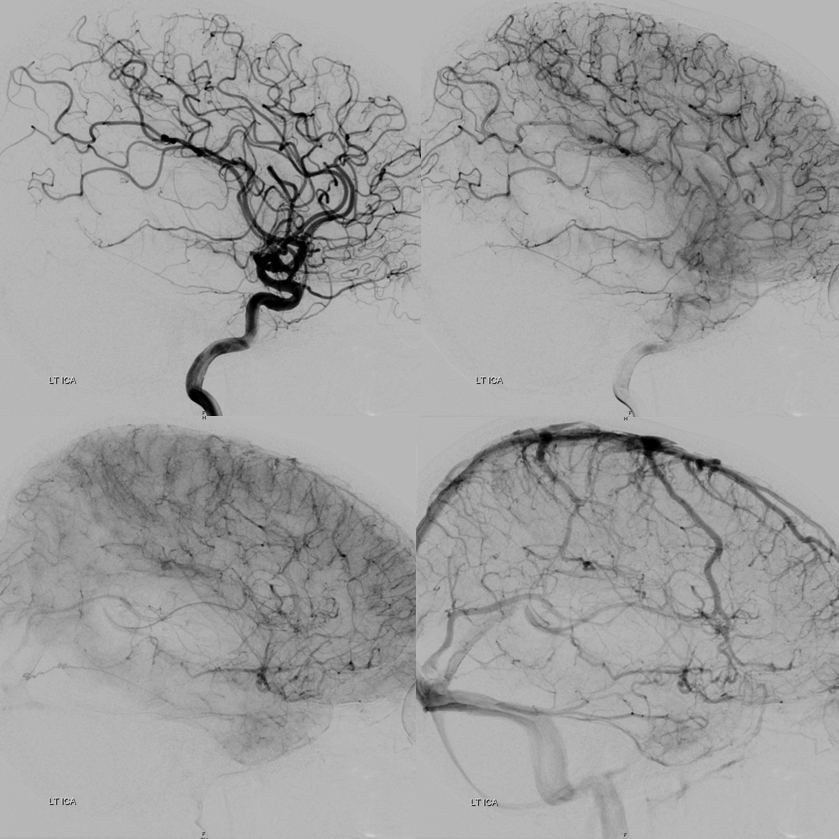
Left ICA — chronic occlusion. Accessory Meningeal and Foramen Rotundum reconstitution of the carotid via the ILT — look ’em up! Full case — great revascularization of the left M2 via the PCOM is here

Another case
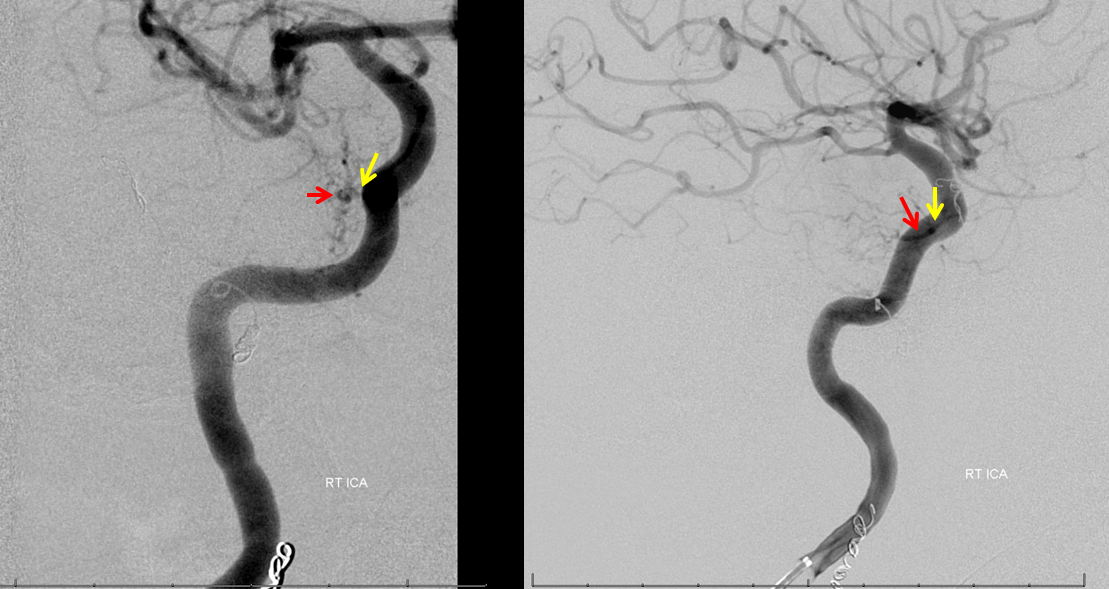
The ILT, along with the ophthalmic artery, is a primary pathway of ICA reconstitution following proximal occlusion. Common routes include foramen rotundum branch, accessory and cavernous branches of the accessory and middle meningeal arteries.
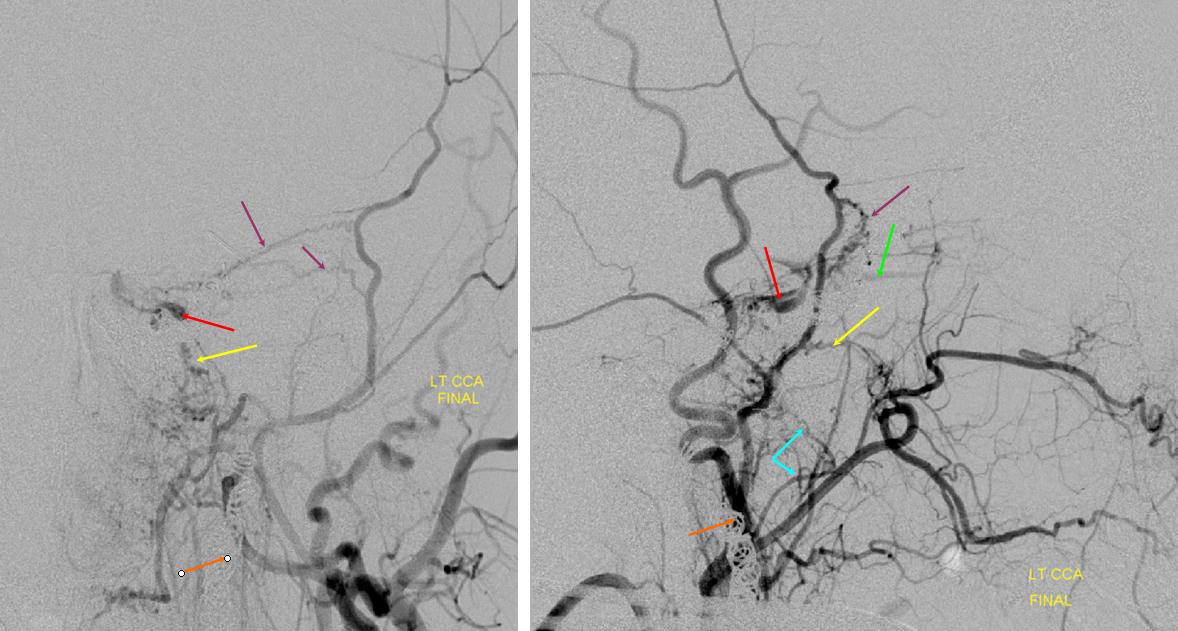
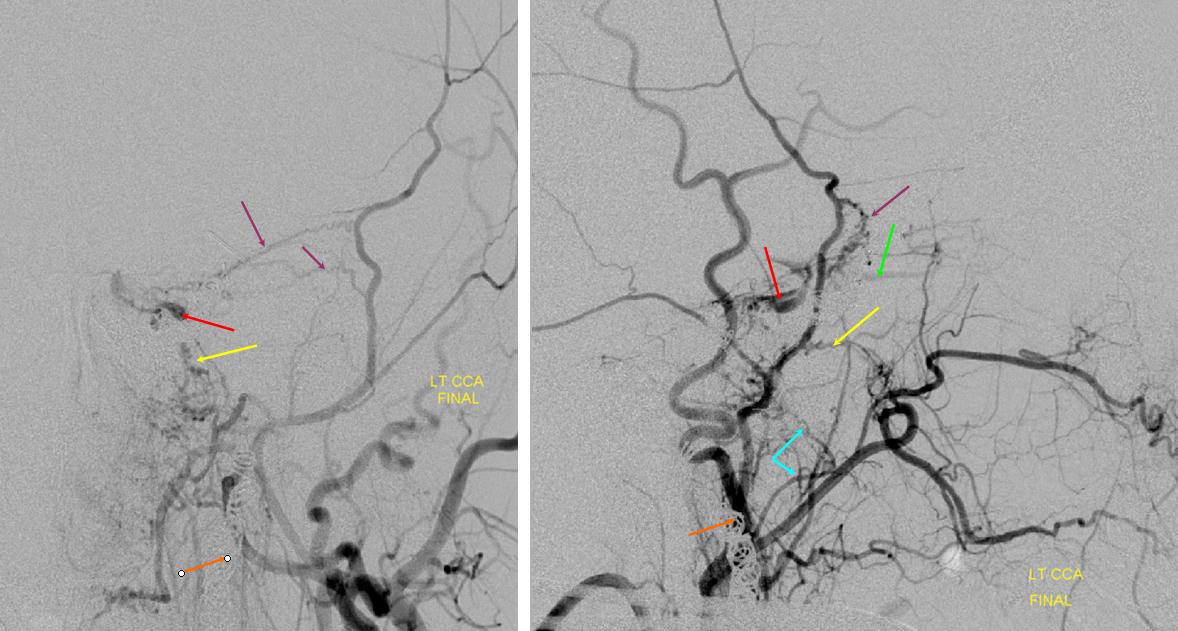
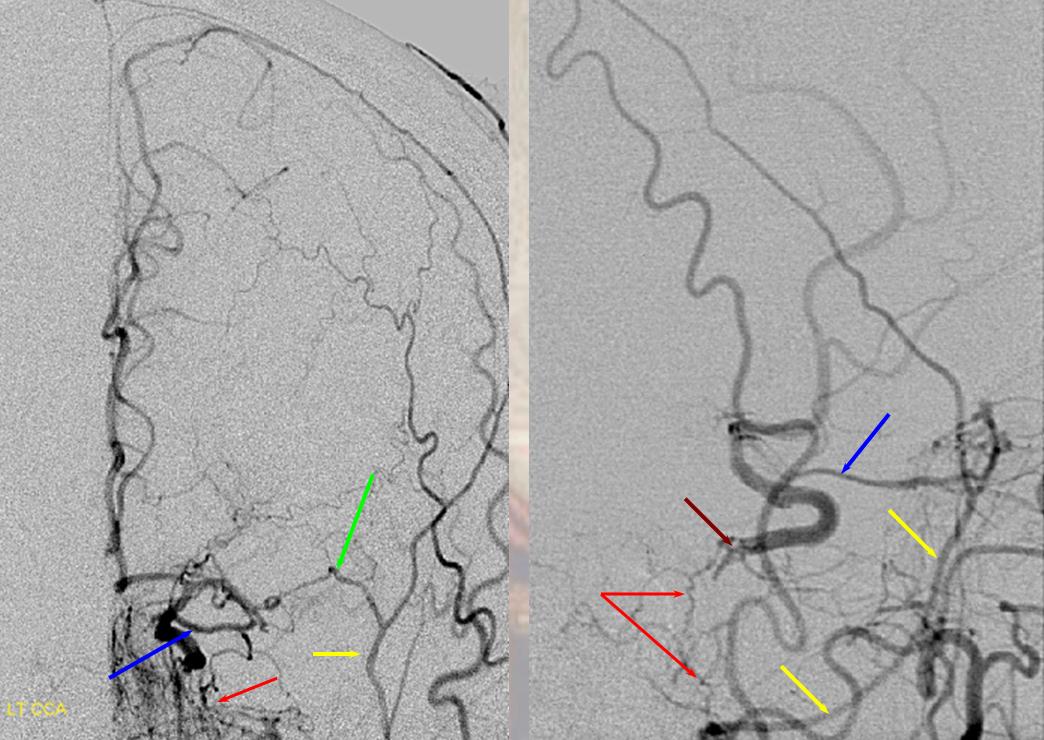
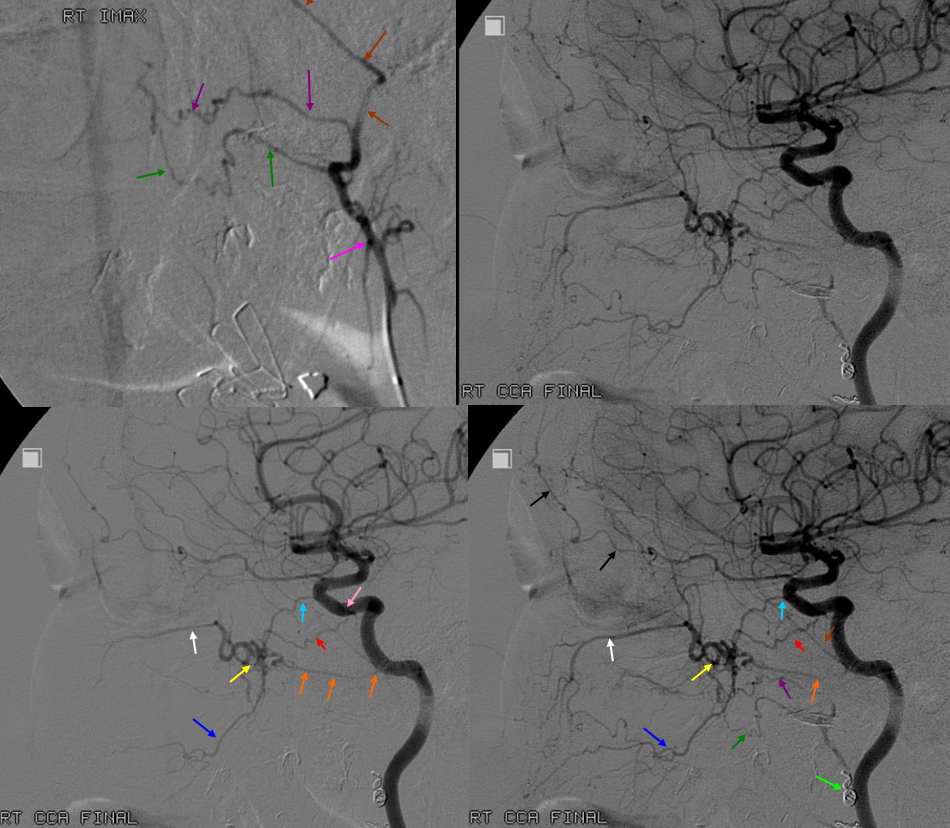
ICA reconstitution following iatrogenic occlusion with coils (orange arrows) The ILT reconsitutes the ICA via sphenoid branches of the MMA (purple), foramen rotundum branch of the IMAX (yellow) and cavernous branches of the Accessory Meningeal (blue) arteries. The patient originally presented with a dural CC fistula. Possibly because the ILT vessels were already enlarged, they were relatively quickly recruited into ICA supply instead of the ophthalmic artery (green) which continues to fill its usual anterograde direction, highly unusual for an ICA occlusion. The coils in the cavernous sinus are also faintly visible in the region between the red and yellow arrows on the lateral projection (see below as well)
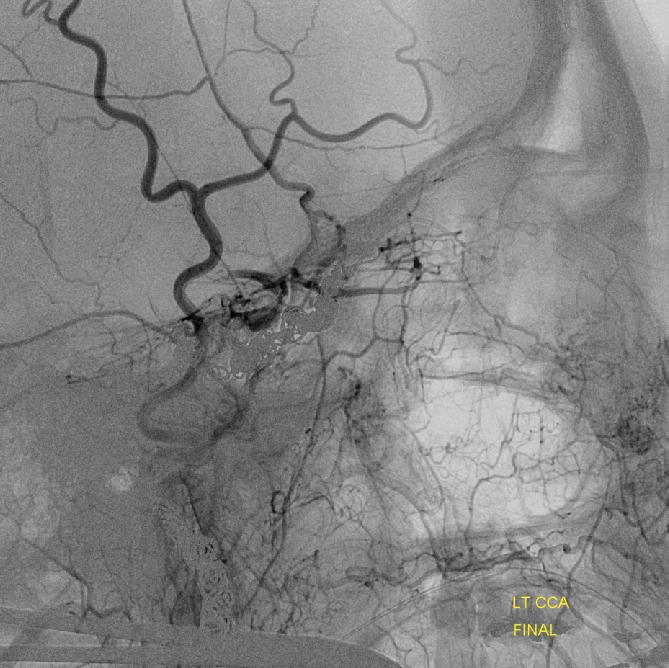
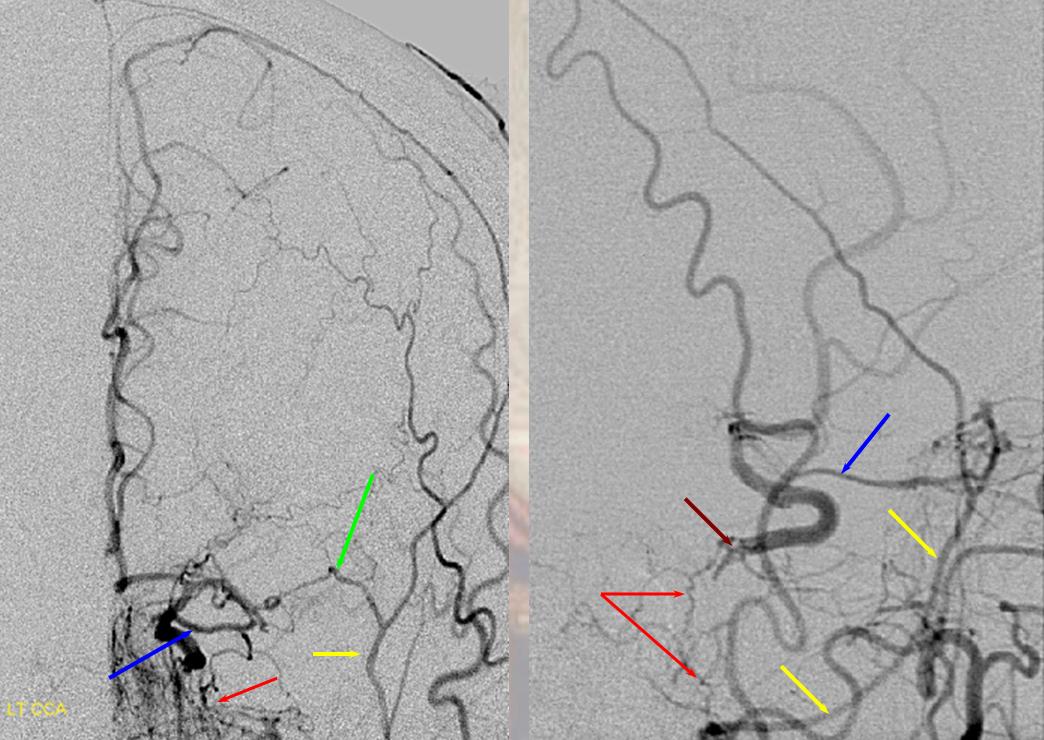
ICA occlusion with ILT and ophthalmic reconstitution. Cavernous branches of the MMA (red) participate in reconstitution of the inferolateral trunk region (brown) The sphenoidal branch (green, best seen on AP and foreshortened on the lateral) of the MMA (yellow) reconstitutes the ophthalmic artery (Blue)
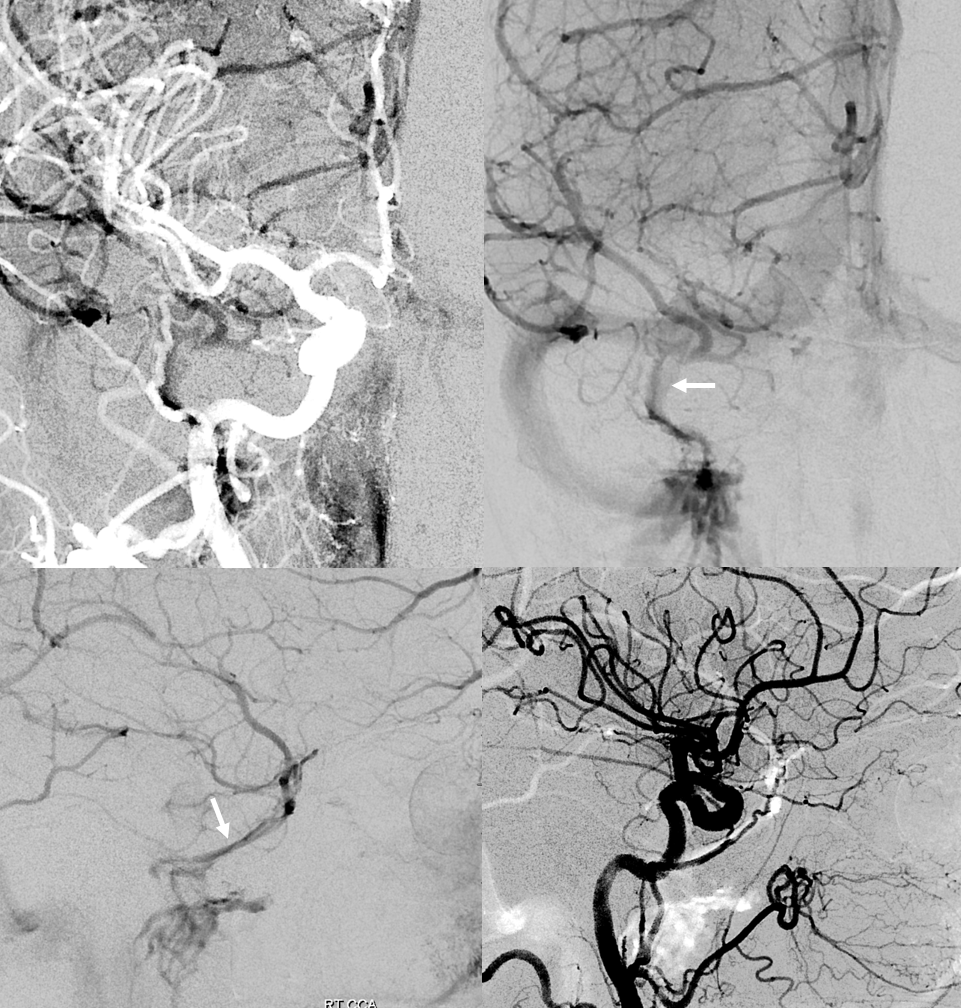
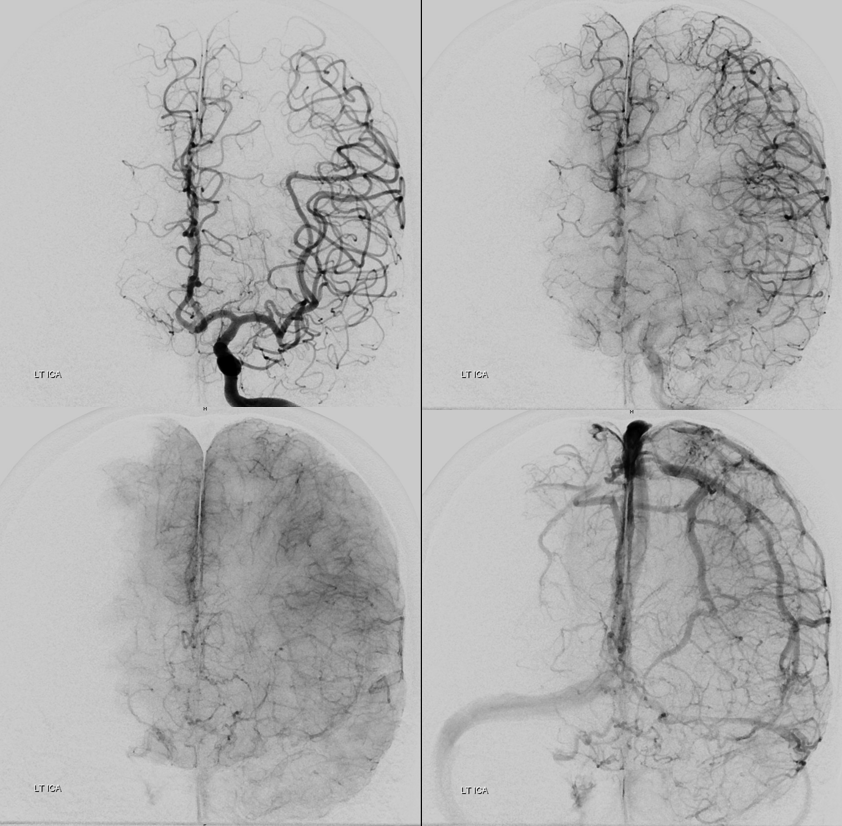
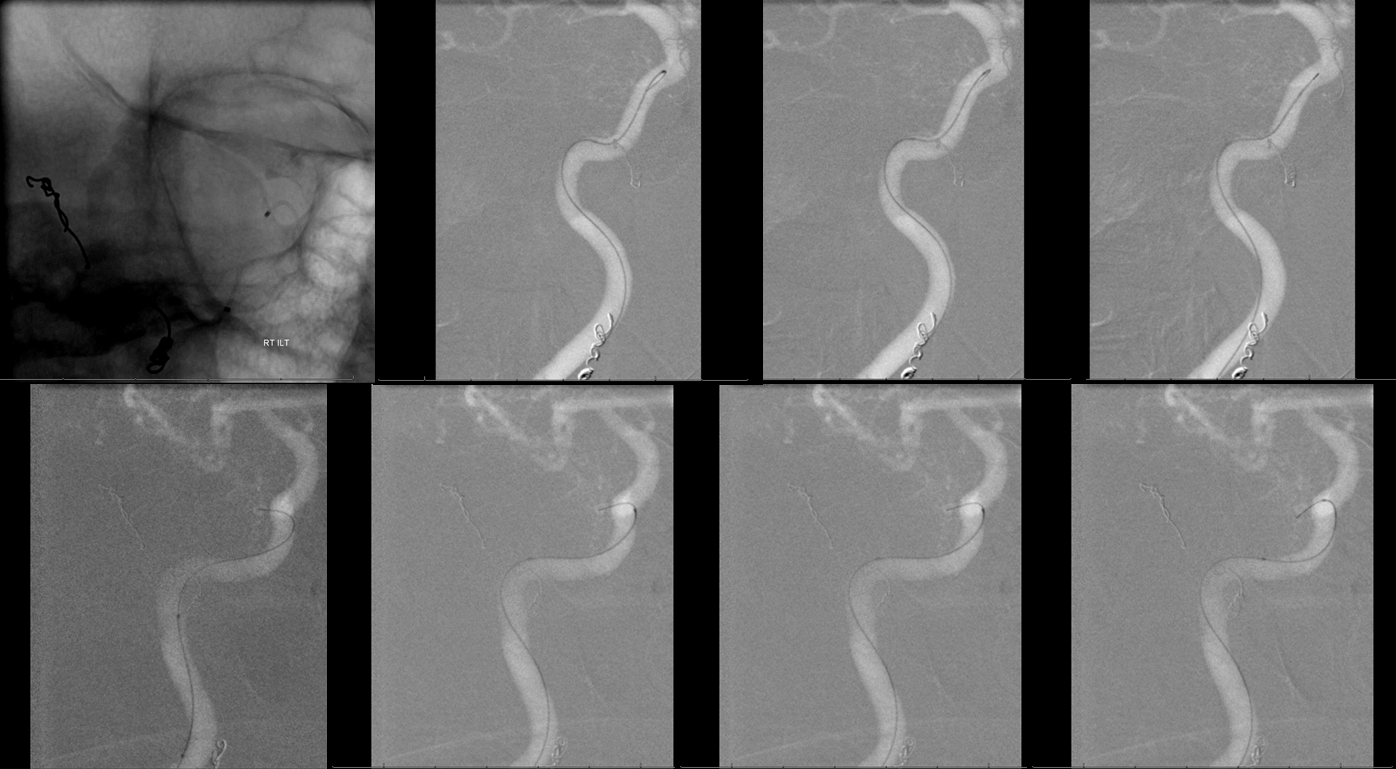
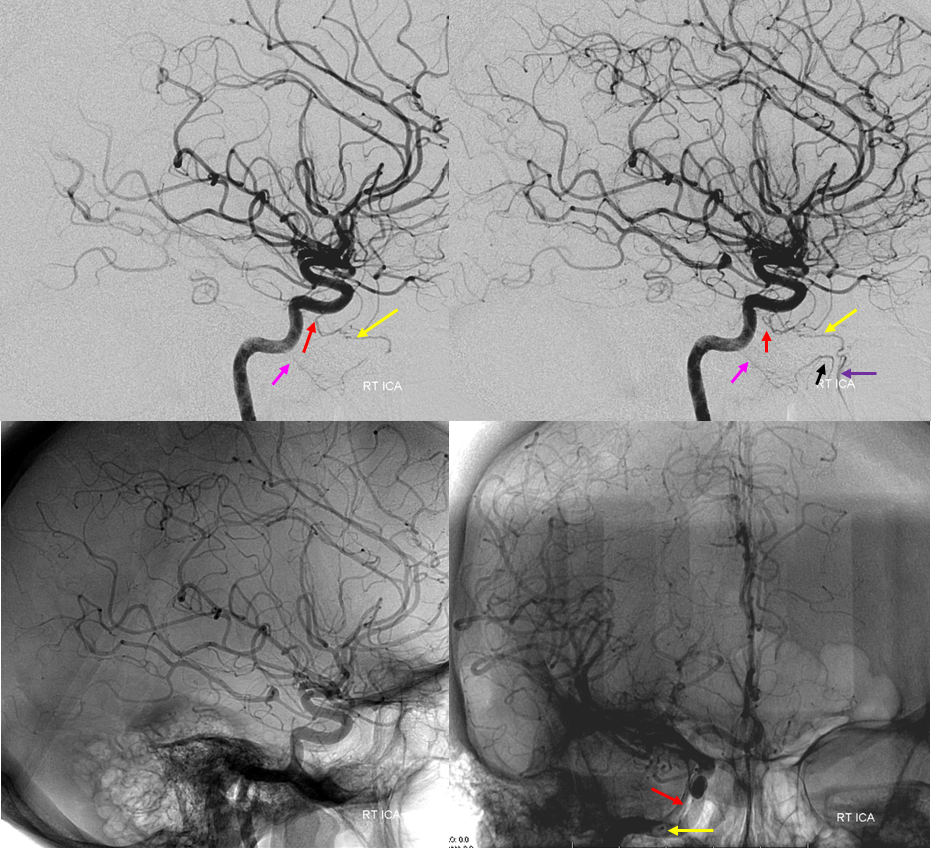
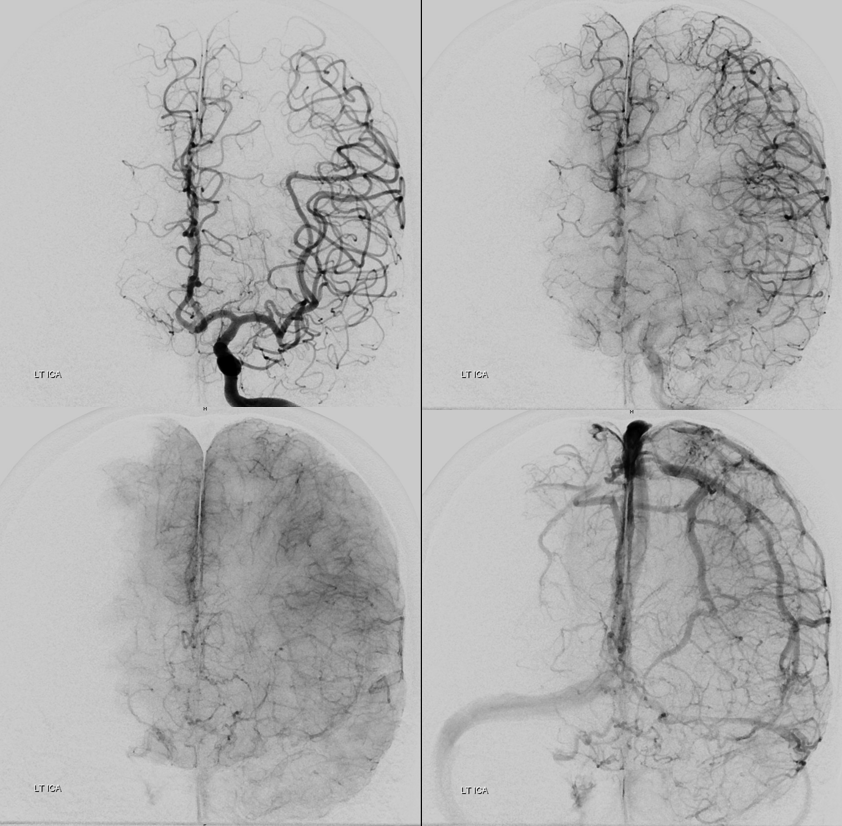
Accessory meningeal reconstitution of the MCA territory via foramen ovale branch — right ICA is occluded at the origin. The ACOM is insufficient. Brisk reconstitution of the MCA territory is afforded via a the accessory meningeal artery inflow via the foramen ovale branches. Additional supply to the cavernous carotid was present via posterior clival branches of the MHT (see MHT). The orbital region is being reconstituted via the MMA.
Red=carotid; purple=extracranial MMA, pink=foramen spinosum; yellow=intracranial MMA; light blue=sphenoidal branch; dark blue=meningo-ophthalmic artery; green=accessory meningeal artery; white=foramen ovale branch of the ILT; brown=carotid stump
ILT flow reversal into ICA to support AVM. Lateral and AP projections demonstrating prominent supply of ILT via accessory meningeal and foramen rotundum branches. The ILT flow is revesed due to presence of a large right frontal AVM. Following embolization (lower right lateral ICA injection), the ILT is now visible off the ICA with normal antegrade flow.
Red=ICA. Purple=ILT. Dark Blue= rotundum. Light blue=foramen ovale branch to the accessory meningeal artery. Yellow=accessory meningeal.
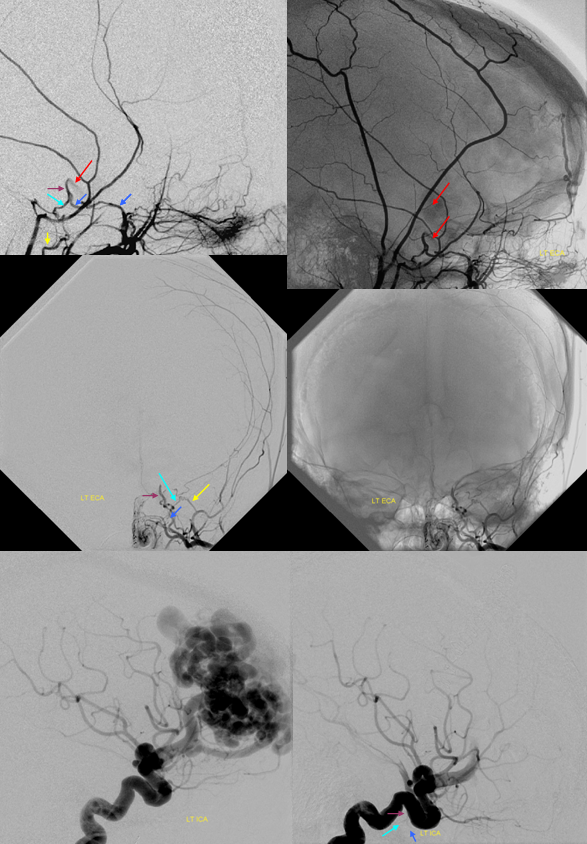
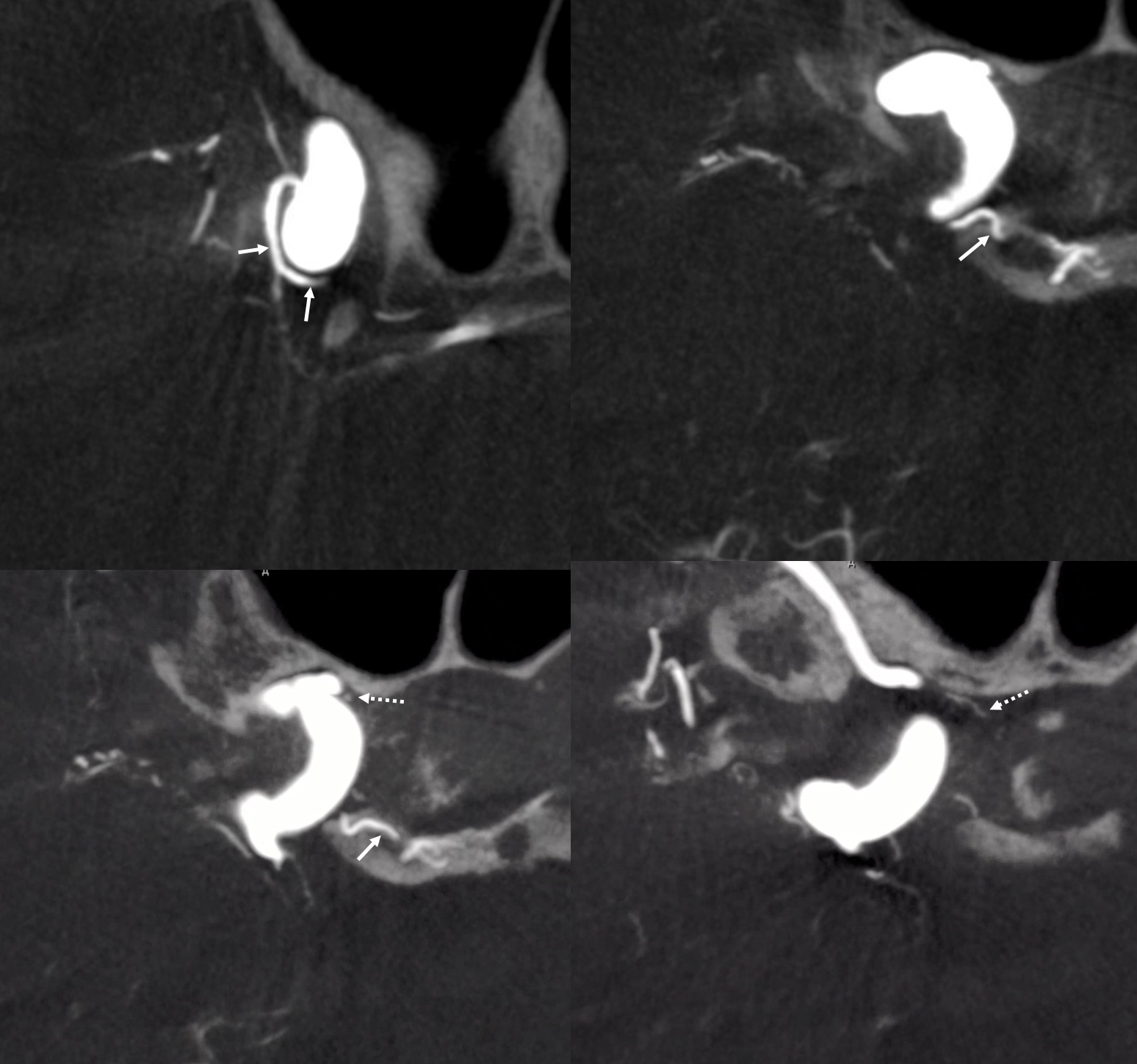
Cavernous Origin of the Ophthalmic Artery — this not so rare disposition corresponds to persistence of embryonic dorsal ophthalmic artery, essentially representing an ILT origin of the ophthalmic. In the usual disposition, the anteromedial branch of the ILT (Figure 1, letter C) represents a vestige of the dorsal ophthalmic. See ophthalmic artery page for additional info
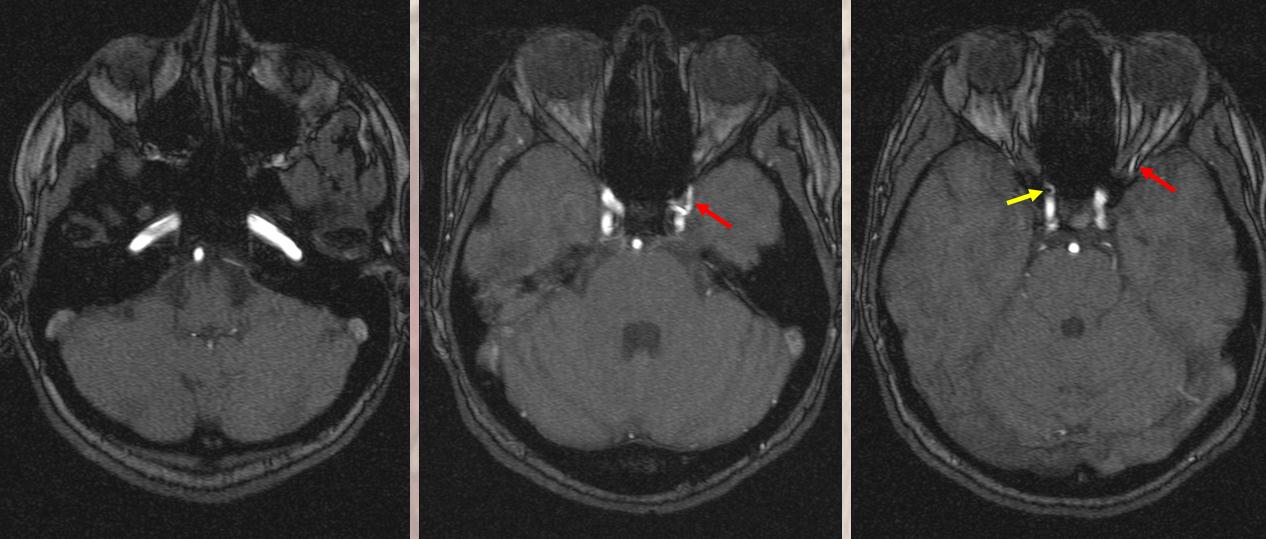
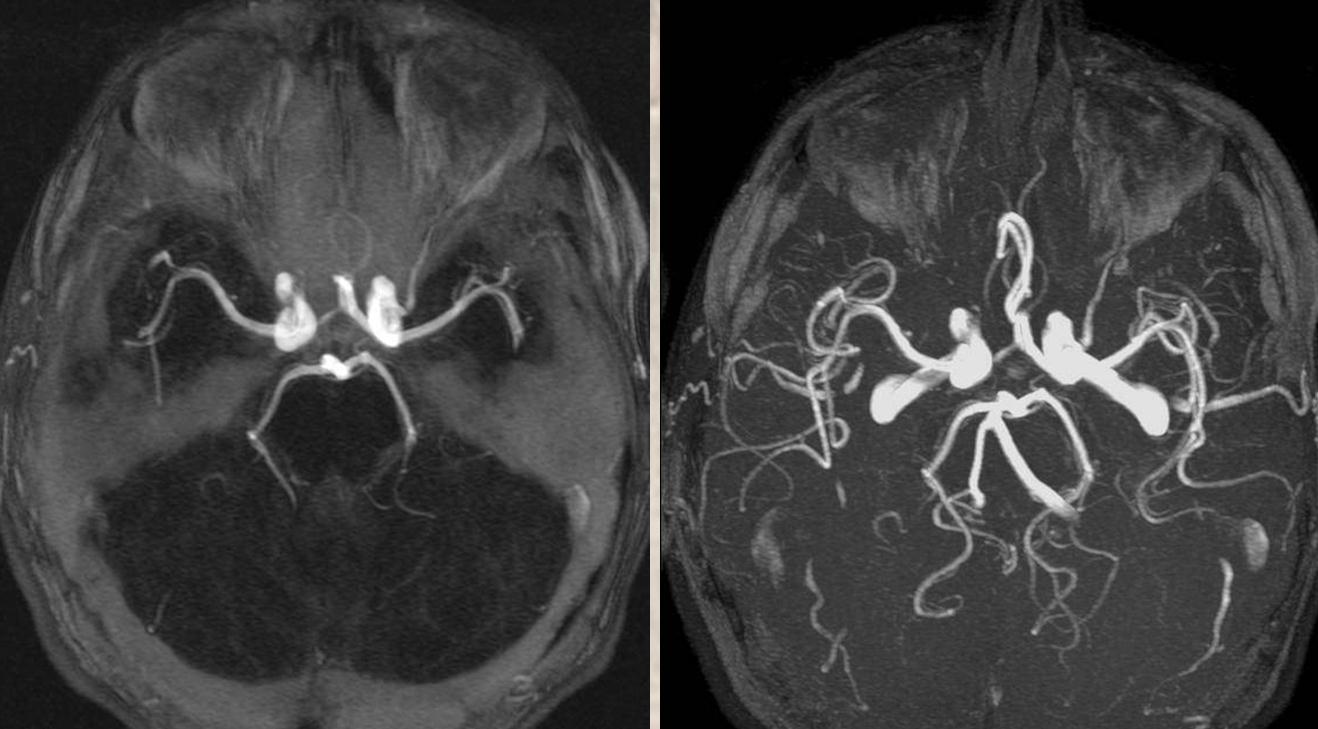
Persistence of dorsal ophthalmic artery. A — site of “classic” ophthalmic artery origin; B — dorsal ophthalmic artery; C — future ILT; D — recurrent meningeal branch of the ophthalmic artery; E — meningo-ophthalmic branch of the MMA
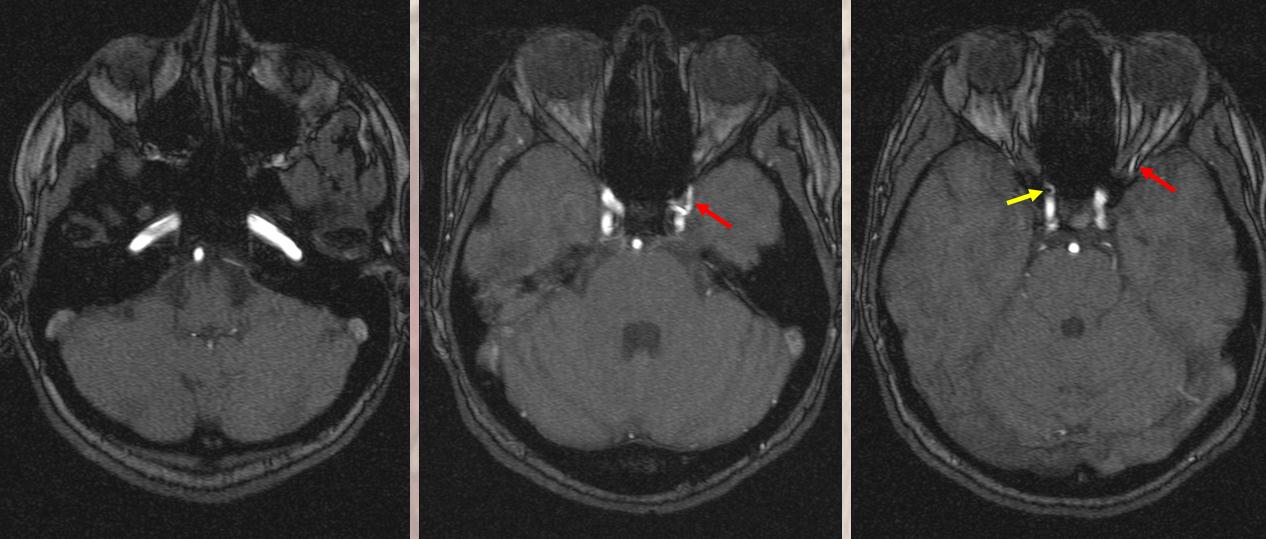
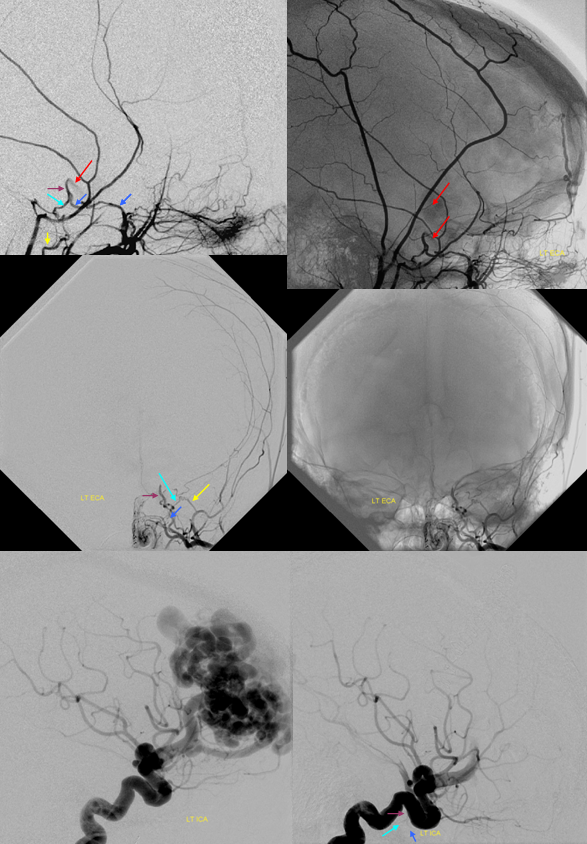
A vessel originates from the lateral cavernous portion of the left carotid artery corresponding to location of the ILT and enters the orbit (red arrows). The right ophthalmic artery origin (yellow) is normal. Average (left) and MIP (right) projections of the same case are seen below.
Similar case on angio of ophthalmic artery origin off the ILT
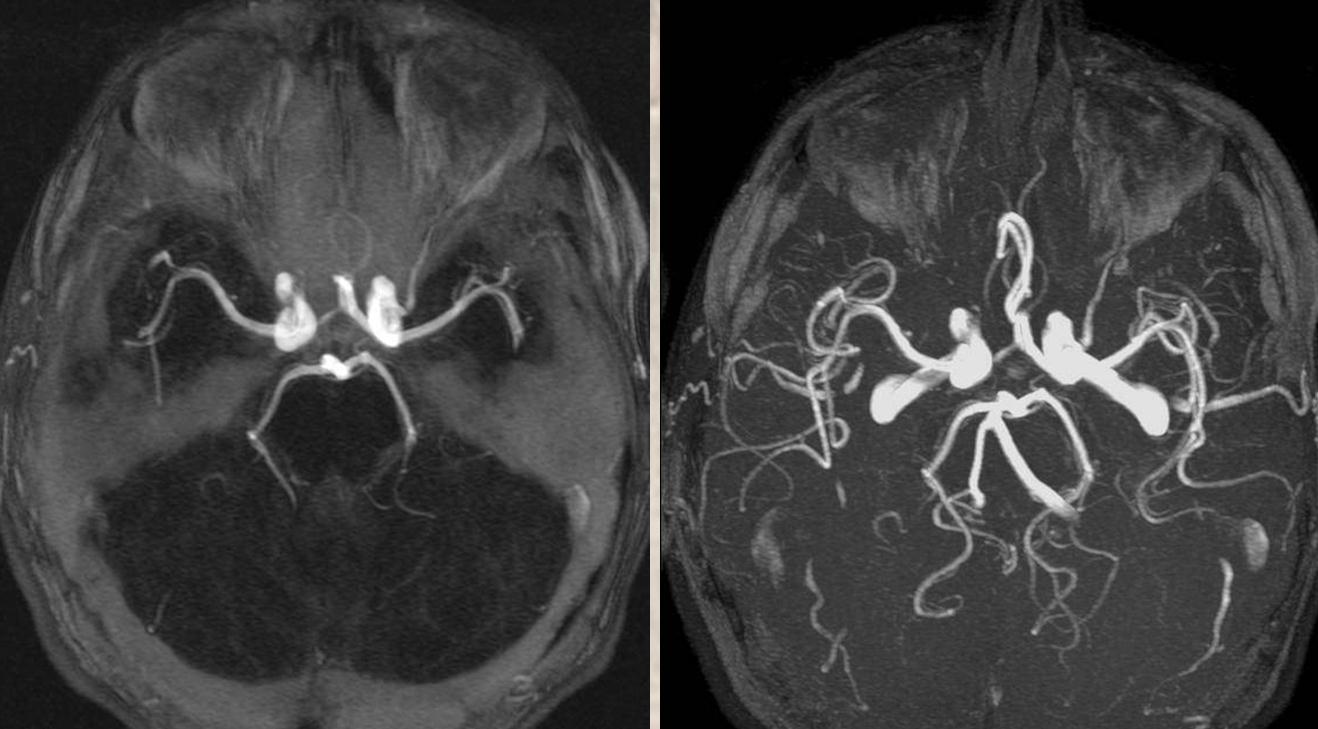
Left ICA injection shows a very large dorsal ophthalmic artery — embryologically this is the same as the anteromedial branch of the ILT.
Cross-eye stereos
Anaglyph stereo
VRs, showing a another branch of the ILT/dorsal ophthalmic (black arrows)
Dyna CT axial views trace the dorsal ophthalmic (white arrows) through the superior orbital fissure. The smaller branch (black) also traverses the superior orbital fissure to enter the orbit more laterally — perhaps a lacrimal branch
Anaglyph VR stereo
See Ophthalmic Artery Page for more info
“Duplicated” ILT — main trunk usual territory, smaller one free margin artery
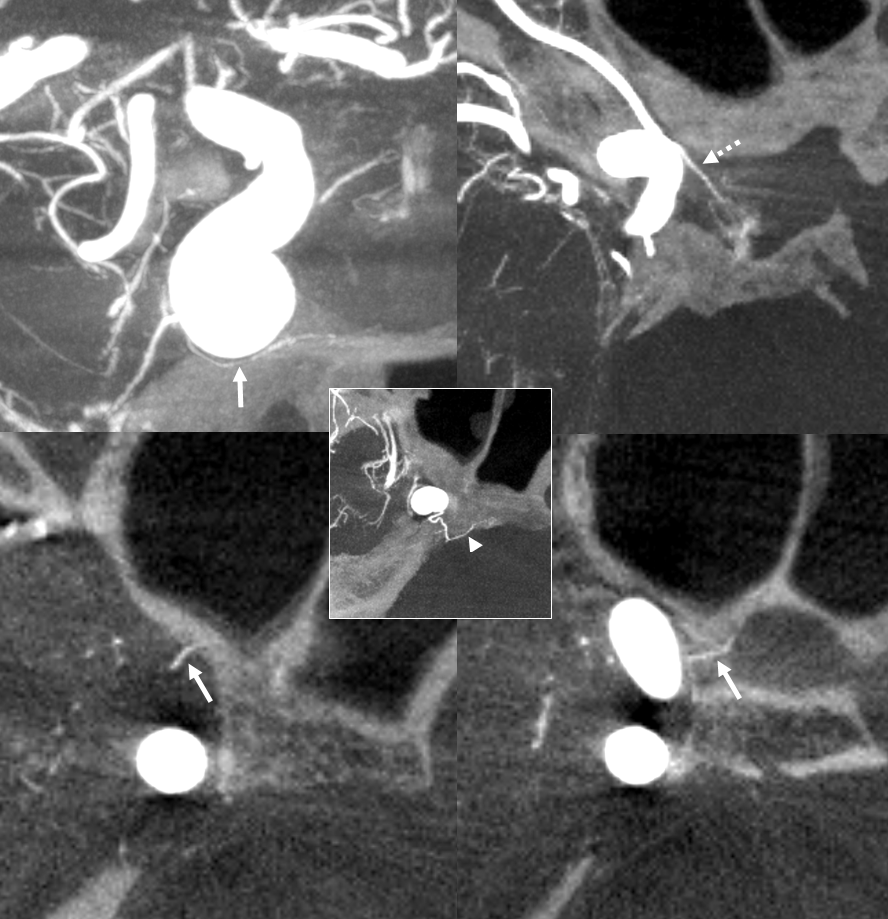
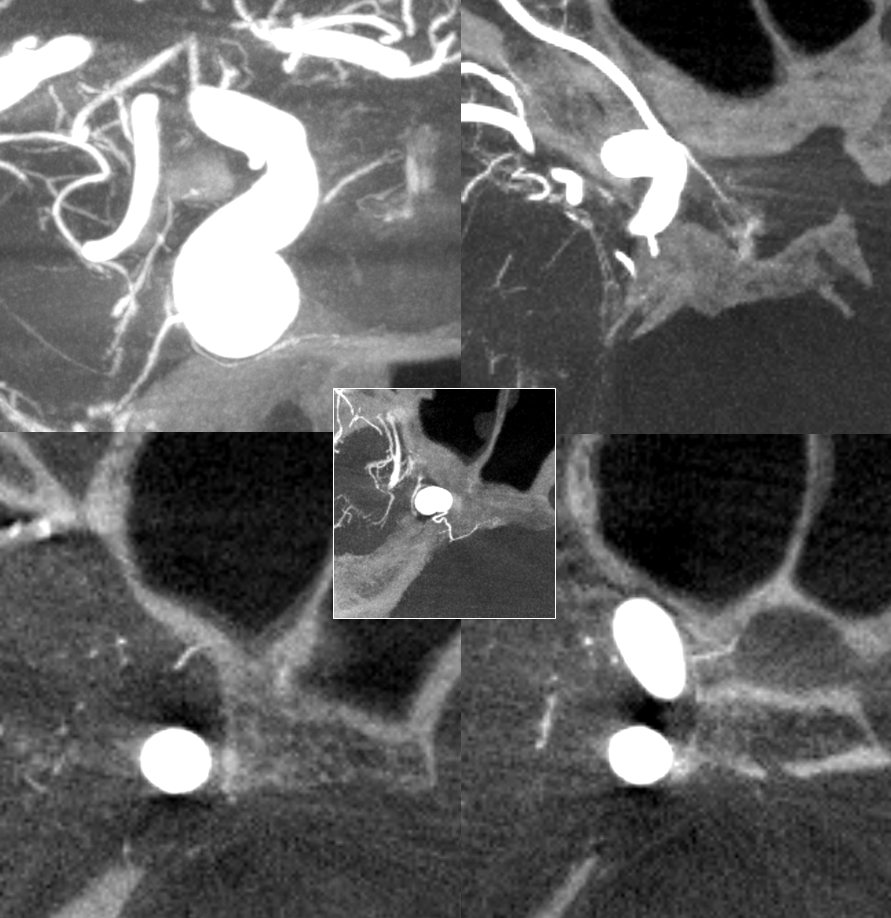
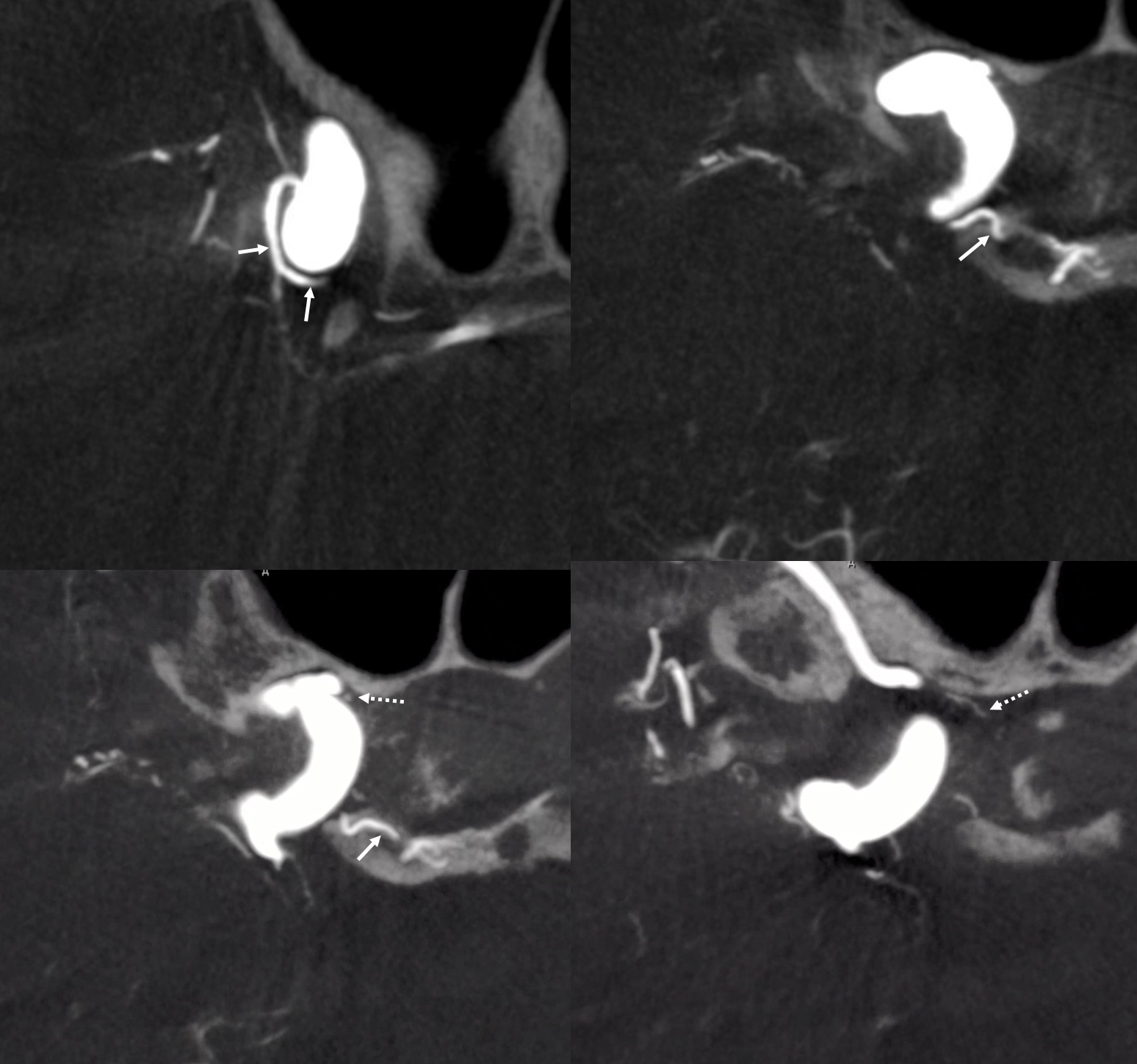
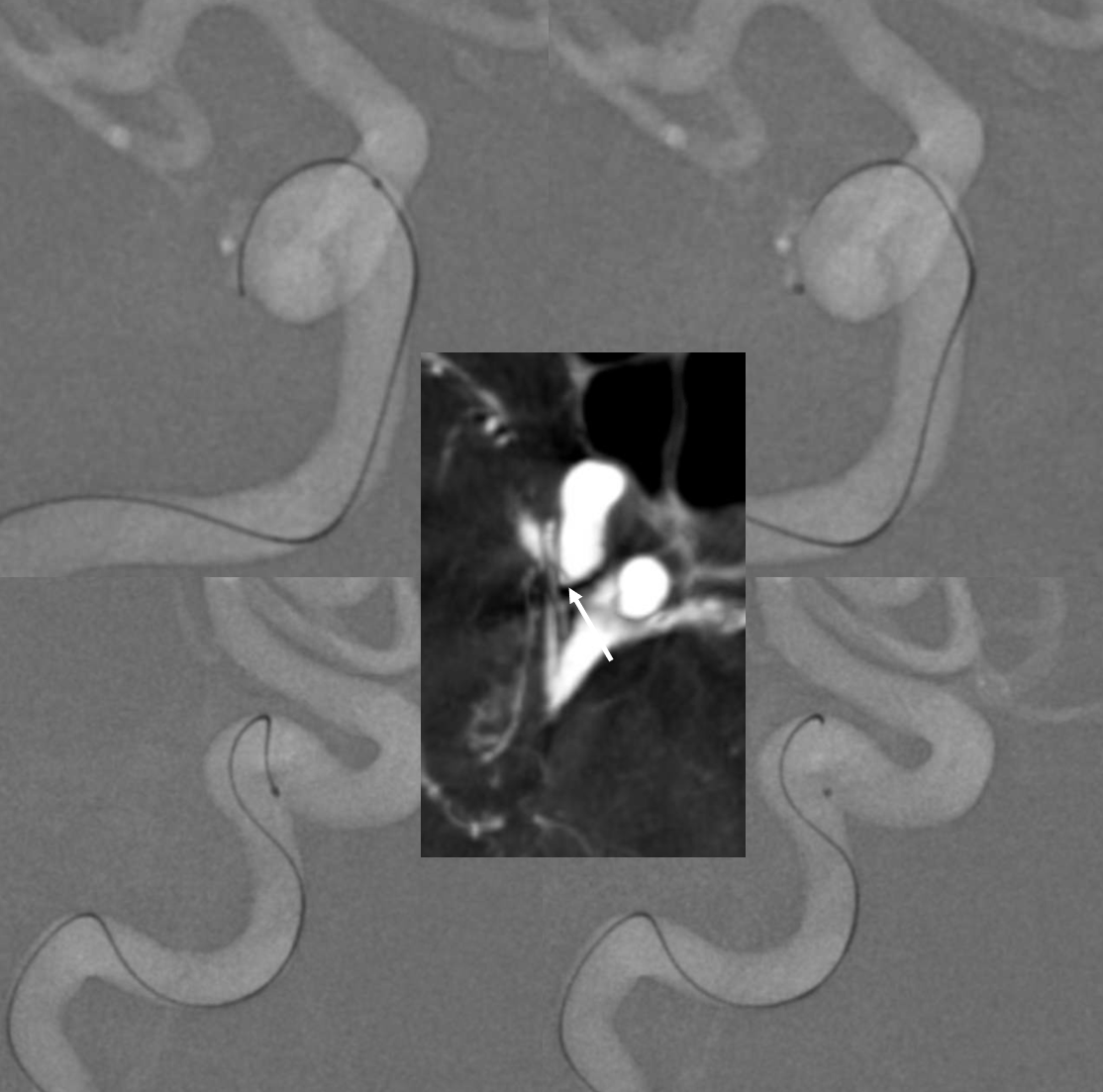
ILT Supply of the Pituitary
Very rare. ILT branch (arrows) passing underneath the ICA supplies anterior pituitary, and is in balance with the superior hypophyseal branch (dashed arrow) and inferior hypophyseal branch (arrowhead, inset)
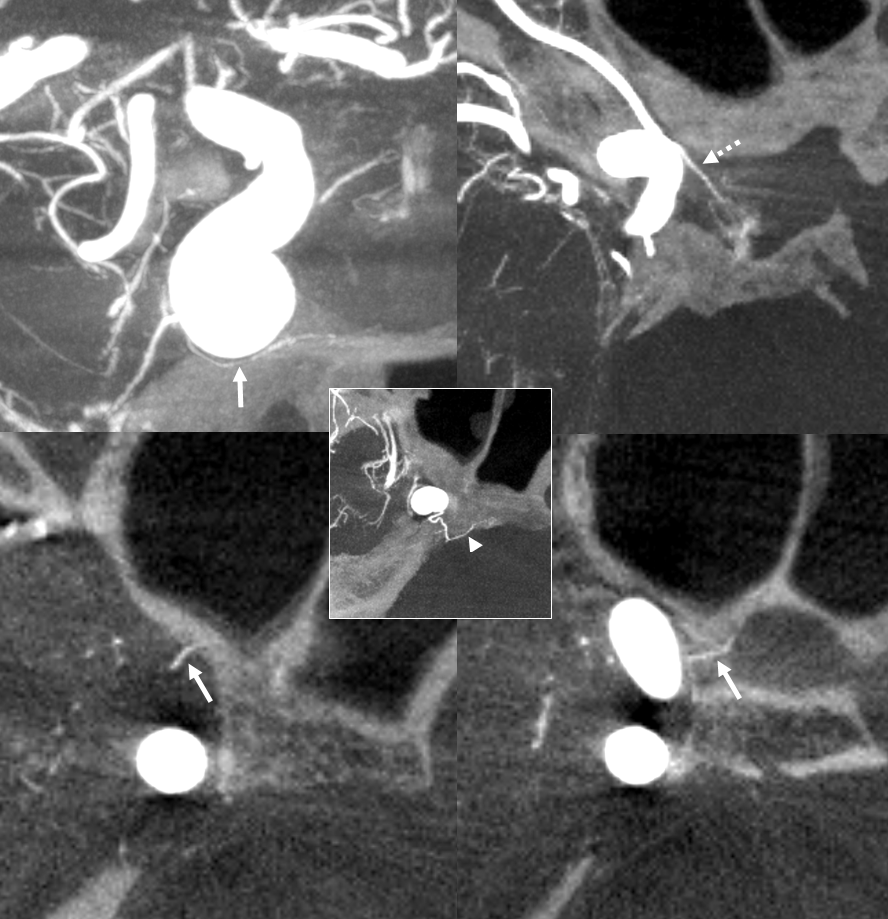
No arrows
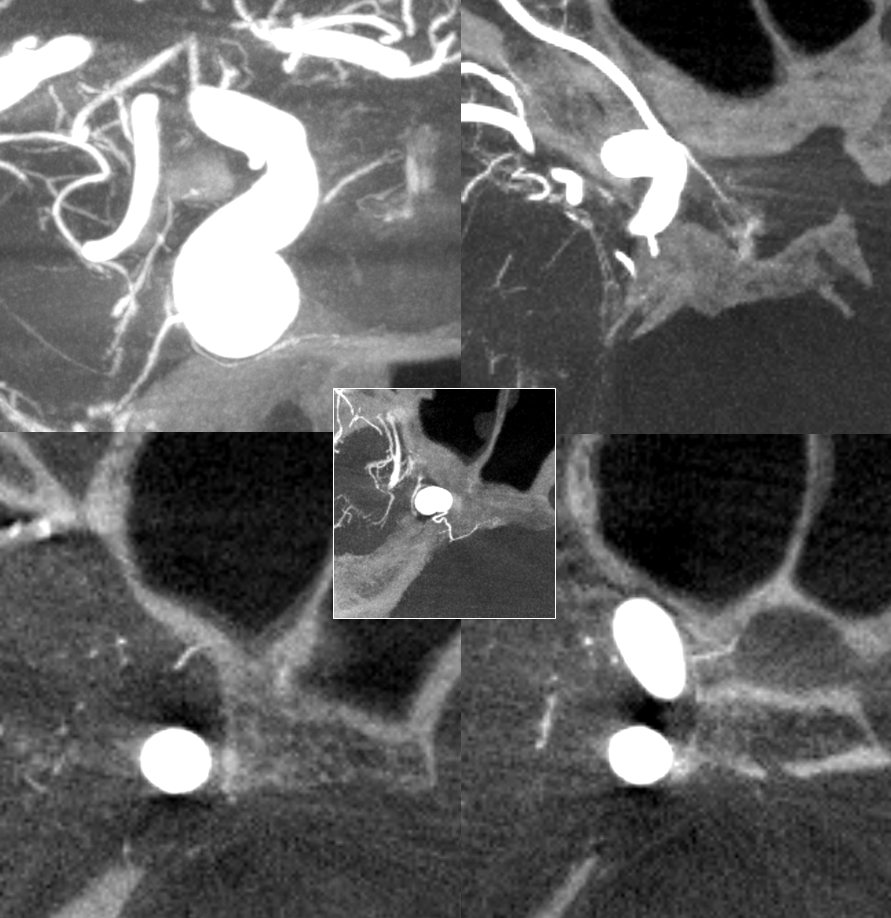
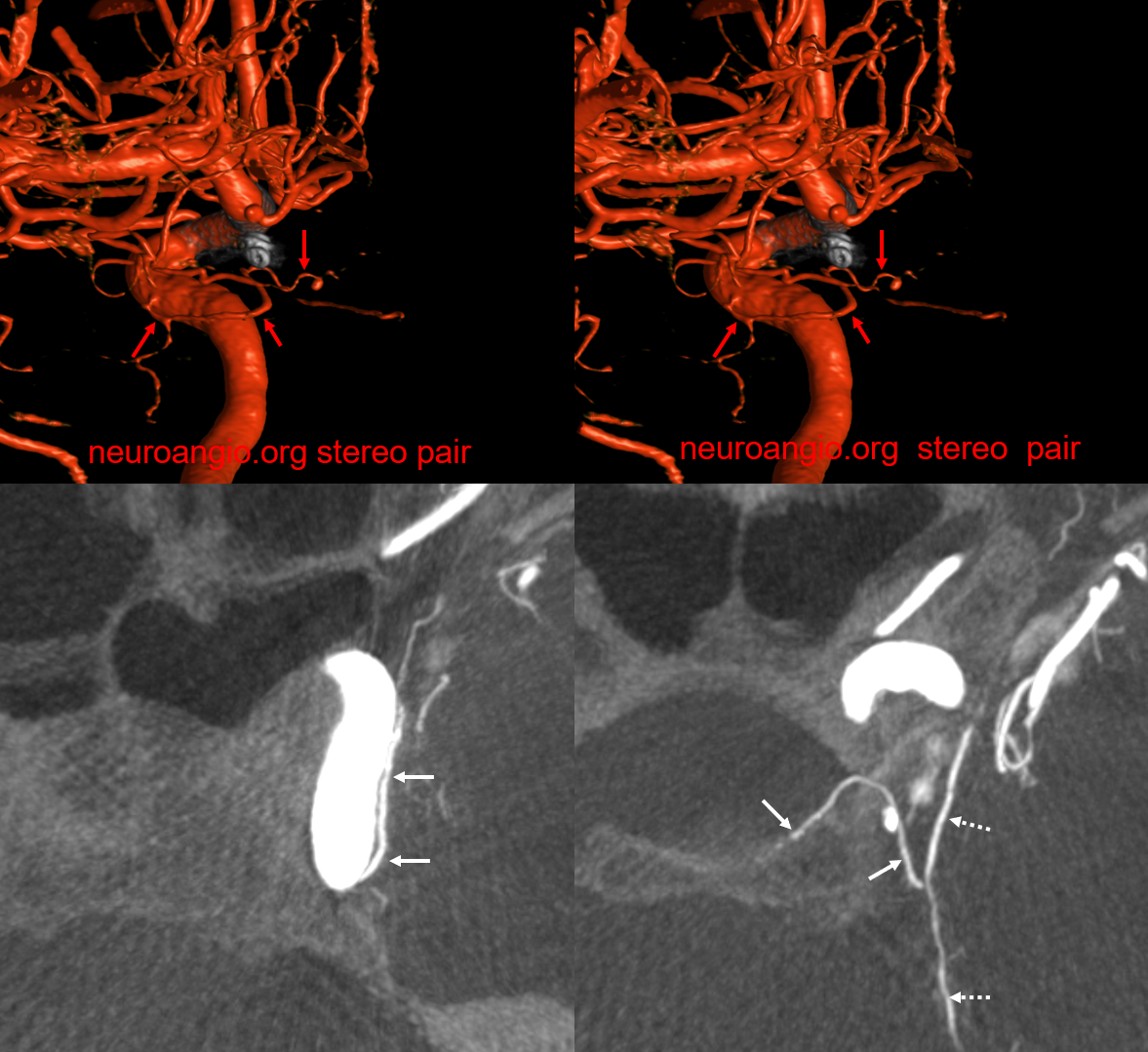
ILT Supply of Pituitary — Hypoplastic MHT
Again, the ideas of spectrum and balance. If MHT is hypoplastic, something else has to do the work. In this very rare case, the ILT supplies posterior pituitary (via the tentorial branch) due to MHT hypoplasia.
MIPS — ILT is arrows. Also present is superior hypophyseal artery (arrowheads) supplying anterior pituitary.
Another nice example below. The inferior hypophyseal (solid arrows) is seperate from the tentorial arcade, which extends from the ILT to the marginal tentorial area (dashed arrows).
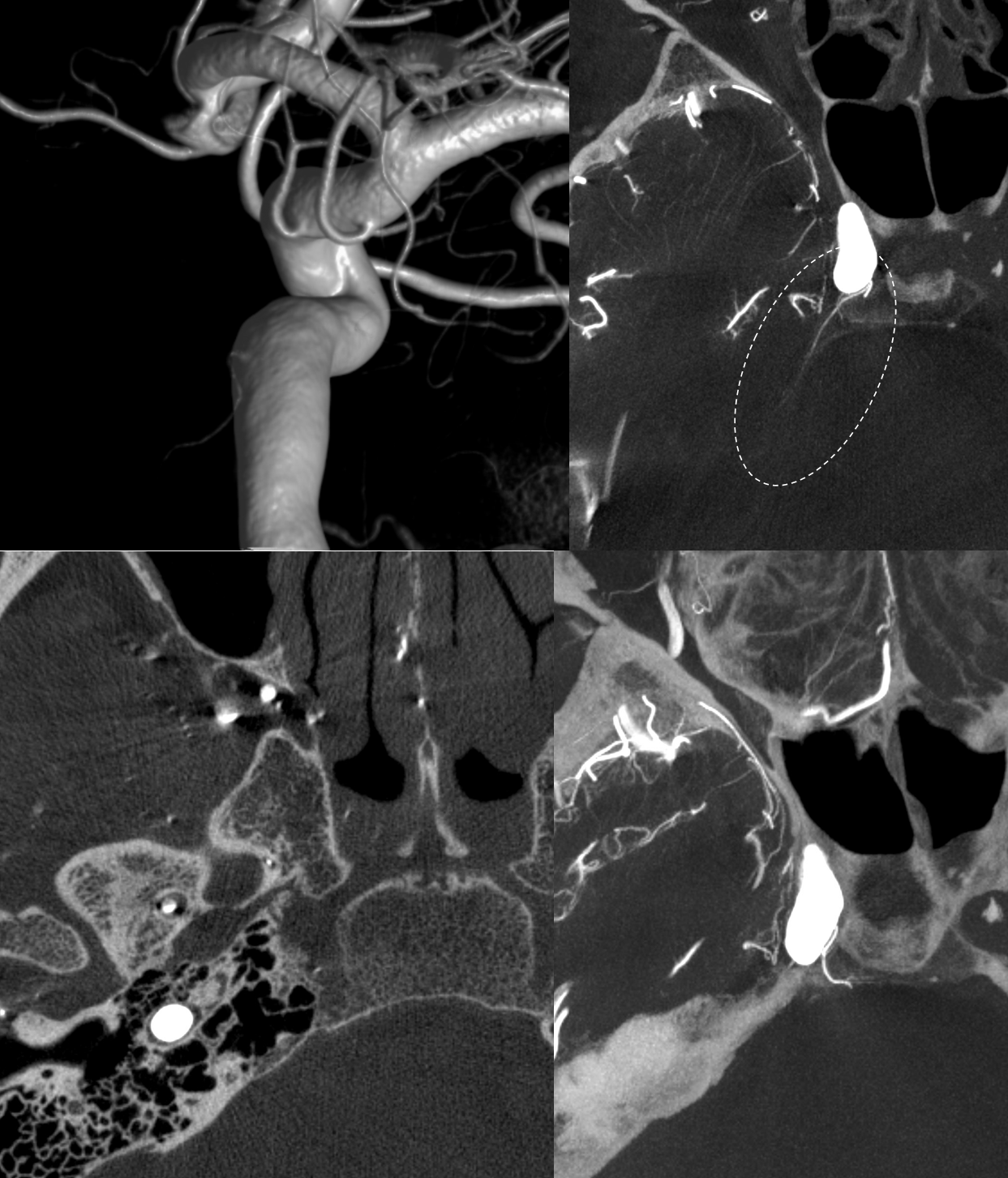
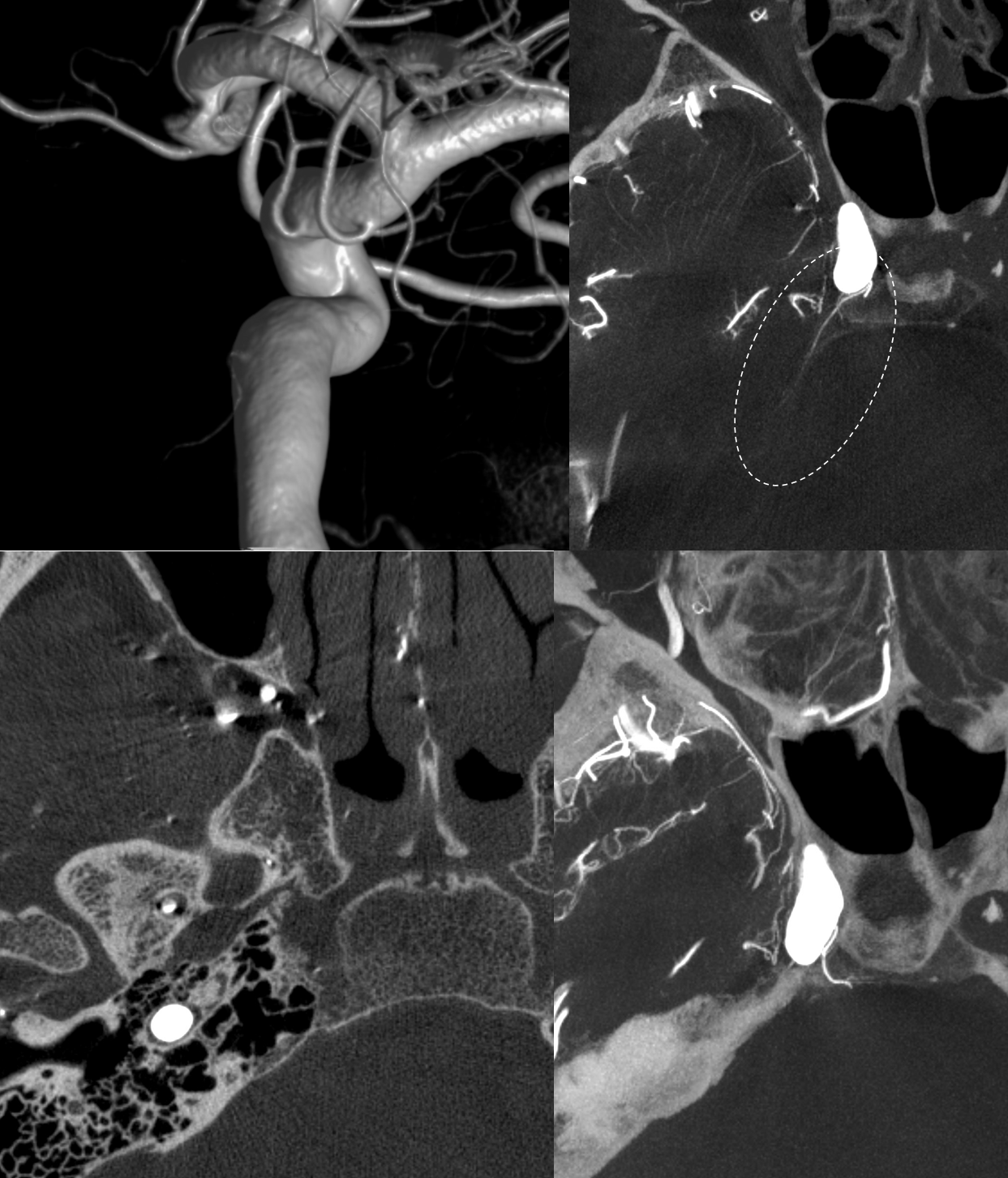
Hypoplastic ILT and MHT — Accessory Meningeal Supply
Just because its an ILT page doesnt mean we dont talk about its absence. Sometimes its hypoplastic. MHT and others will pick up slack… Here ILT is MIA, and MHT is smallish but does supply lateral tentorial arcade (dashed oval). The ILT area is supplied by accessory meningeal, here entering skull through foramen of Vesalius
ILT supply of the marginal tentorial arcade
Again, balance. The marginal tentorial is usually a branch of the MHT. However, the ILT can supply this territory via the “deep recurrent meningeal” artery — also known as marginal clival artery — also known as number 43 in the diagram above — the recurrent branch of the ILT. This is the same way that ILT can be connected with the Trigeminal artery. Sagittal MIP below shows continuation of the marginal tentorial artery as artery of the straight sinus
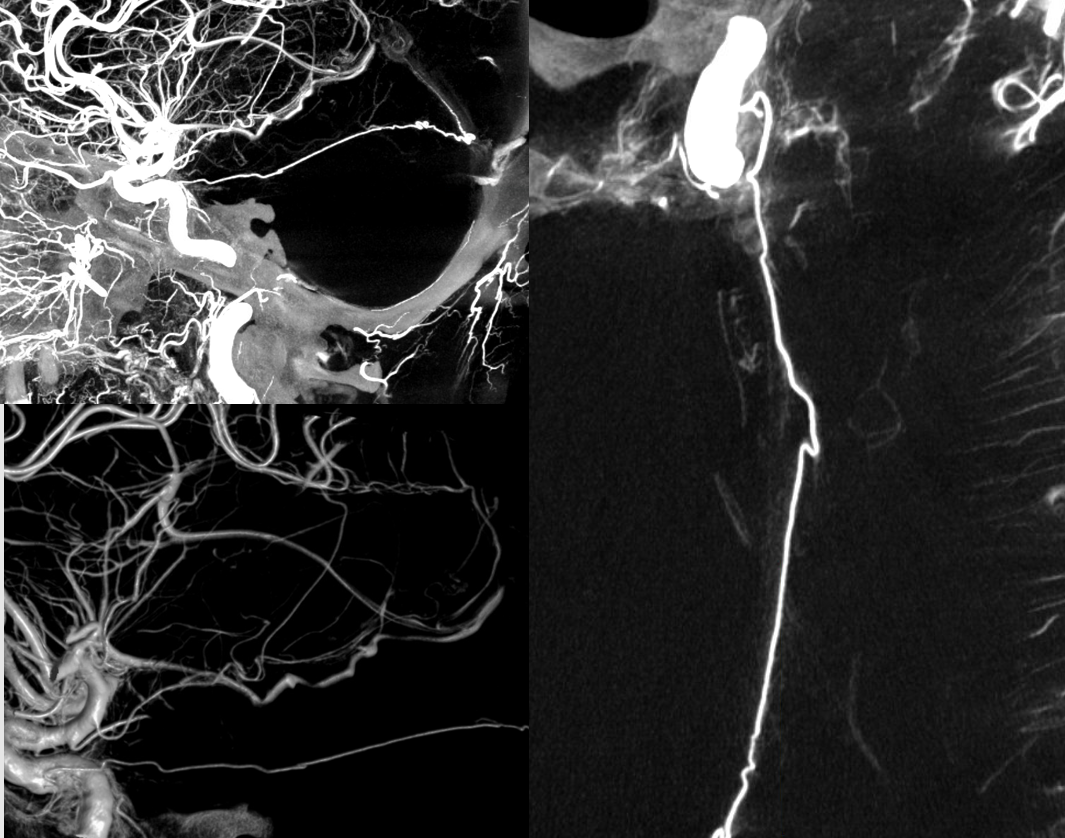

The promiment marginal tentorial continues as the artery of straight sinus. Lest you think that this is only DYNA type image. See angio below
Can u see it on frontal views?
ILT and mandibulovidian reconstitution of IMAX territory
Foramen rotundum branch and other branches are commonly recruited for IMAX reconstitution of ICA in setting of proximal occlusion. The reverse may also take place following occlusion of the proximal IMAX, whereby the ILT feeds into the terminal IMAX in the pterygopalatine fossa. Typically, the facial artery is a much more robust candidate for reconstitution, so for ILT to become recruited the facial artery usually must be MIA as well. This is the case here, as the patient has had multiple surgeries for mandibular malocclusion and other issues. The upper left ECA injection demonstrates occlusion of the distal ECA trunk (pink) with reconstitution of the distal IMAX via two collateral branches (dark green and purple). The earlier (bottom left) and later (bottom right) images status post coiling of the ECA (bright green) demonstrate robust reconstitution of the pterygopalatine fossa IMAX (yellow) via foramen rotundum (light blue) and foramen ovale (red) branches of ILT (cream), as well as from the mandibulovidian artery (orange). The sphenopalatine (white) and descending palatine (blue) branches of the IMAX supply the palate and nasal mucosa and extend quite anteriorly on the later phase image. Also note reconstitution of the Middle Meningeal Artery (brown) via retrograde flow thru the above-mentioned IMAX channels (purple and dark green) into the ECA above the coils (pink). Incidentally noted is presence of a prominent anterior meningeal artery (black) arising from the ophthalmic artery.
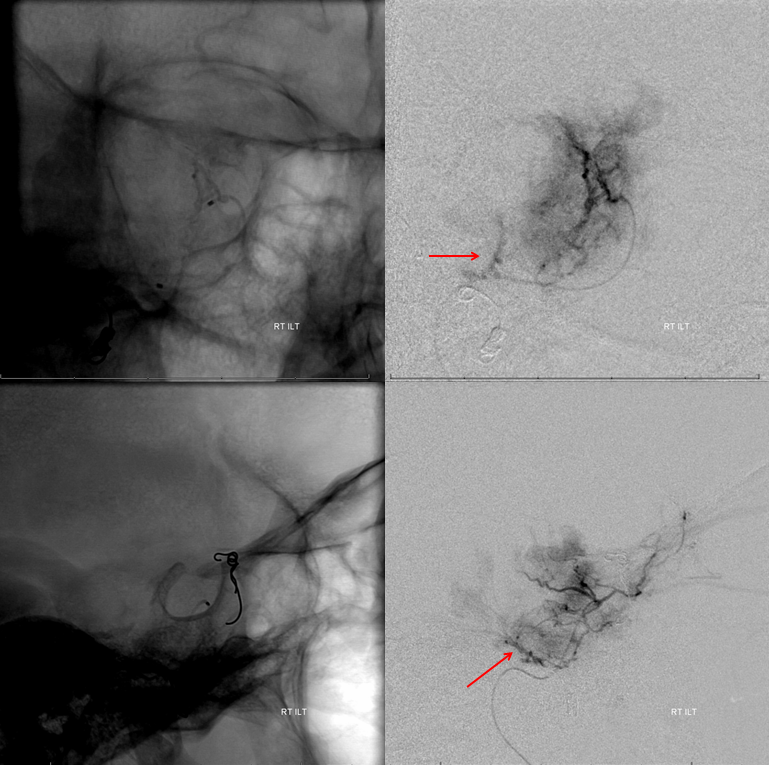
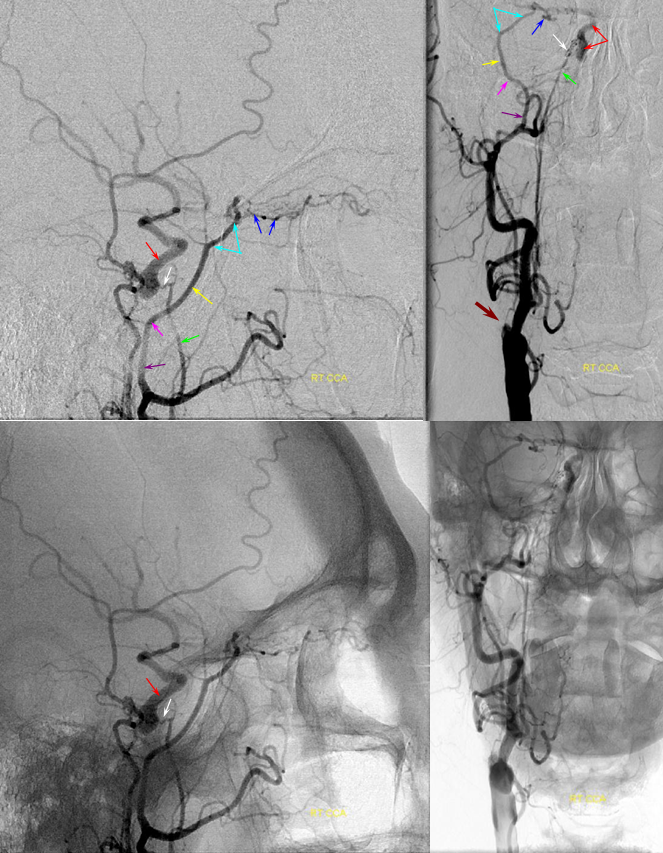
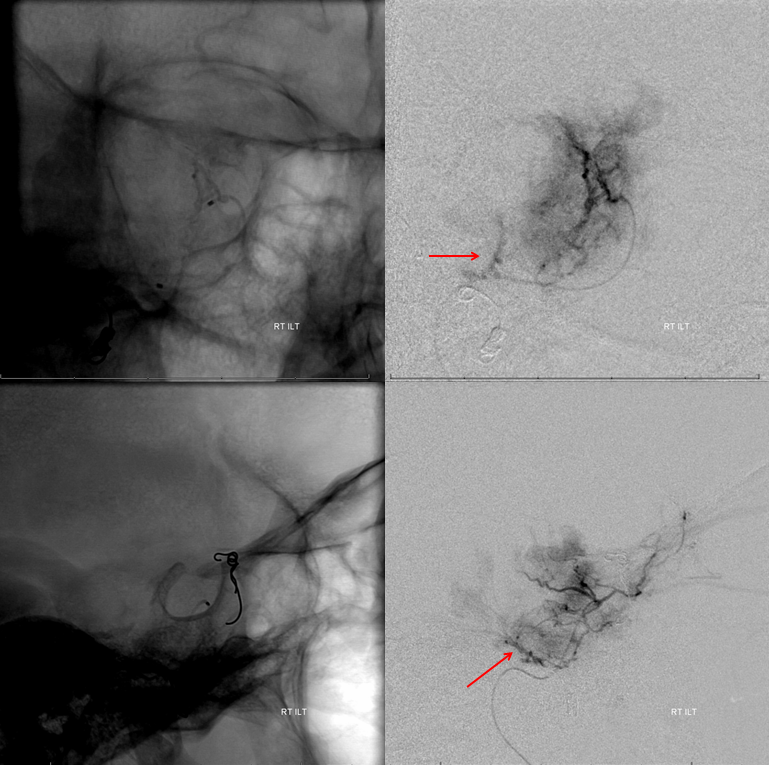
Pathology — tumor embolization
The ILT is frequently involved in supply of nearby meningiomas, which include sphonoid ridge, petroclinoid, and cerebellopontine angle types. Approaches to these vary widely, from no preoperative embolization, to extracranial embolization with various agents to, rarely, intracranial embolization. Our approach is, whenever possible and useful, to perform intracranial embolization through MHT and ILT, as dictated by supply, with small PVA Contour particles. Some examples of ILT access for meningioma embolizations are here. We find steam-shaping the marathon to about 45 degrees to be particularly helpful for getting into this rather inconvenient branch
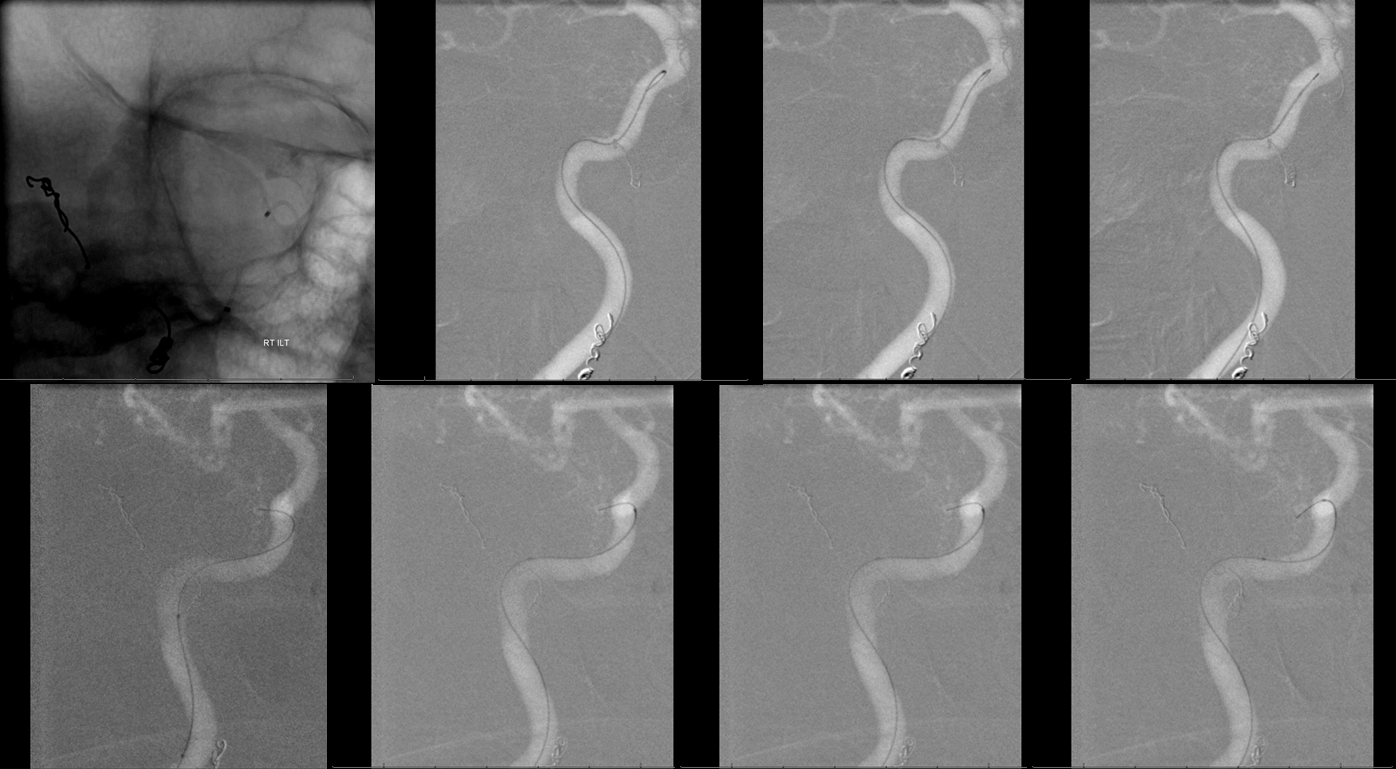
Proximal origin of ILT
Here is another tumor embo — and showing that ILT sometimes arises quite proximally along the horizontal cavernous segment
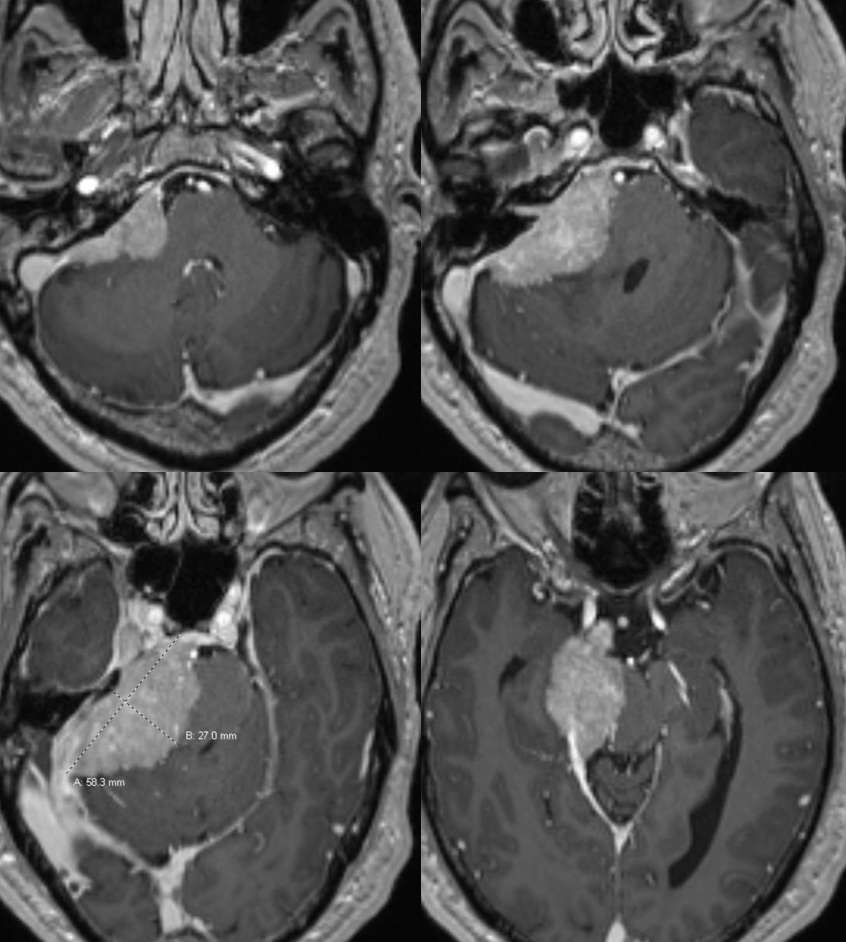
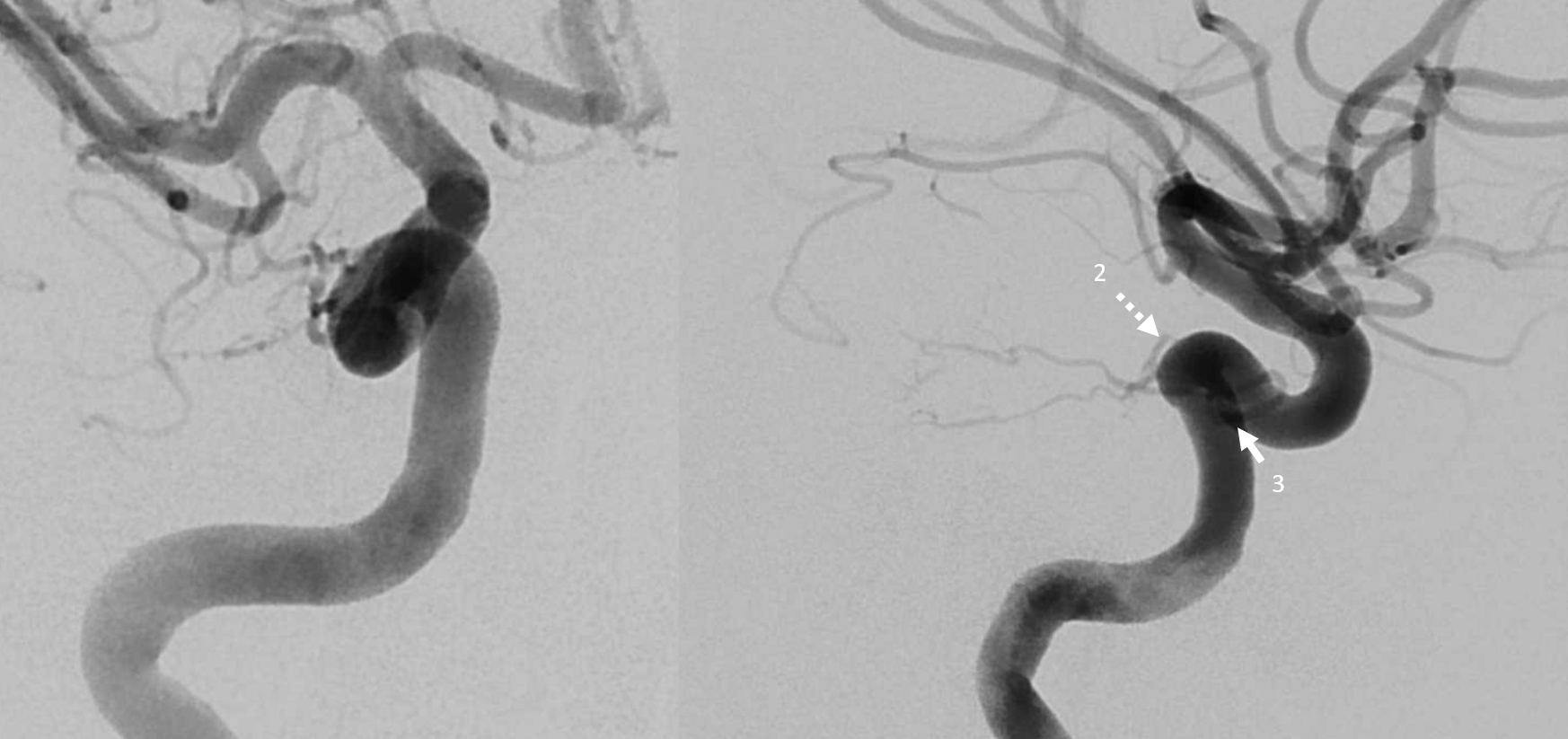
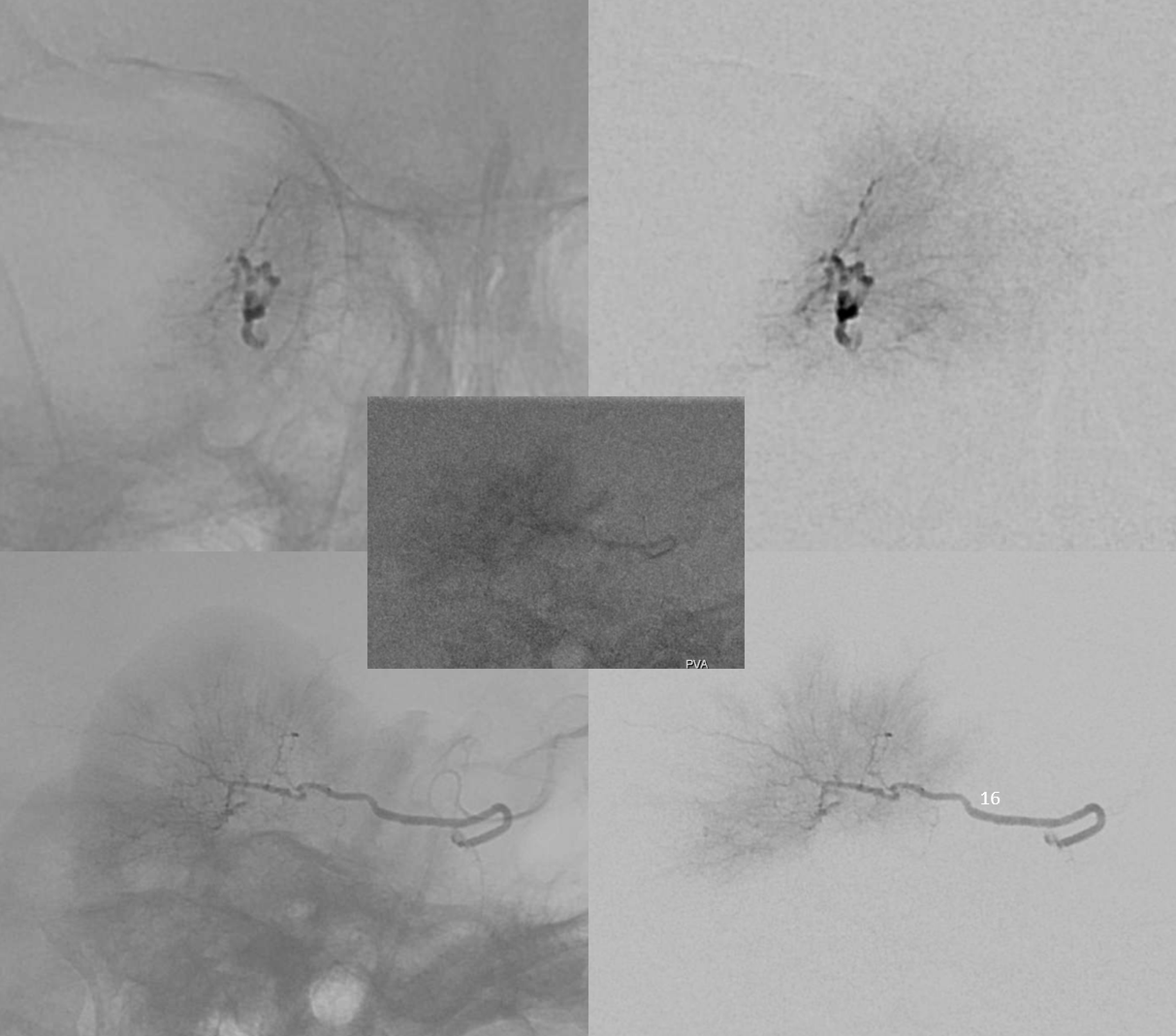
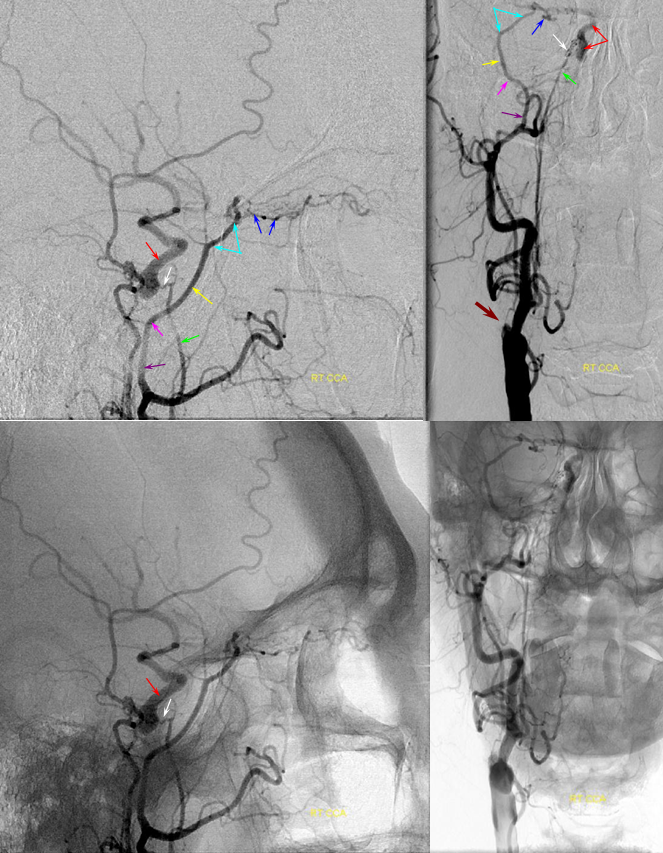
Big CPA mening
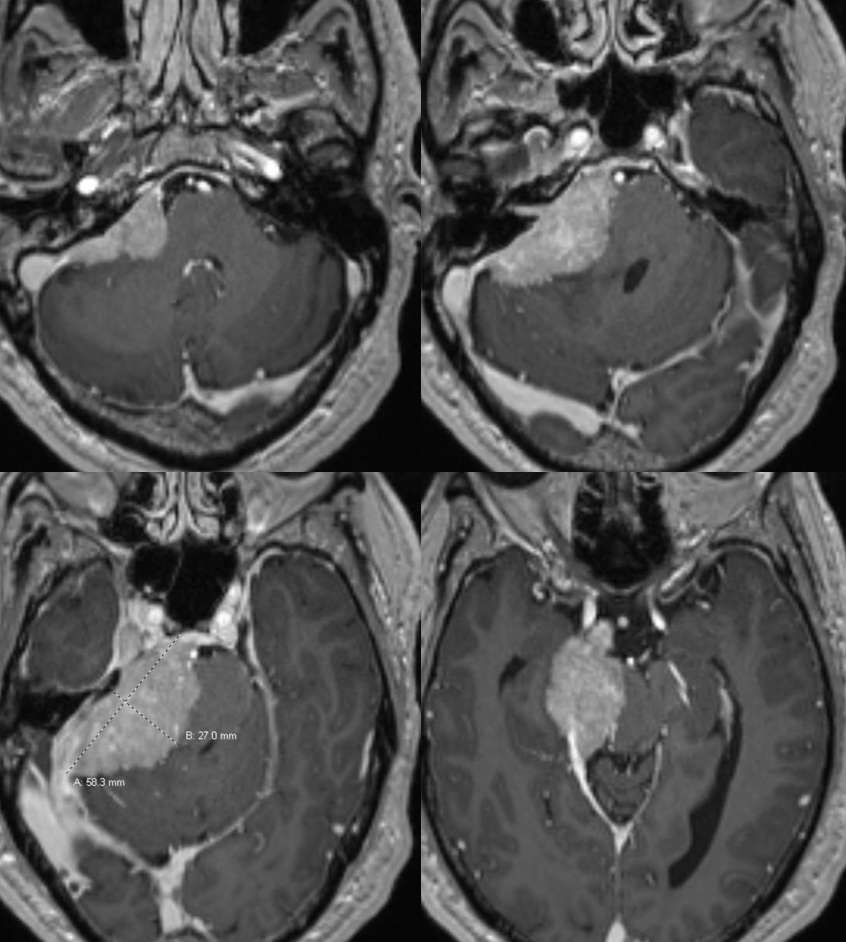
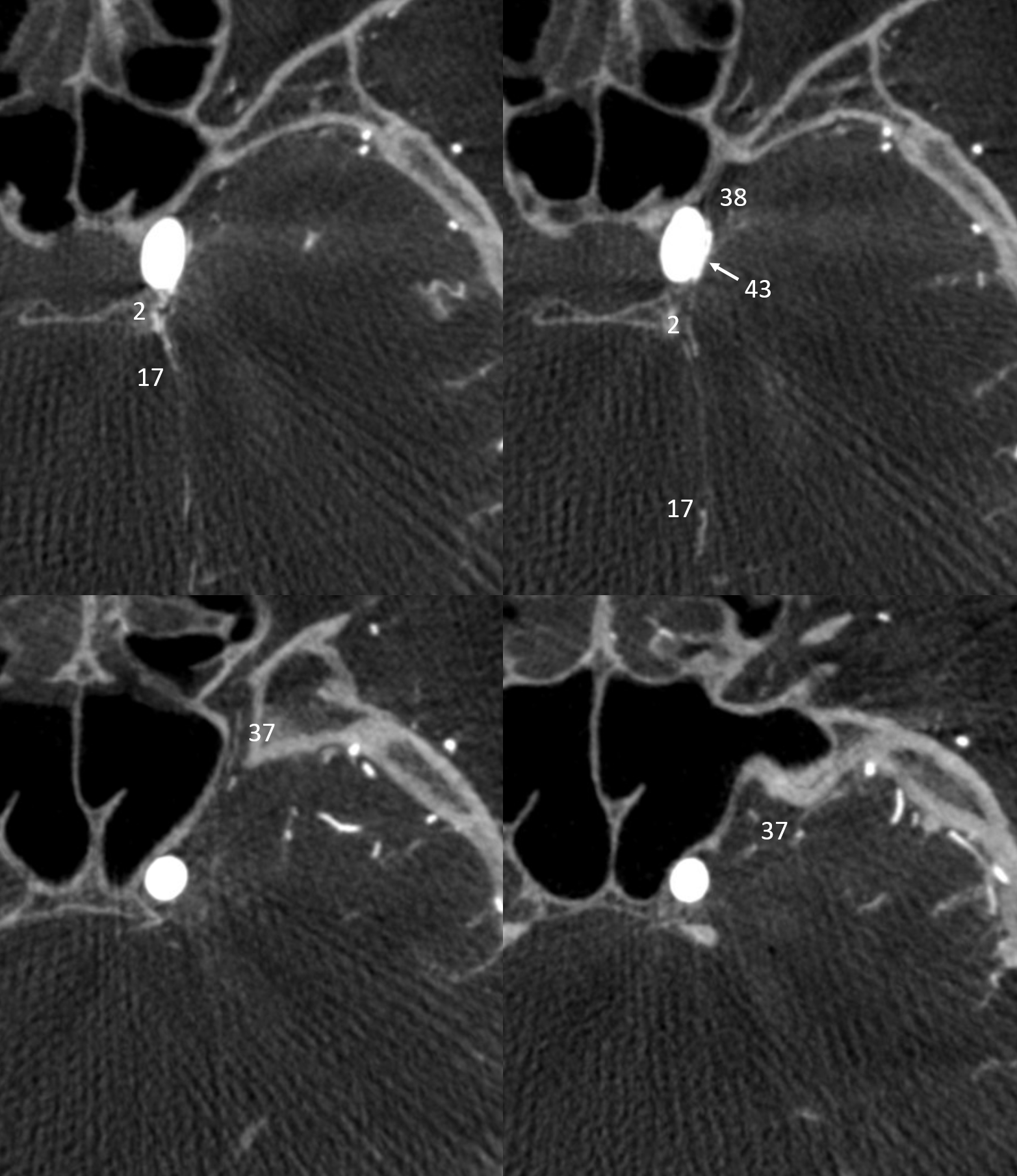
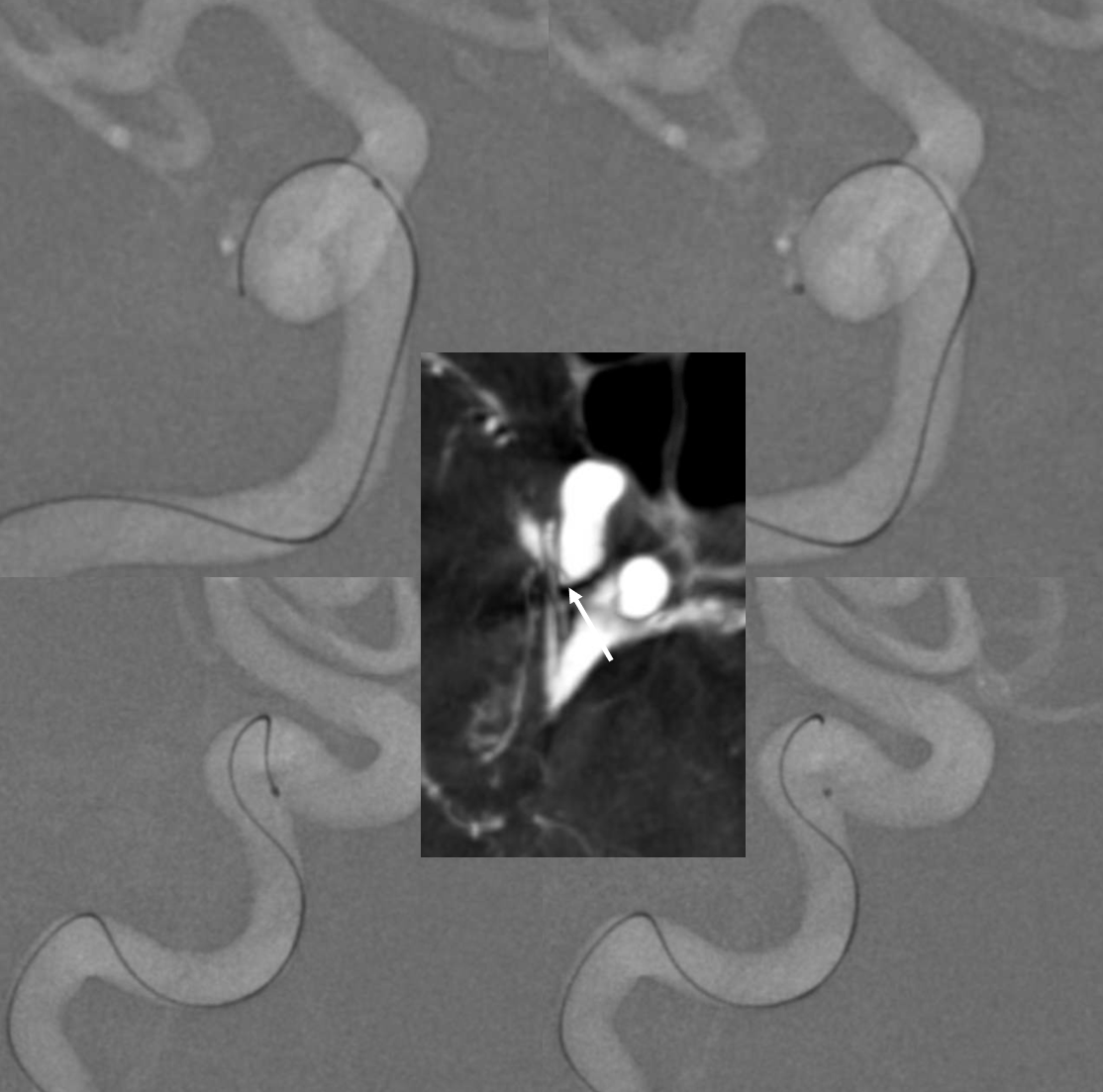
Very proximal origin of ILT (3), from very proximal horizontal segment. Typical origin MHT (2)
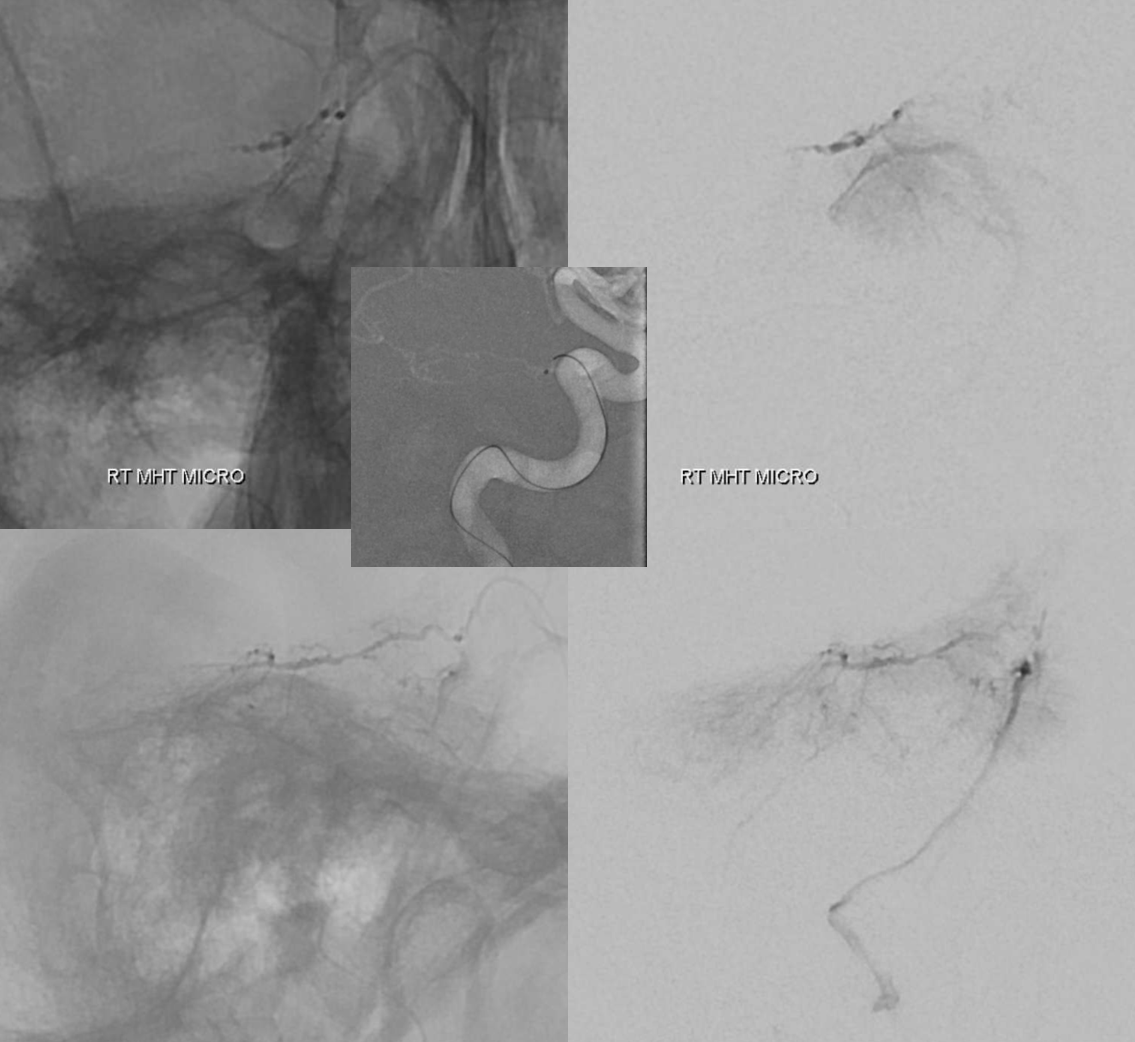
MHT catheterization and micro run — subsequent embo with 45-150 um Contour PVAs was done
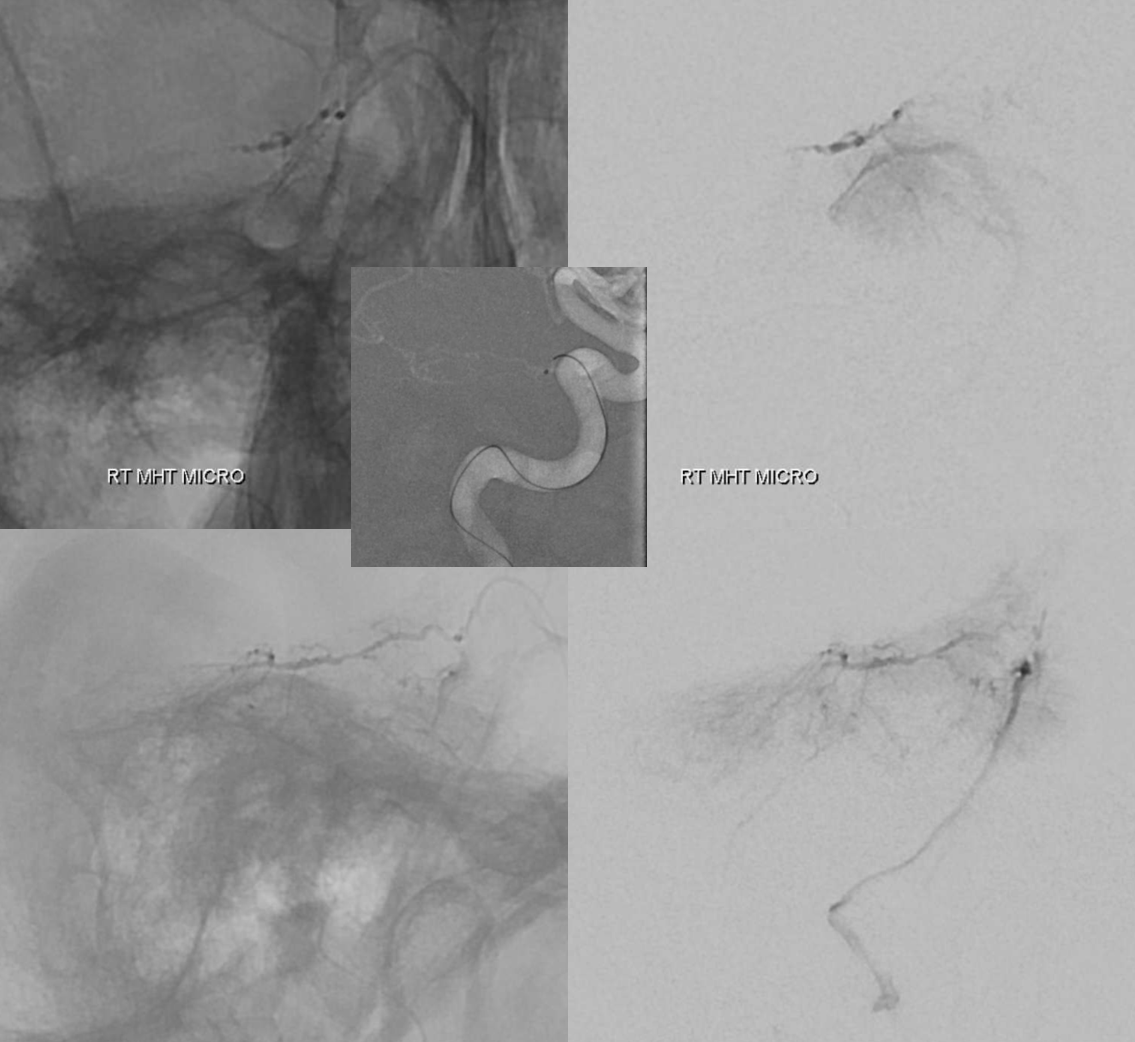
ILT catheterization — Headway Duo 167 cm and Synchro 2 soft — the winning combo for these — notice again proximal ILT origin, also seen in DYNA axial inset (arrow)
Micro run shows tumor supply along the lateral tentorial arcade. PVA embo same particles
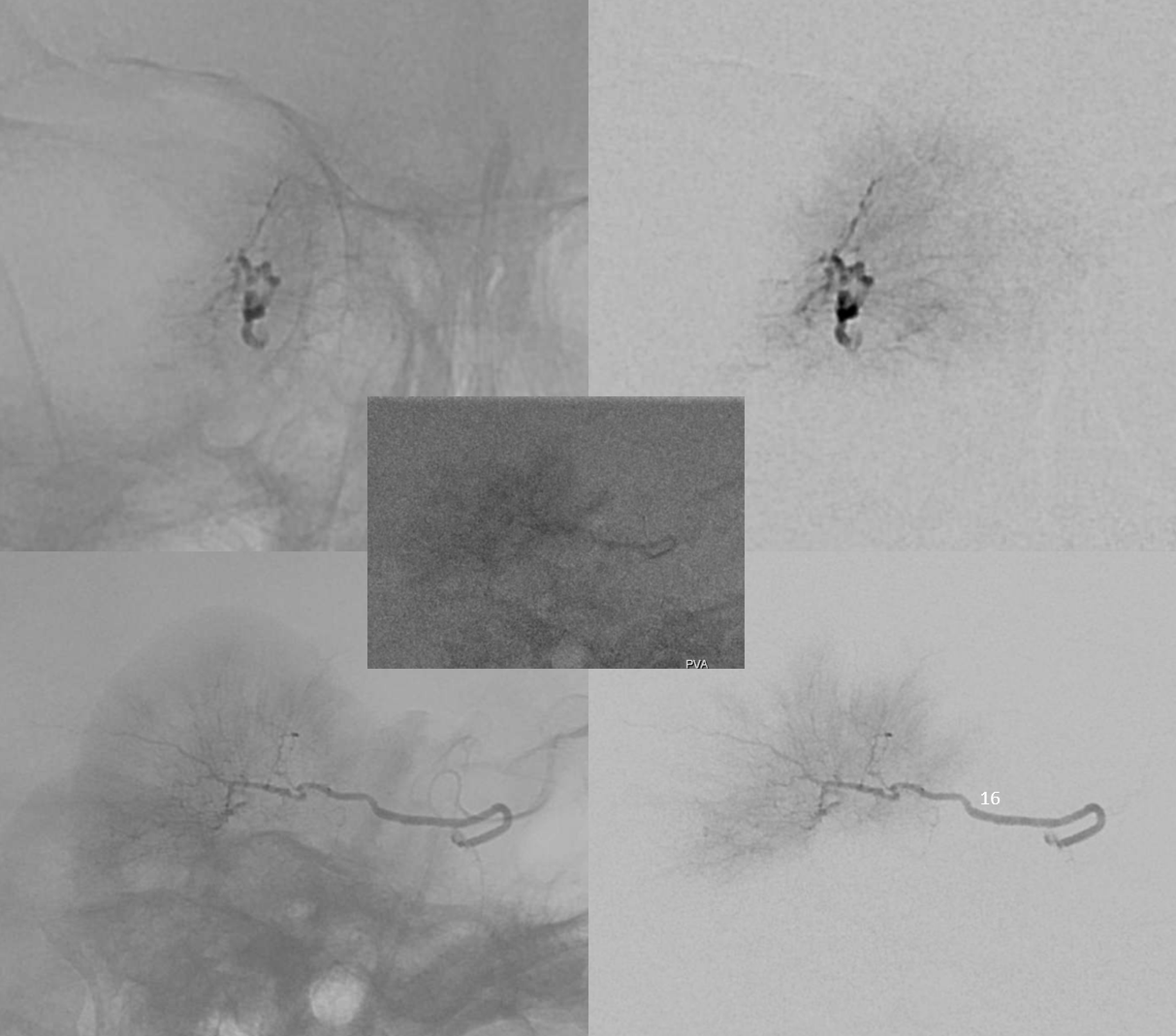
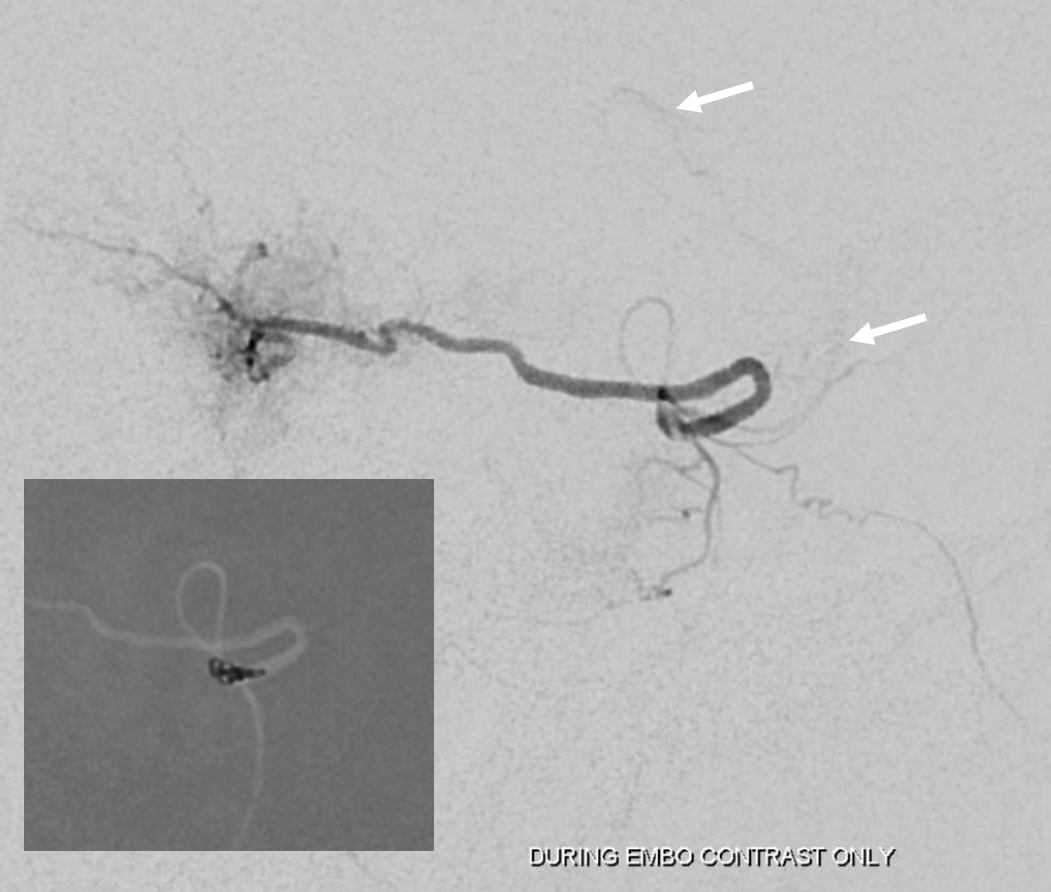
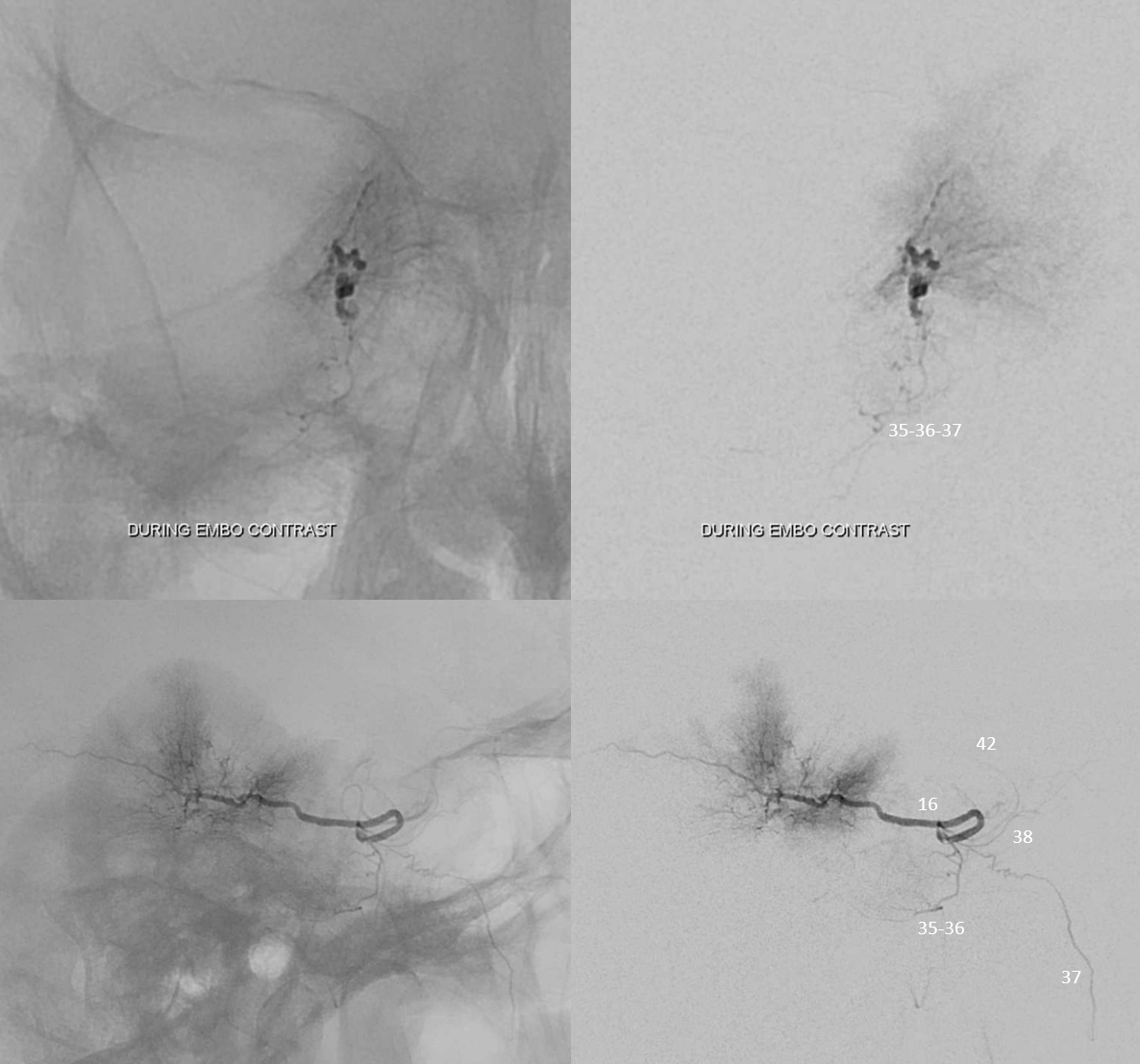
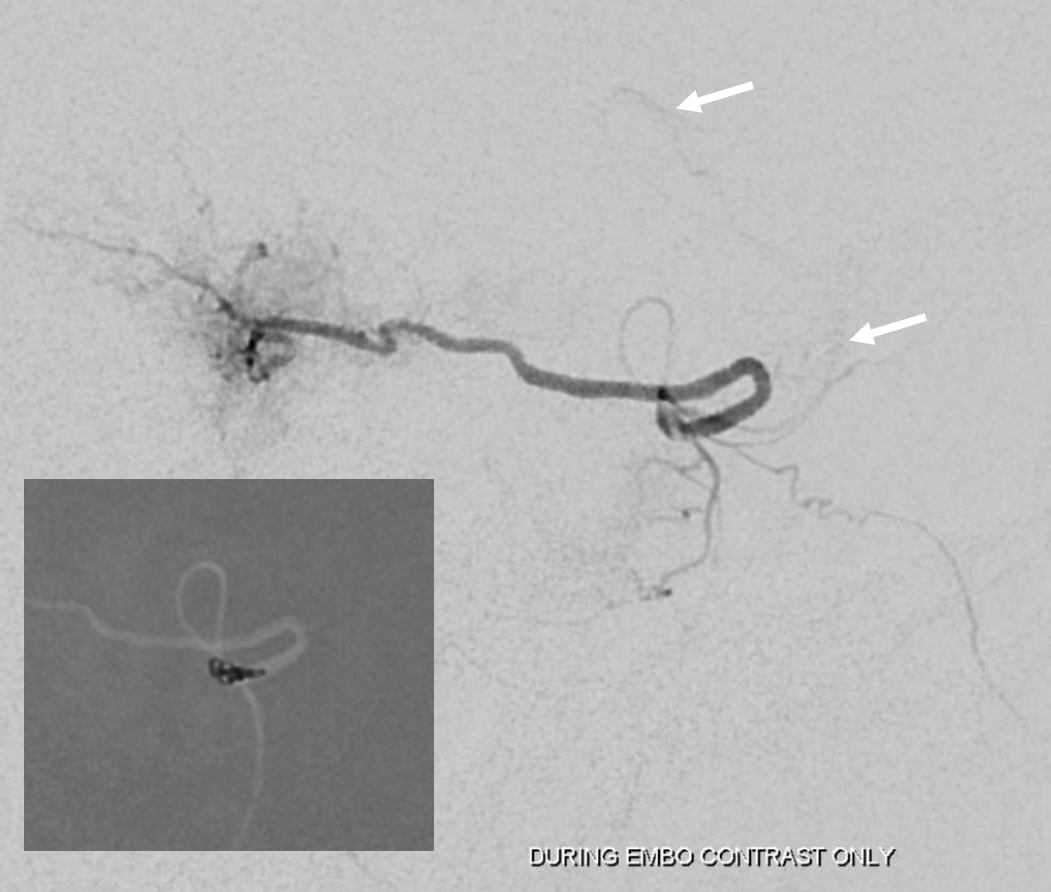
During embo, important to check — as tumor is filled with particles, hemodynamics result in increased reflux and contrast penetration of previously unpacified connections. The run below following partial embo shows all kinds of other ILT branches (proof that this is indeed ILT if you need one)
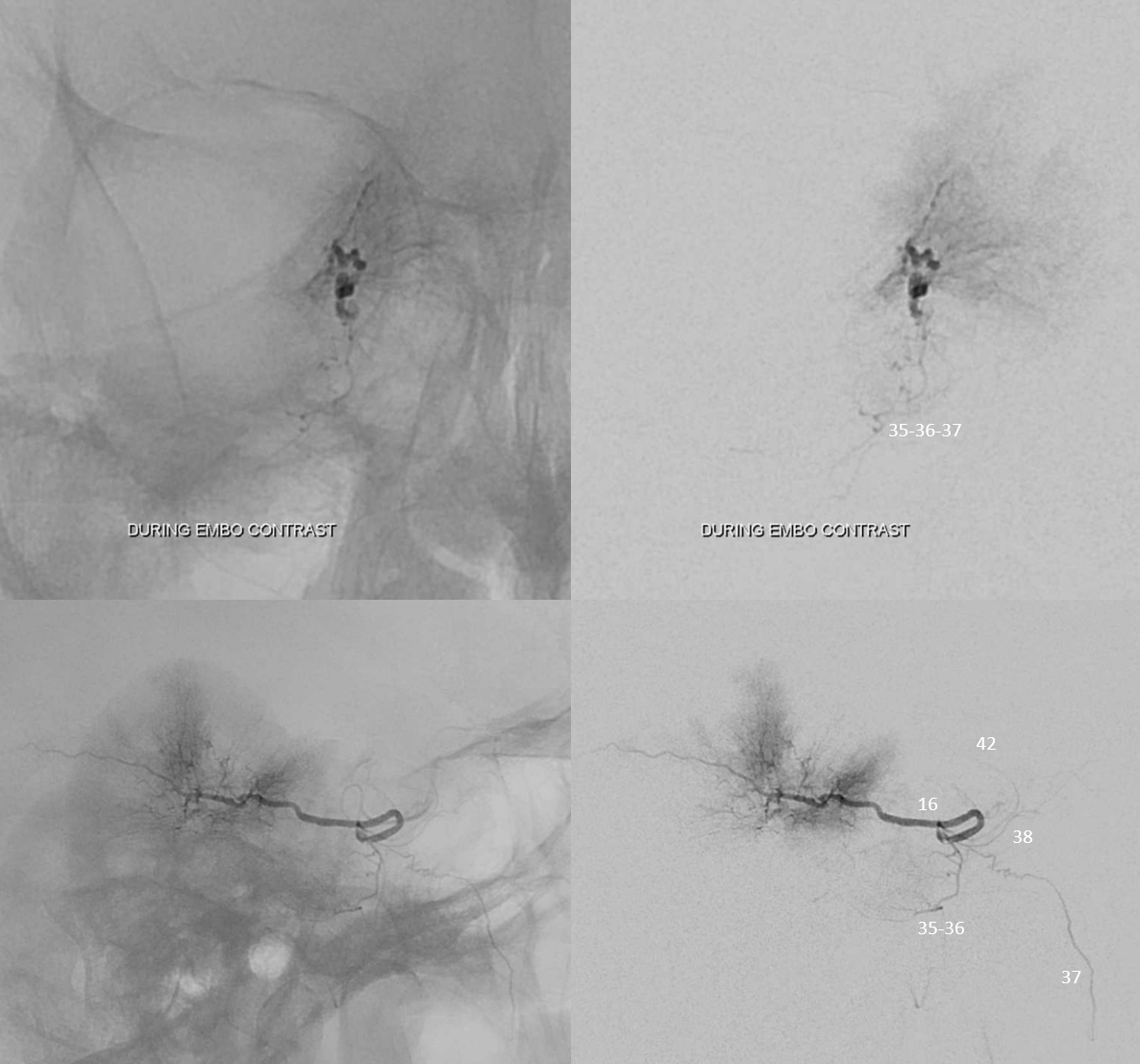
so, we put in more particles — very gently now. Another check later — these micro injections are done after carefully purging the microcatheter of particles, and injections are stronger than particle injections — to see what happens — shows same branches, but now also reflux into the ICA (arrows). At this point, we close the ILT with a small nano coil — nanos fit well into the long headway duo