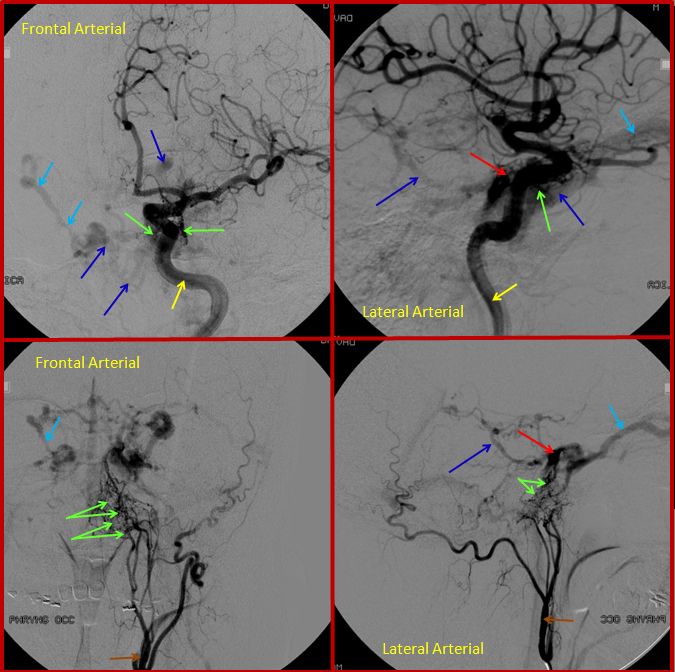
Case 1 — Vein-sparing (stent and transarterial embolization) approach
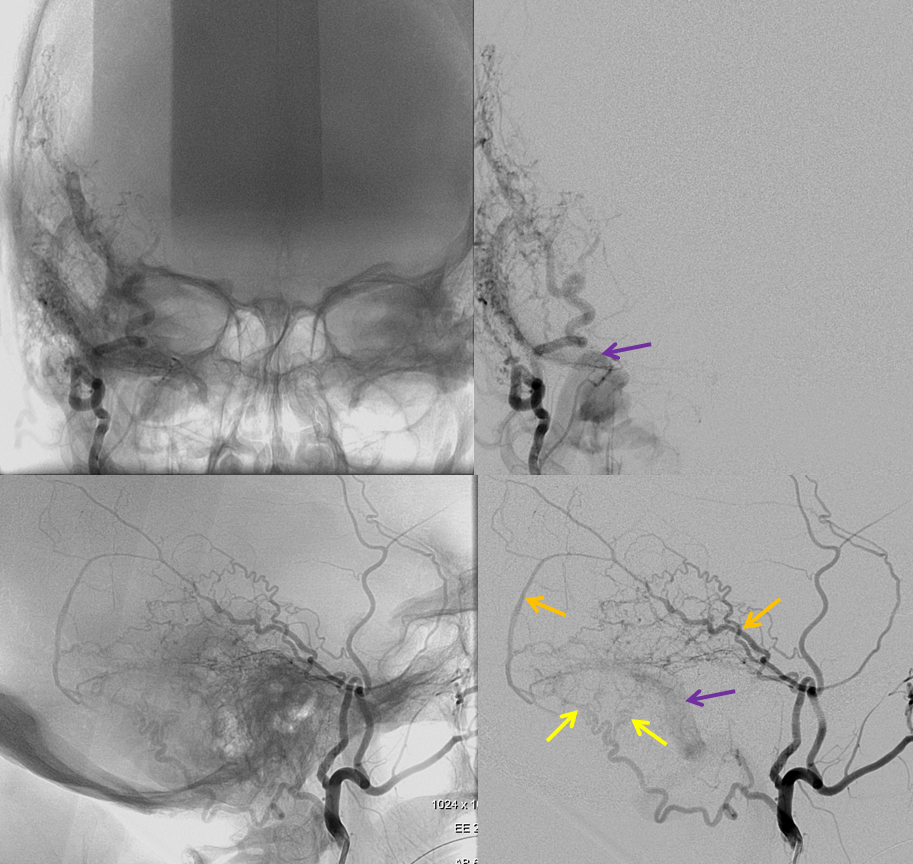
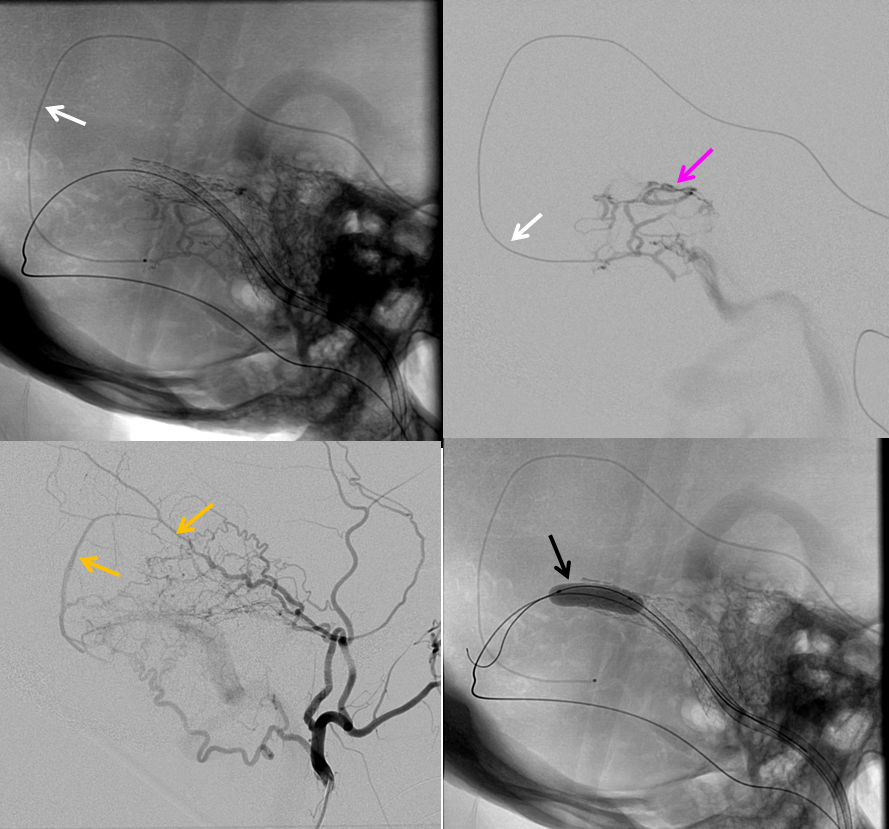
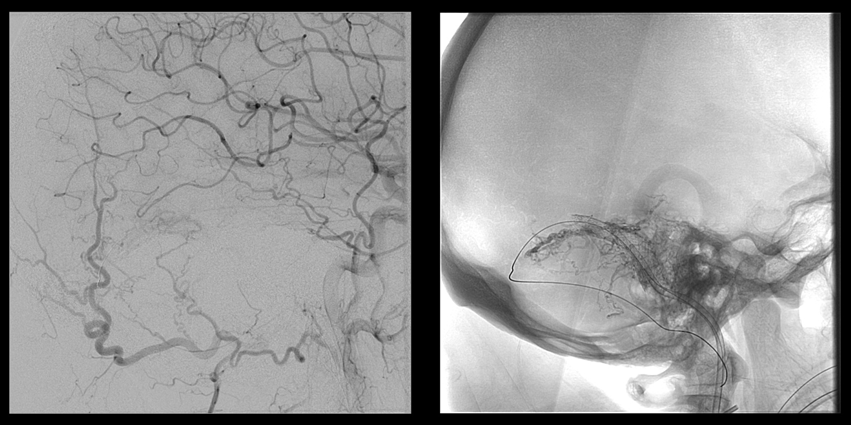
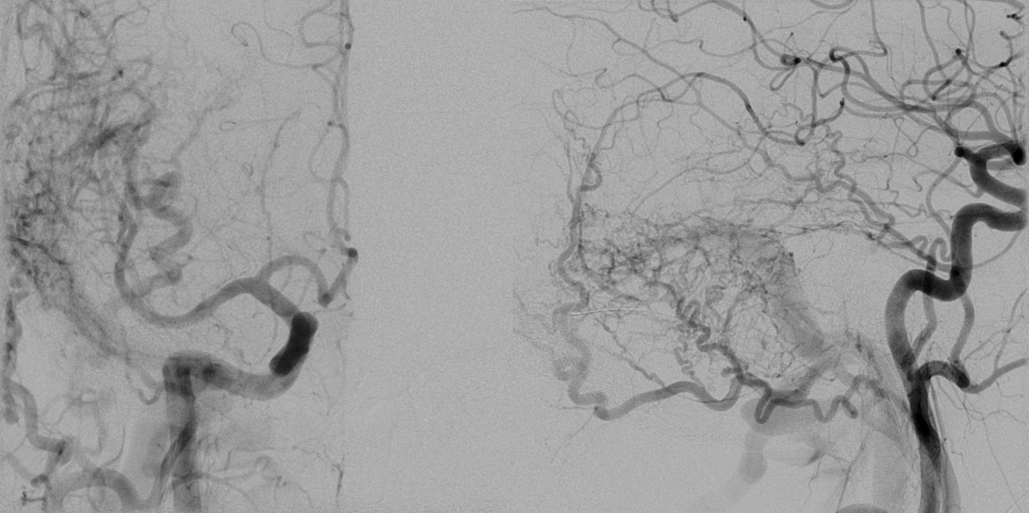
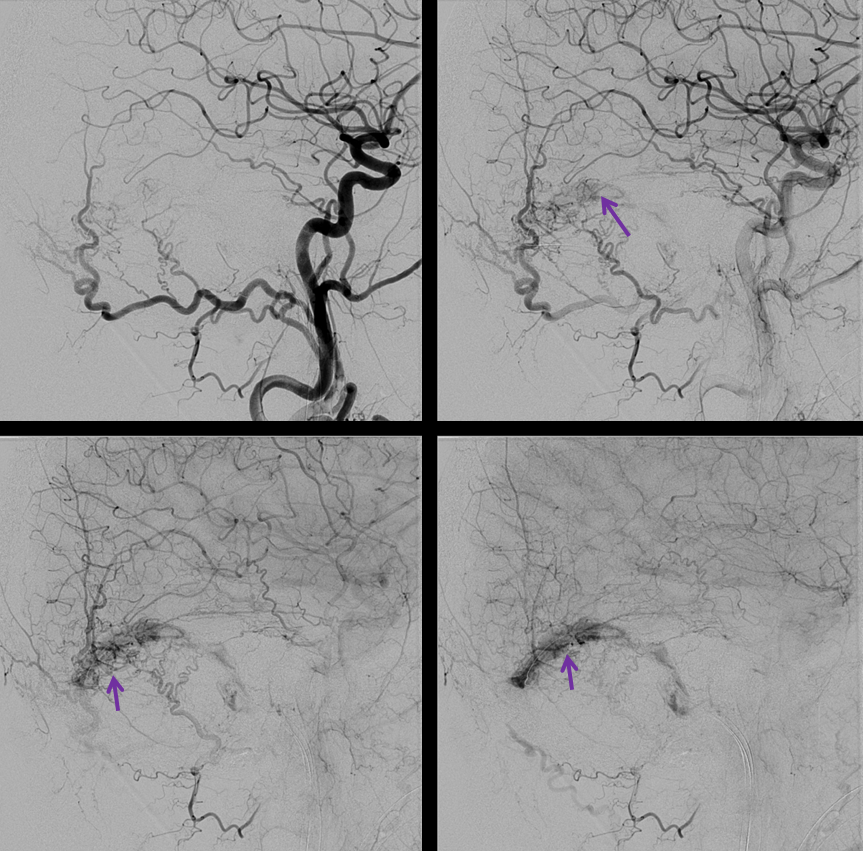
This woman in her 50s presented with right-sided pulsatile tinnitus, of several years duration. Right ECA injection shows premature opacification of the sigmoid sinus (purple); the fistula is supplied via branches of the middle meningeal artery (mostly petrosquamosal in dark yellow) and transmastoid occipital artery (bright yellow)
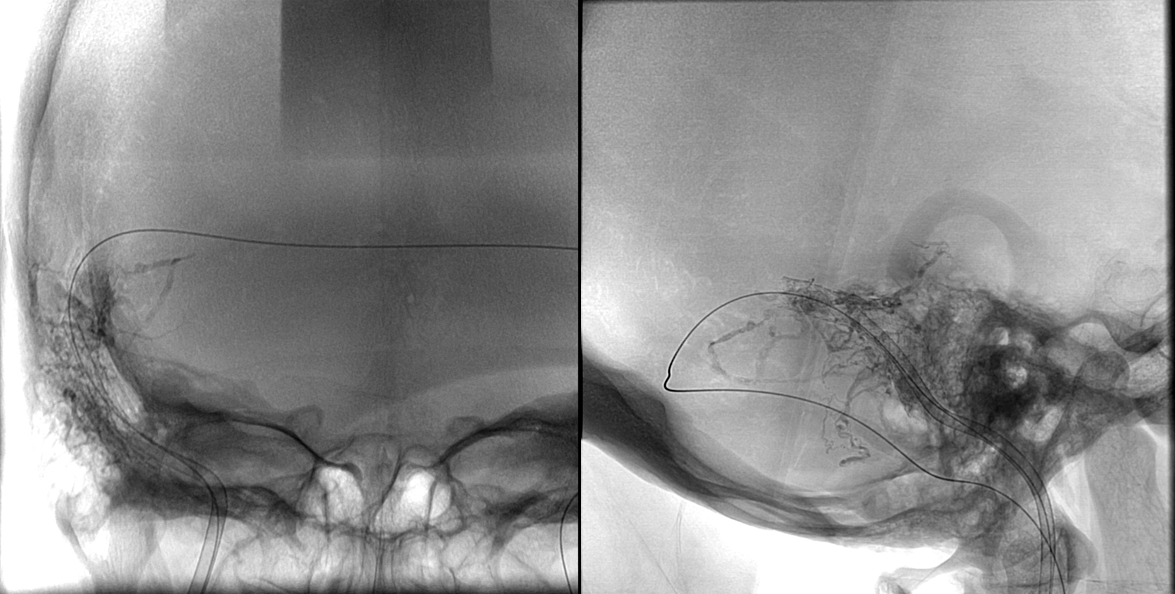
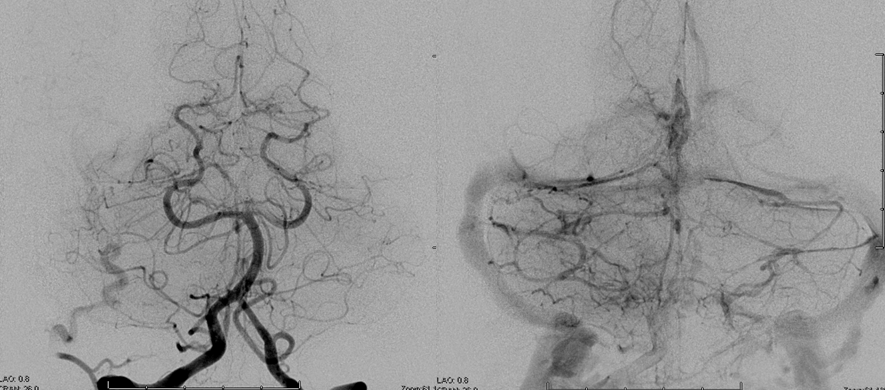
Movies of the same injection, in AP and lateral projections
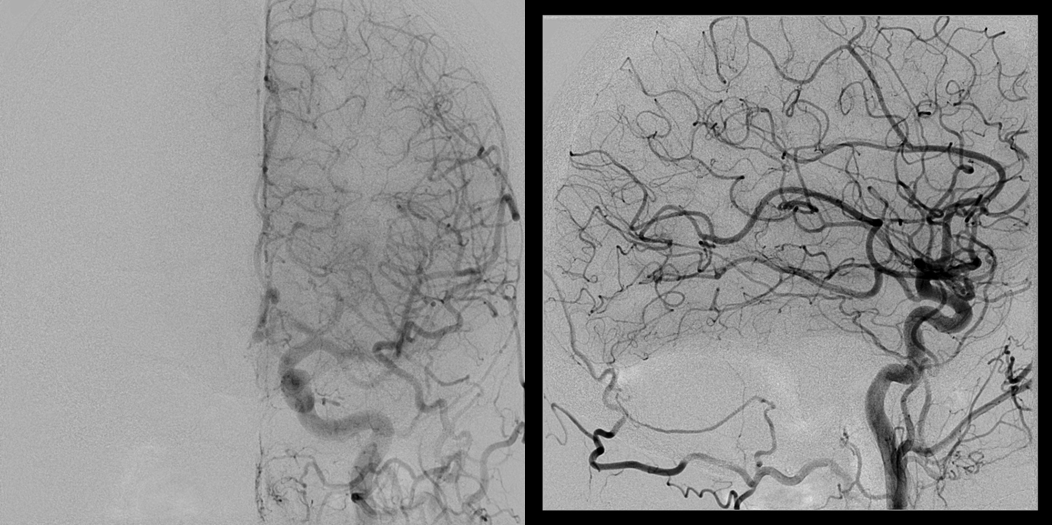
Contralateral left ECA injection, demonstrating innumerable torcular dural arteries (brown), supplied by transmastoid branch (white) of the occipital artery (green), feeding into the fistula via a common arterial channel (pink) within the medial wall of the transverse/sigmoid sinus — this artery can also be supplied via the jugular division of the ascending pharyngeal artery. The fistula itself (red arrow) is better seen from this injection, without overlying branches of the right ECA injection.
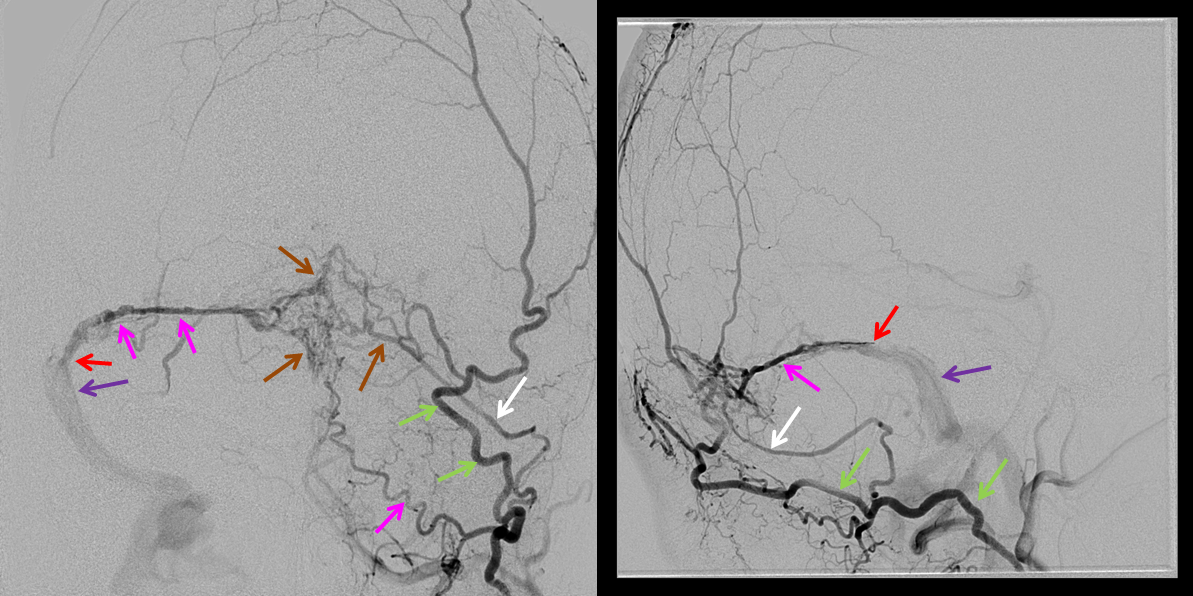
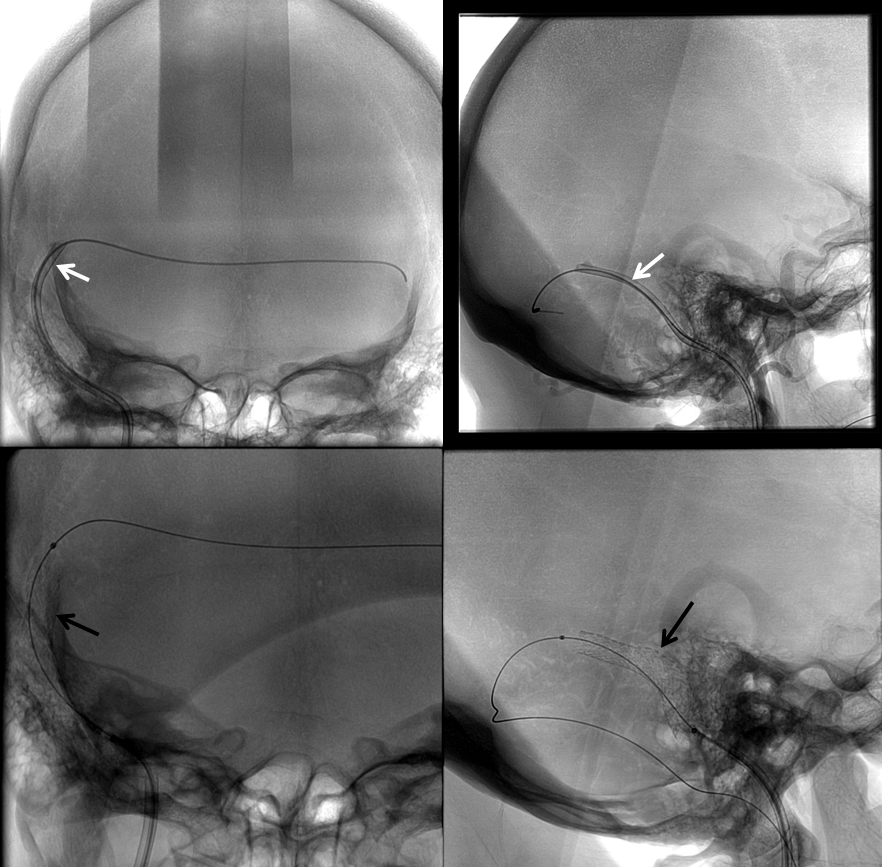
Venous access is obtained, and a large enough distal access catheter (white) placed into the transverse sinus to facilitate delivery of a stent (Precise carotid stent, in this instance, black)
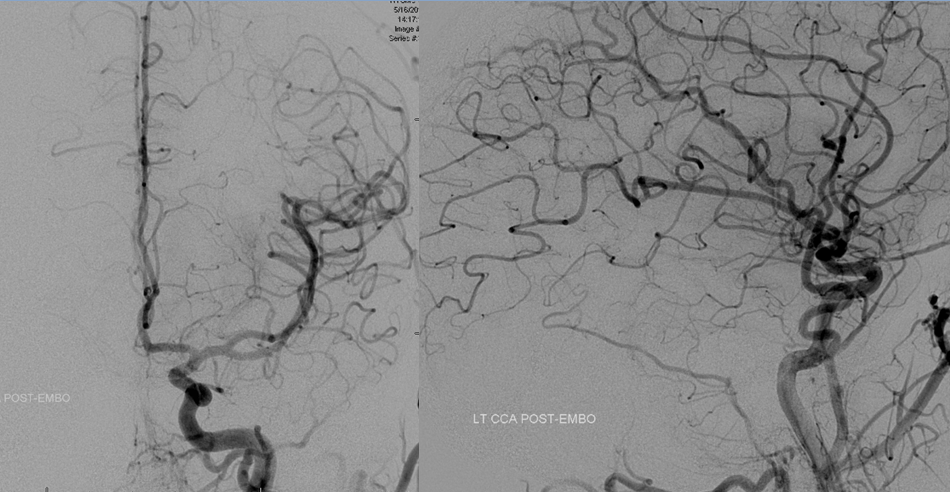
Post-stenting right common carotid artery injections
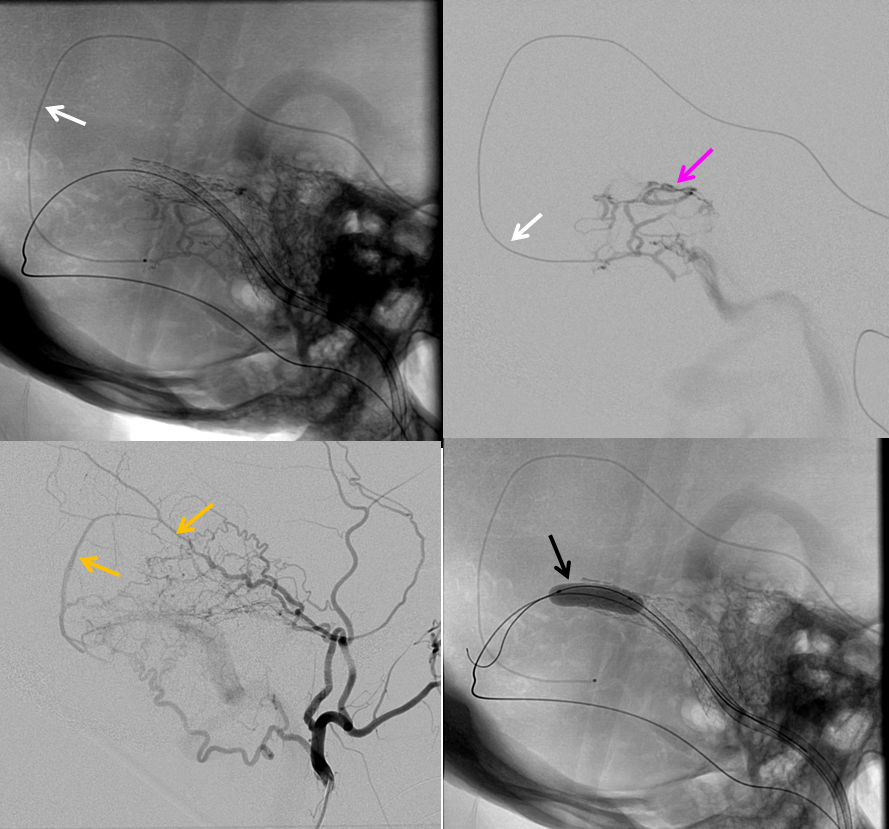
A microcatheter (SL-10, white) is now placed into the distal right petrosquamosal branch (dark yellow) of the middle meningeal artery. Because the middle meningeal branches are straigher and better supported by adjacent dural and skull, a substantially more distal catheterization, hense closer to the fistula, is possible as compared with the tortuous occipital artery, which meanders within relatively unsupportive soft tissues. A microinjection visualizes multiple arterial feeds to a part of the fistulous arterial channel (pink), and portions of the sigmoid sinus are visible. Finally, a compliant balloon (Hyperglide) has been inflated in the transverse sinus and distal stent to further protect the sinus from glue clumping.
Movie of the glue shot is shown below. At the start of the movie, there is already glue present in the vasculature, so not all glue deposition is recorded. The catheter is pulled back in the middle of the movie, and glue permeates another channel, coming in contact with the balloon. This causes the balloon to rupture (these balloons always pop on glue contact) and deflate, appearing as a negative white image on a live subtraction image. The catheter is then pulled.
Post-glue static images, demonstrating the glue cast in relation to the stent. Most of the glue is located medial to the stent.
Right CCA injection, demonstrating decreased flow through the fistula. Part of the fistula remains open (purple arrow pointing to sigmoid sinus). Notice that flow is now mostly retrograde in the sinus, because some glue inivariably gets into the vein around the stent.
The petro-squamosal branch is re-catheterized to address residual fistula. Notice a common arterial channel (pink) proximal to the sinus.
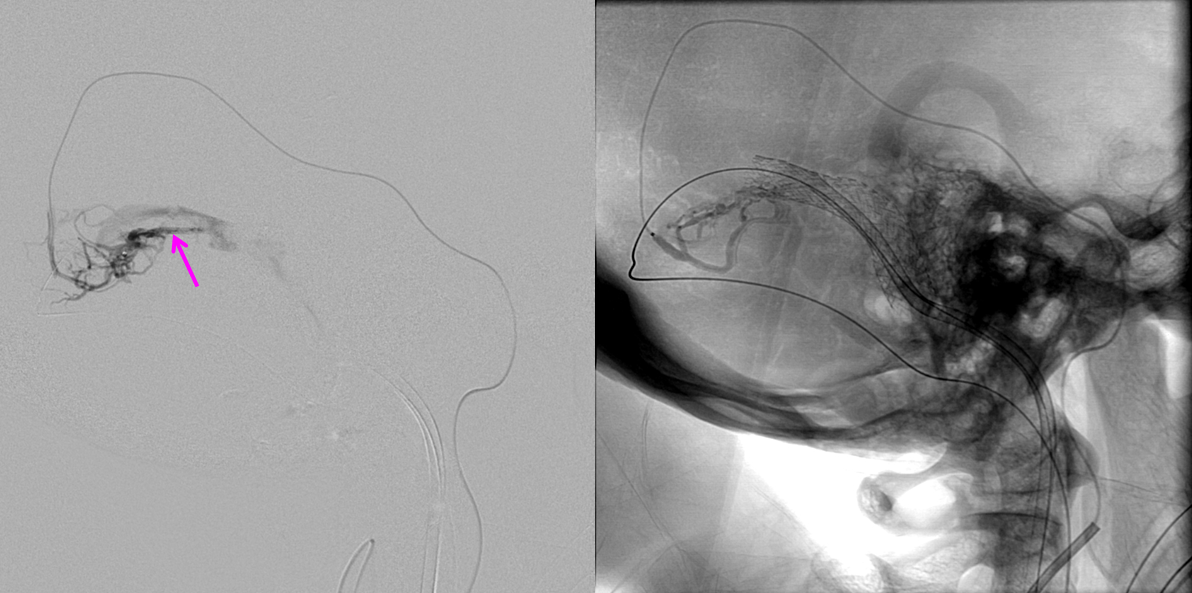
A second n-BCA injection is performed.
Post-embolization lateral projection views showing closure of the fistula. The glue cast is seen on native image
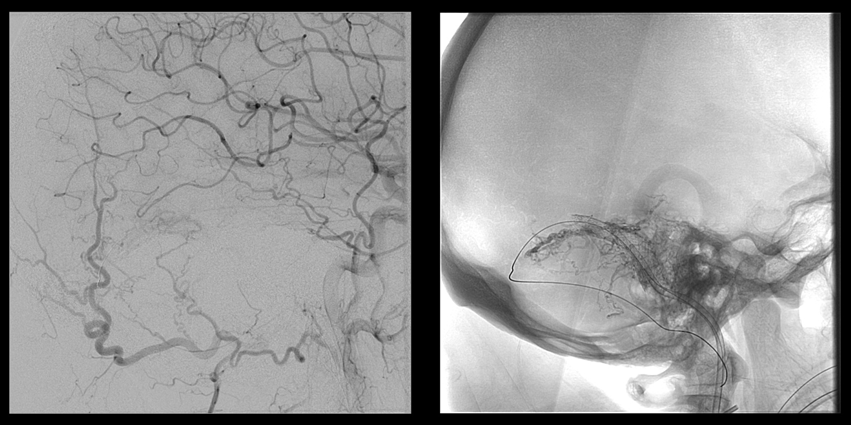
A second precise stent was placed into the sigmoid sinus proximal to the fistula, to squeese intra-sinus glue against sinus walls and faciliate antegrade fllow (stent deployment shown) Post-stenting control angiogrpahy from left CCA shows no reconstitution of the fistula through the torcular branches. The flow in the right sigmoid sinus is now freely antegrade.
Control injection of the left vert, also demonstrating no more fistula. All potential sources of re-supply must be checked before fistula is considered closed.
The patient remains asymptomatic.
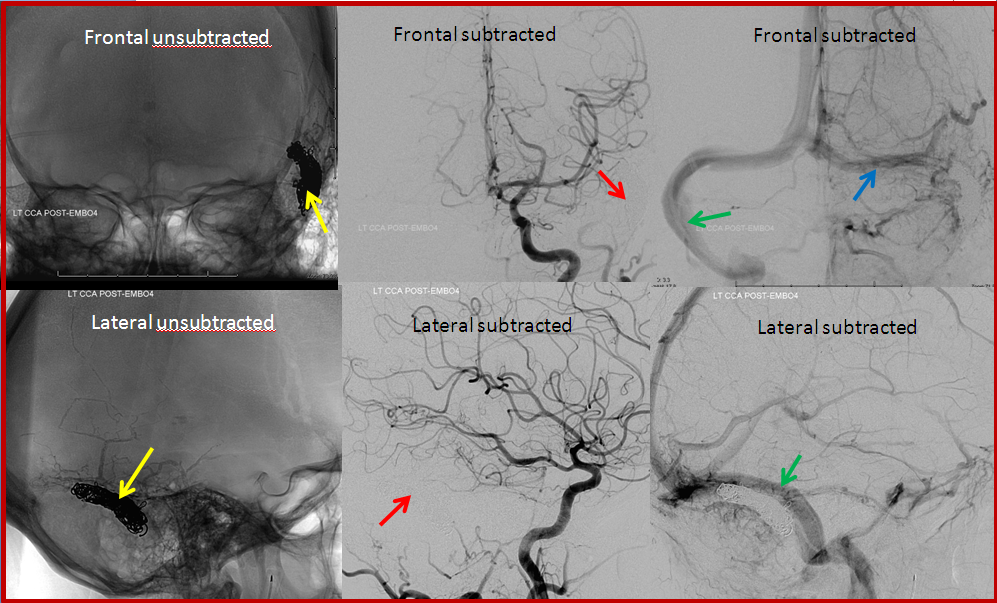
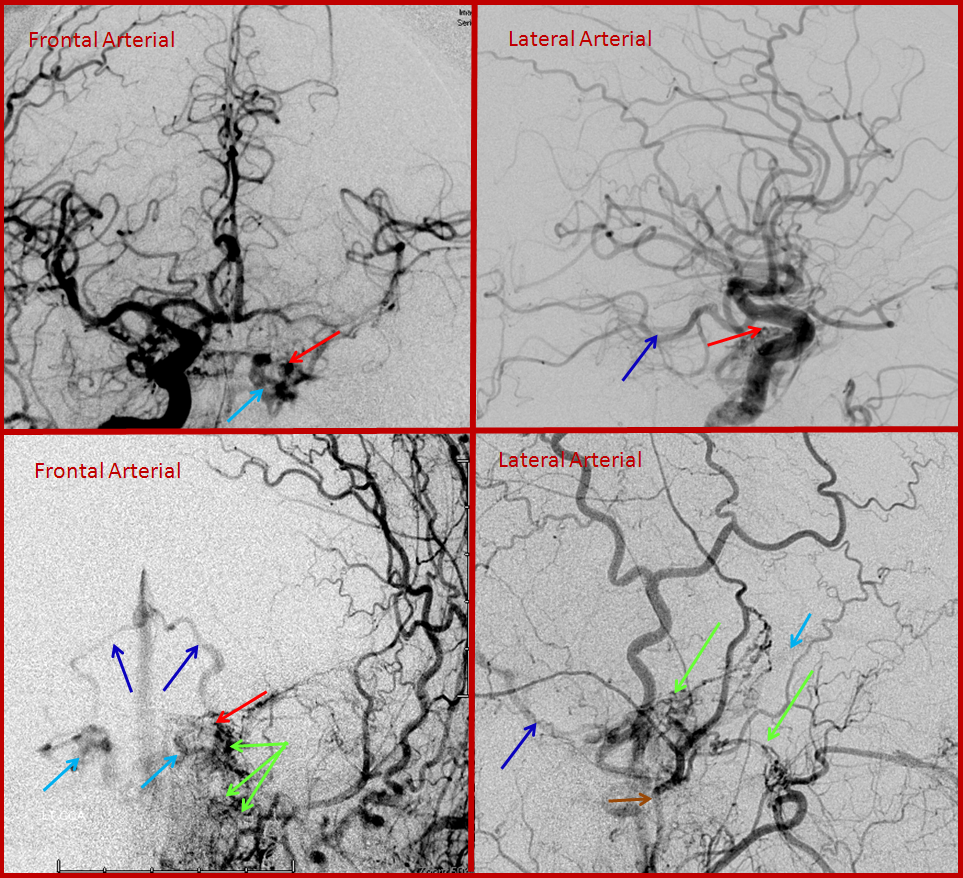
CASE 2 — venous sinus coiling
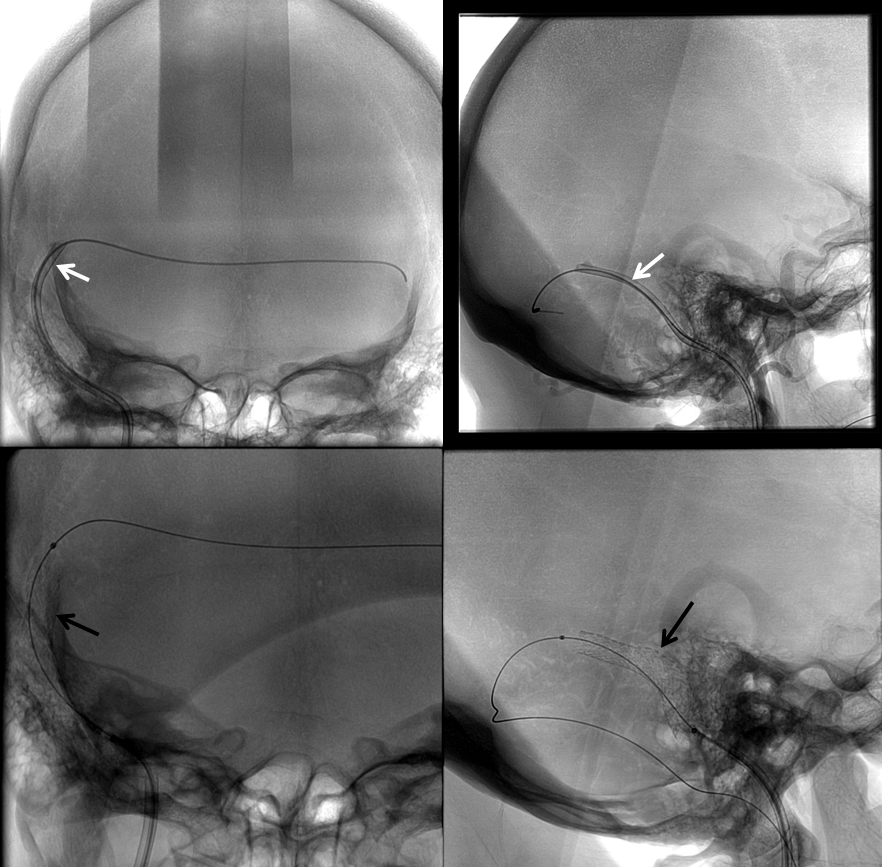
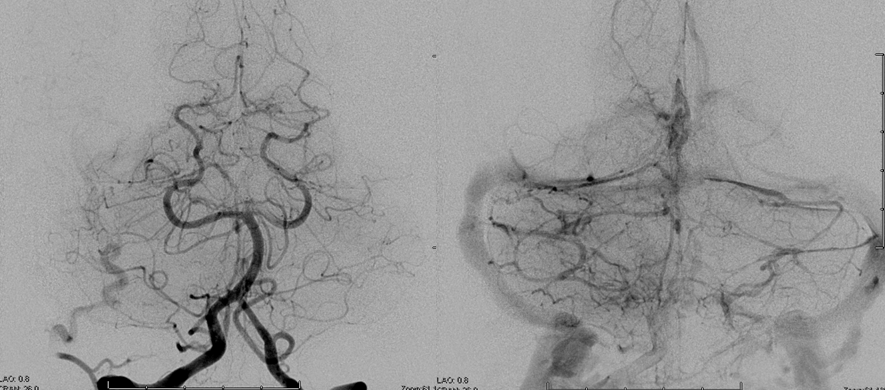
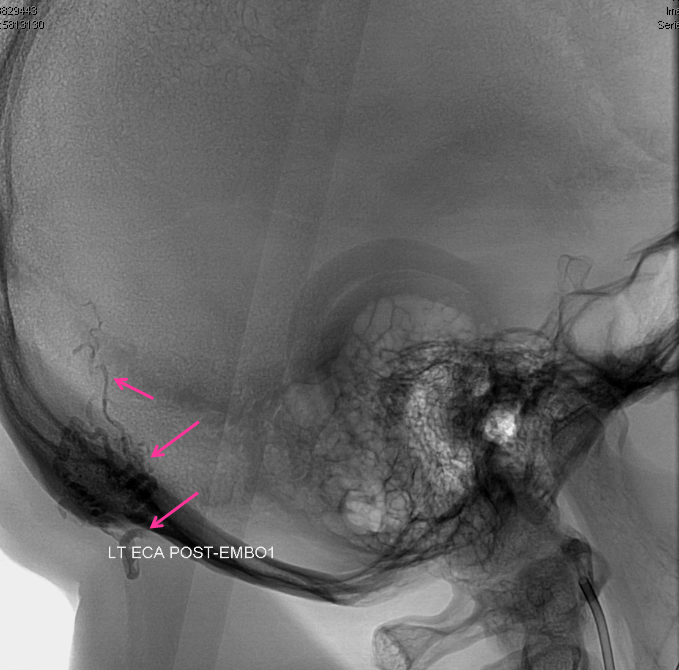
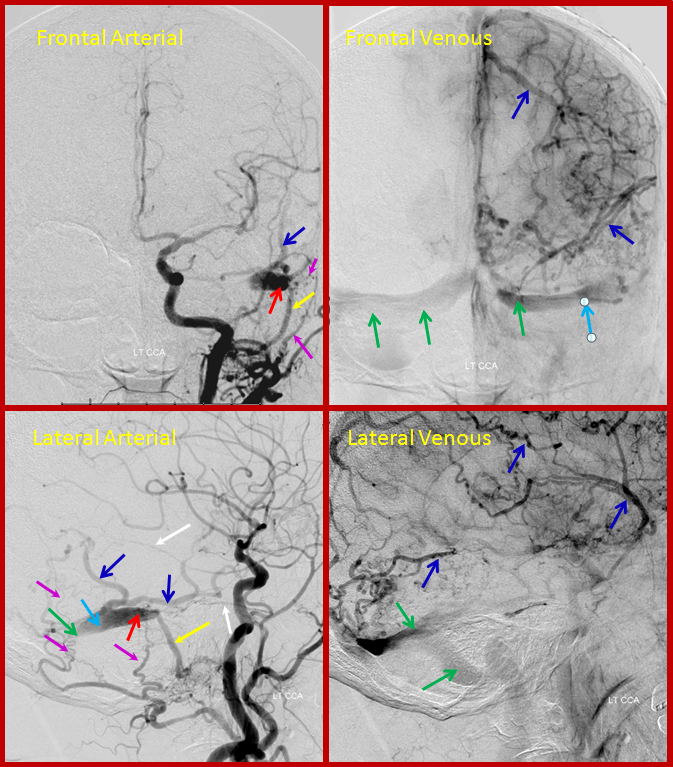
Typical sigmoid sinus fistula. This patient also presented with pulsatile tinnitus.
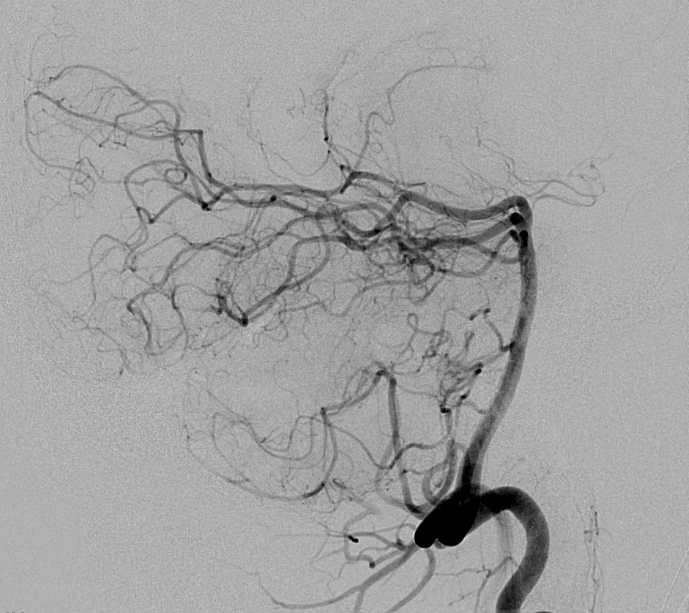
Left external carotid injection, showing innumerable occipital feeders, and several middle meningeal ones. This might be construed as a multiple hole fistula, but it is not. The single fistula point is marked by red arrow, onto which middle meningeal branches converge.
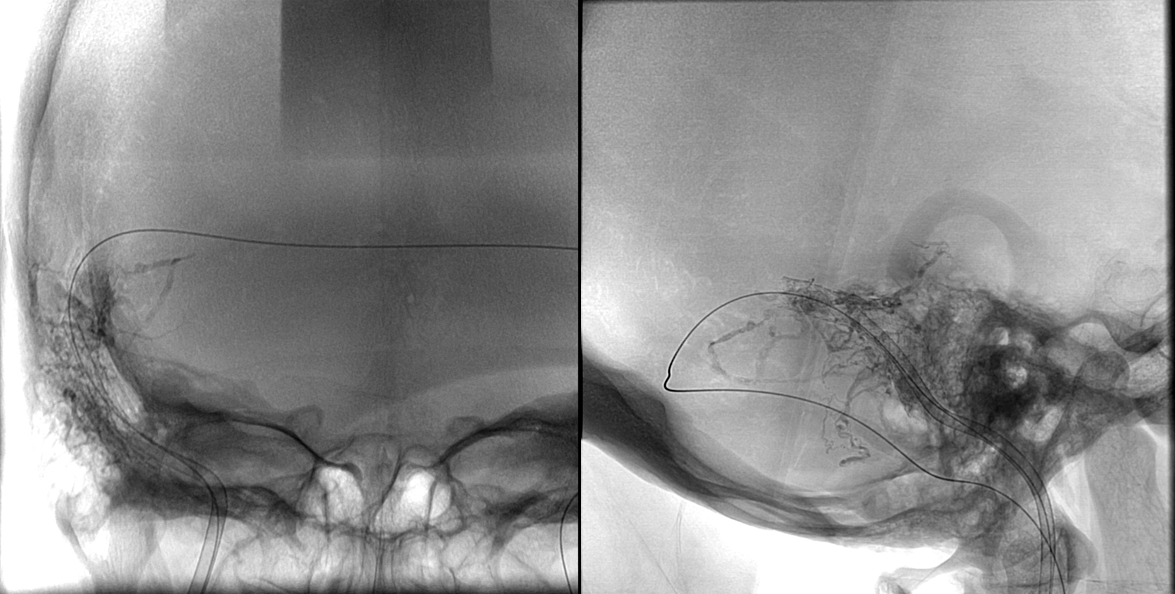
Transvenous coil embolization of the sigmoid sinus. Notice that coil mass is tightest near the fistula, which is completely occluded. A posterior temporal vein drains into the left transverse sinus and retrograde to the right.
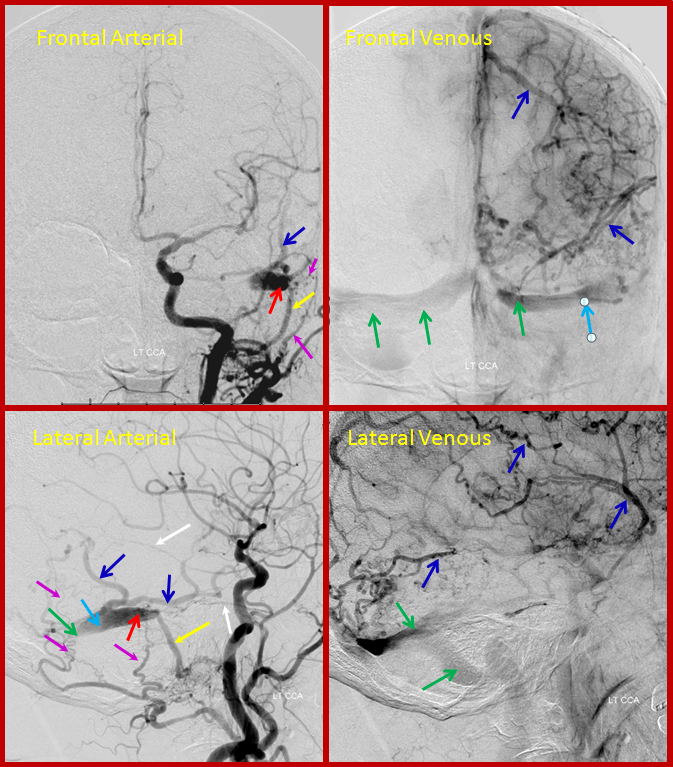
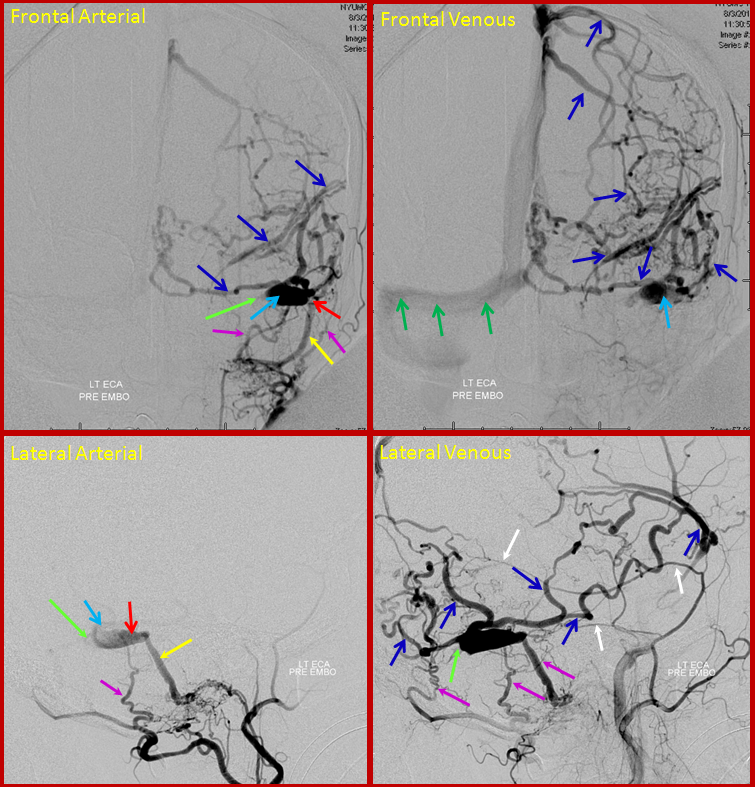
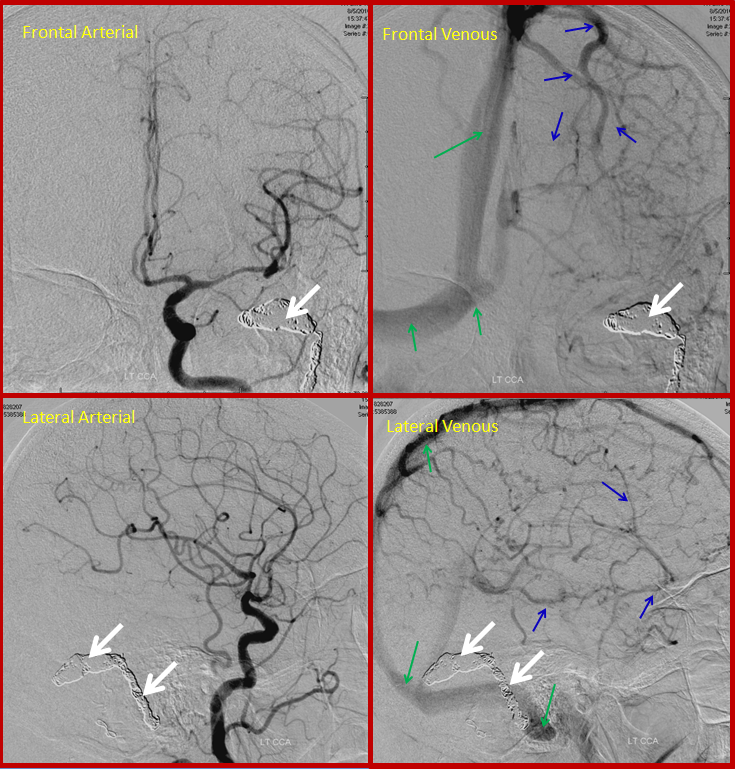
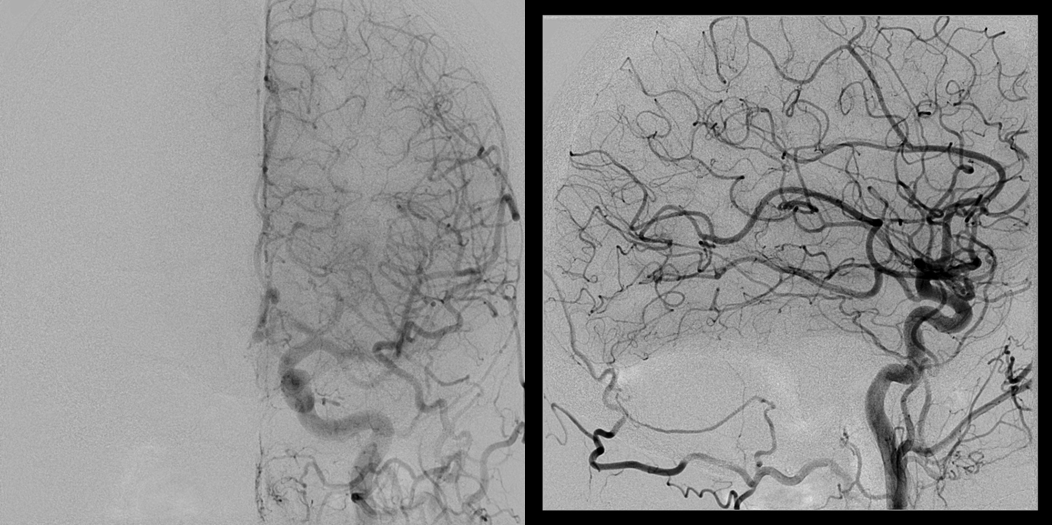
CASE 3 – advanced sigmoid sinus fistula.
This patient presented with headaches and pulsatile tinnitus, having no other symptoms.
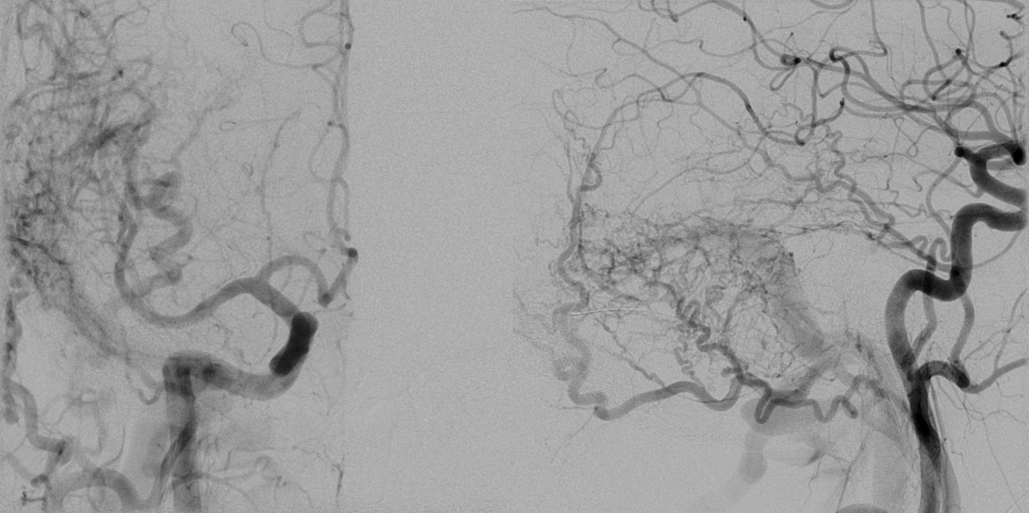
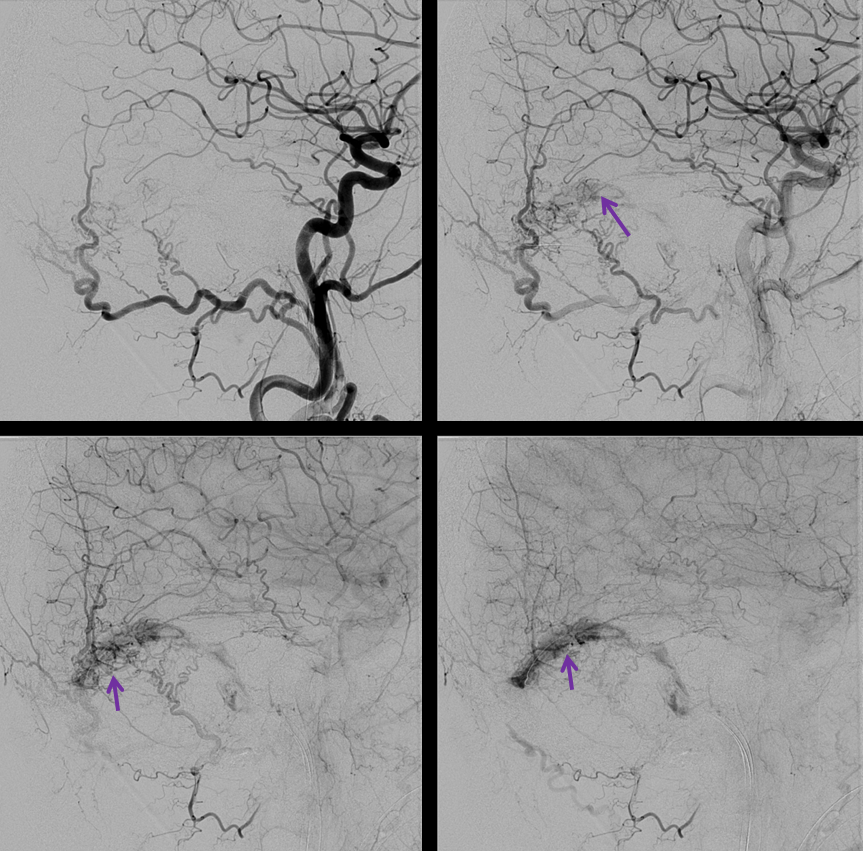
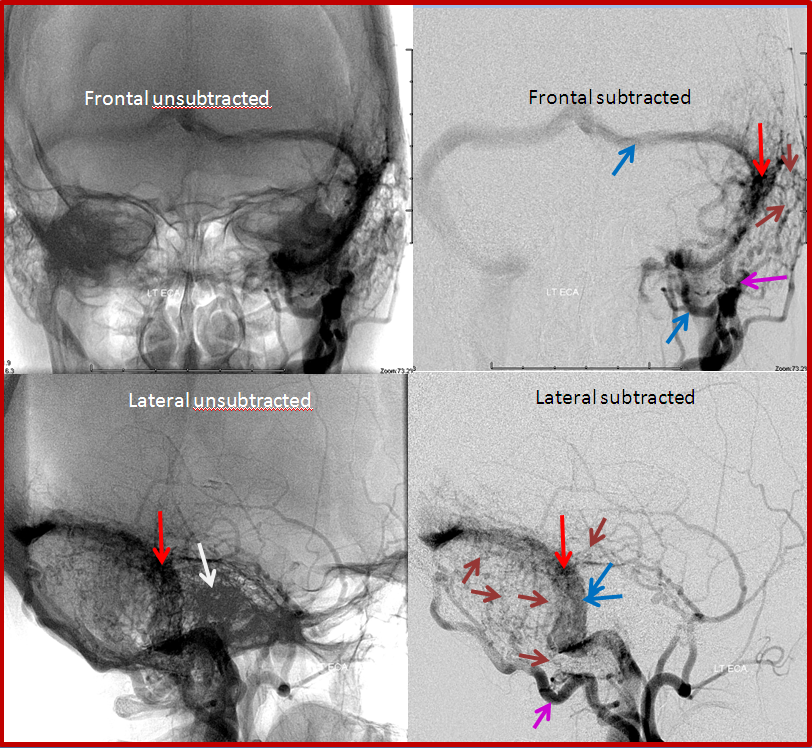
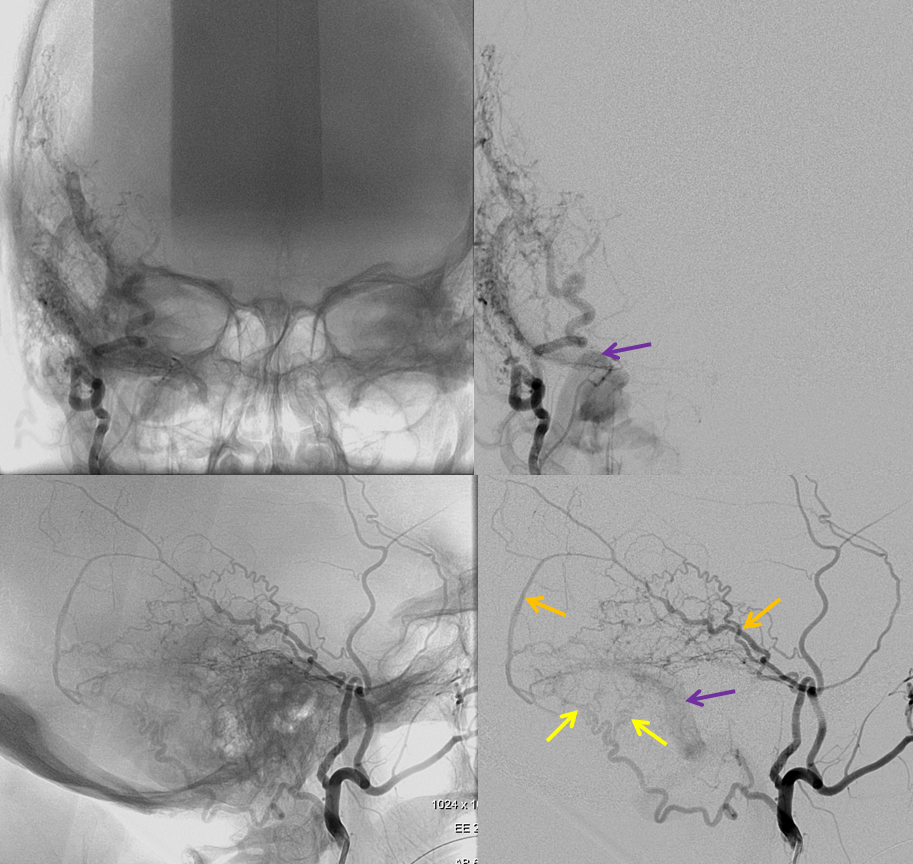
Arterial and venous images of left common carotid injection during diagnostic angiography show sigmoid sinus (light blue) single hole fistula (red) supplied by occipital and middle meningeal artery branches (pink), draining retrogradely into the transverse sinus (green). The ipsilateral jugular outflow is occluded. Extensive retrograde drainage into cortical veins is present (blue).
The patient returned for treatment 2 weeks later, and reported that her tinnitus has disappeared. The pre-treatment angiogram, below, showed that the left transverse sinus proximal to the fistula has occluded (bright green arrow points to new occlusion), such that the fistula (red) empties into a short segment of the transverse sinus, and having now nowhere else to go, drains exclusively into cerebral cortical veins (blue arrows), which then in retrograde fashion opacify the torcula and right transverse sinus (dark green). We typically caution our pre-embo patients to contact us should their tinnitus improve, for this very reason.
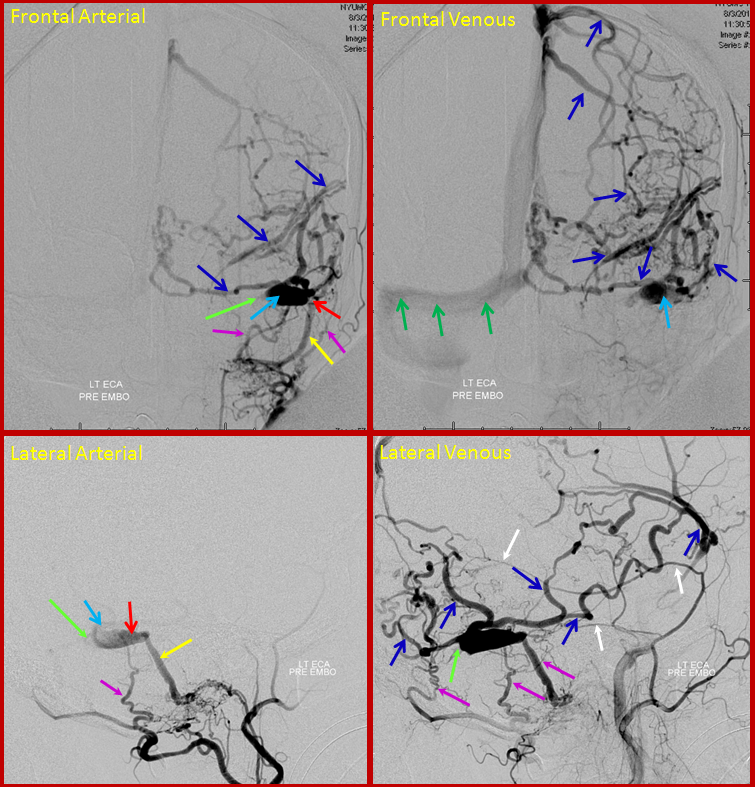
Below is a post-treatment picture. A wire was successfully passed from the right jugular, accross the torcula, and through the freshly occluded left transverse sinus into the sinus segment receiving the fistula. The sinus was then coiled (white arrows), closing the fistula. The brain veins (dark blue) are now once again being used by the brain, draining into the superior sagittal sinus (dark green arrows)
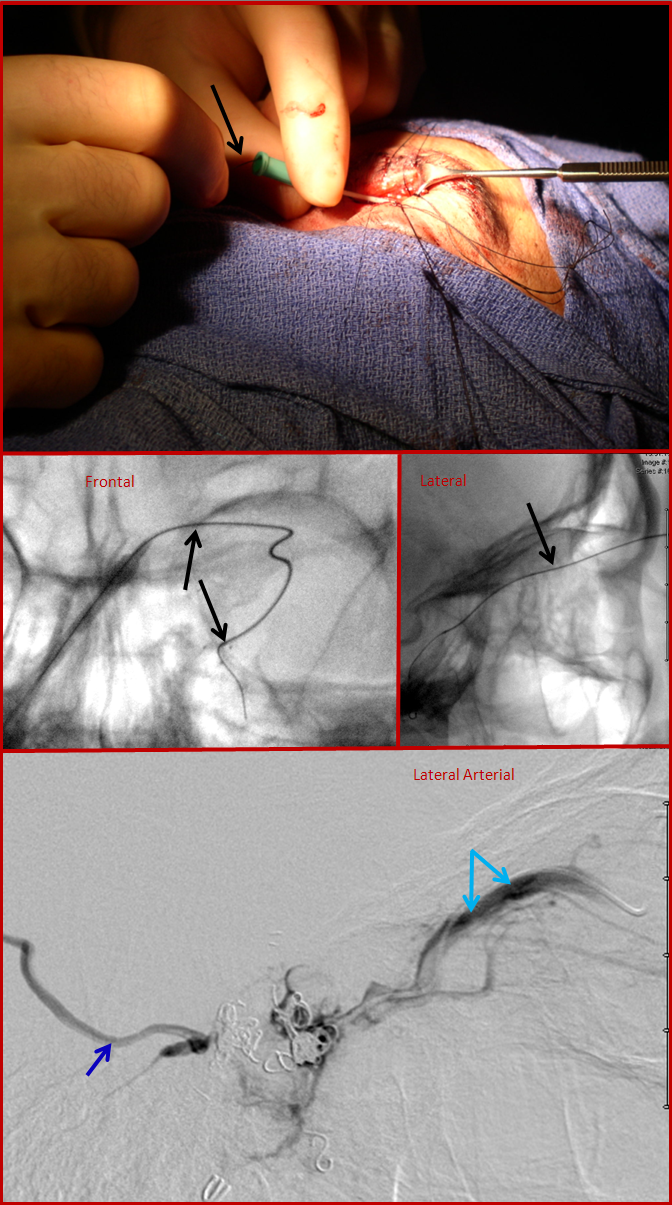
CASE 4
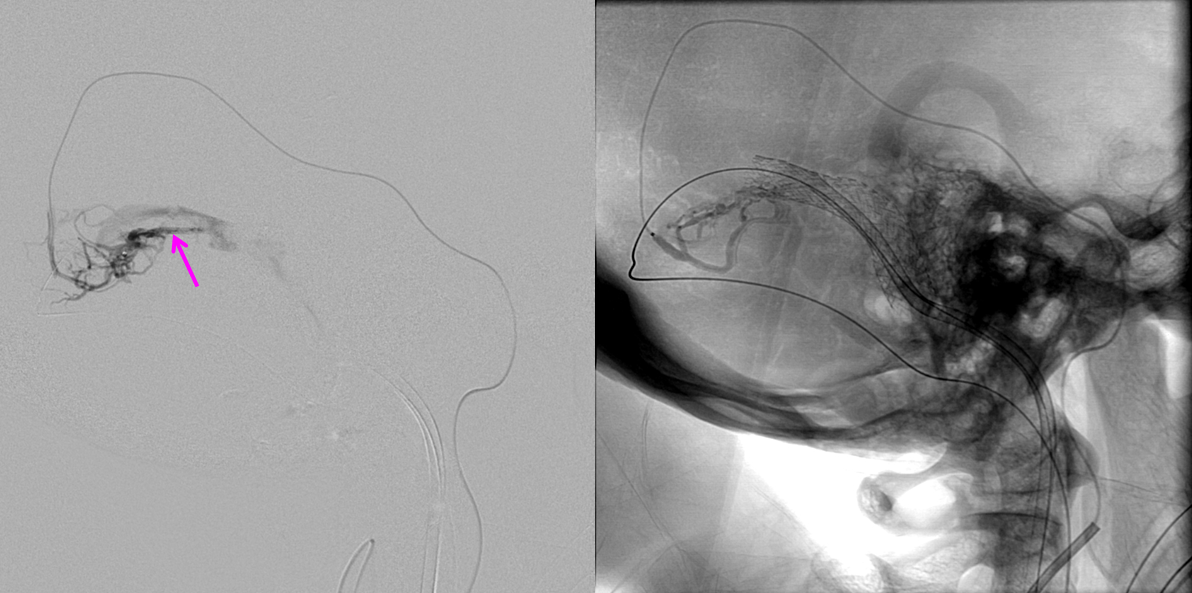
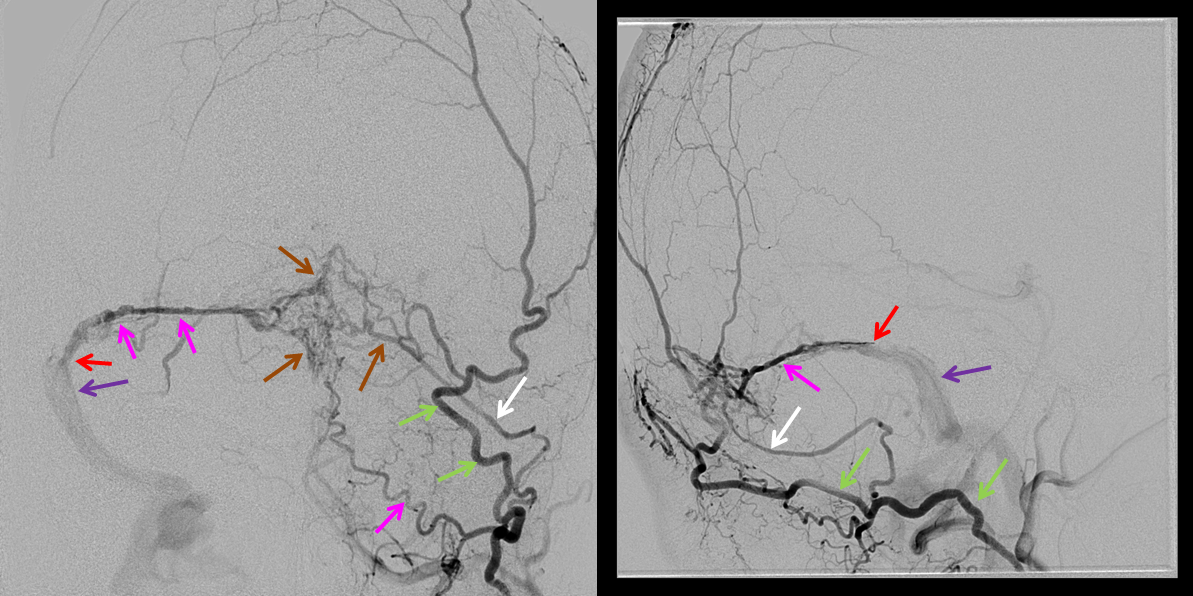
This patient came to the emergency department with bulging, red, swollen left eye, and was subsequently found to harbor a high flow cavernous sinus dural fistula. The fistula (approximately located where red arrow points to) is supplied from innumerable branches of the ILT and IMAX (green arrows). Many veins are seen, including contralateral ophthalmic vein (light blue) and basal vein (dark blue), and deep veins of the brain (pink arrow) and cavernous sinus region veins (dark blue arrows).
After glue injection into a relatively promising IMAX branch, the fistula is still “alive”, though the flow through it has diminished. Thus, veins (dark and light blue arrows) are still seen in the arterial phase. The remaining fistula (red arrow region) cannot be embolized through the myriad tiny feeding vessels (green arrows).
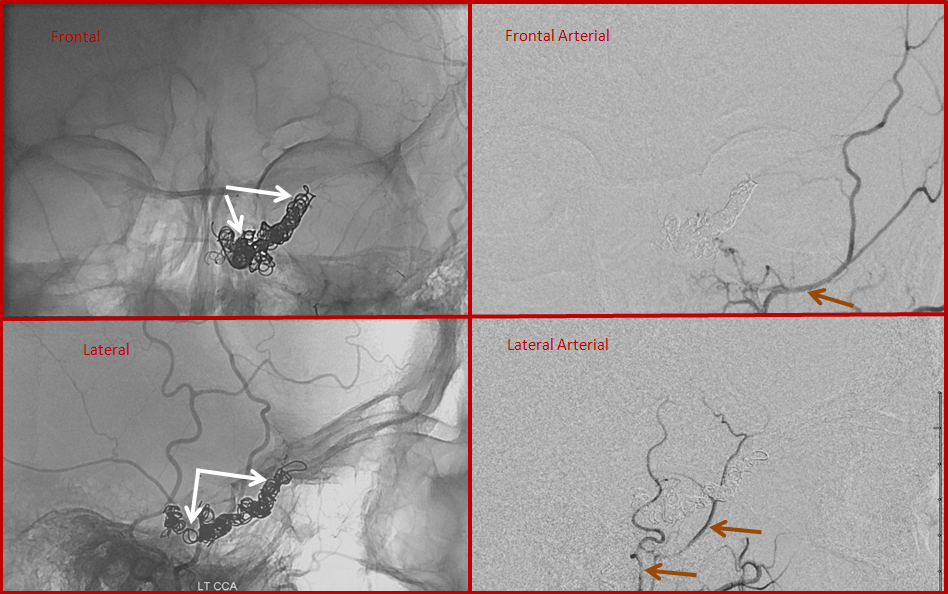
Transvenous approach through the jugular did not reach the cavernous sinus. Therefore, the ophthalmic vein was cannulated directly following a cutdown by an ophthalmic surgeon. An angiocath is sutured into the vein, and a microguidewrire/microcatheter used to catheterize the cavernous sinus. The bottom picture is cavernous sinus venogram, demonstrating the basal vein (dark blue) and ophthalmic vein (light blue arrows). Some coils have already been placed into the sinus. Special care should be taken during this kind of access, since the ophthalmic vein is relatively fragile, and its perforation produces an intraconal hematoma.
Finally, post-embolization views, showing the coils in the cavernous sinus (white arrows) and no evidence of fistula on injections of the external carotid artery (brown arrows). This approach, though technically challenging, can be quite successful when other venues prove unfeasible.
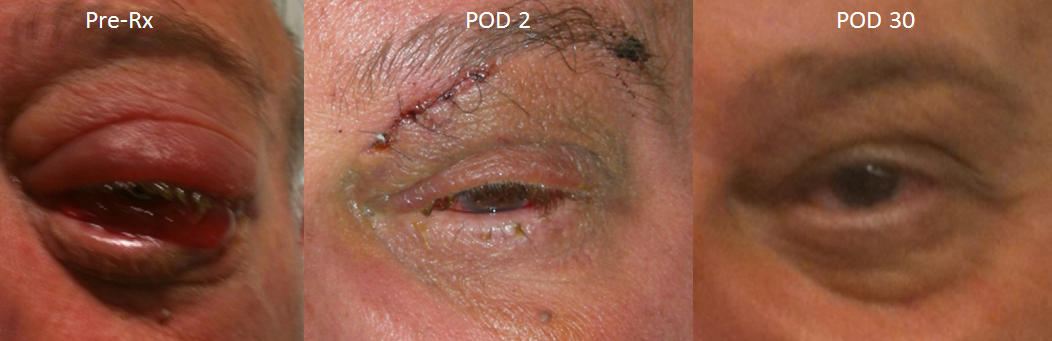
The patient’s eye before and following embolization.
CASE 5 – Tentorial fistula
Thus patient presented with a seizure, preceeded by an aura of scotomata in the right visual field. The fistula is located away from the eye and ear, so there is no tinnitus or exophthalos. Other common symptoms include balance issues.
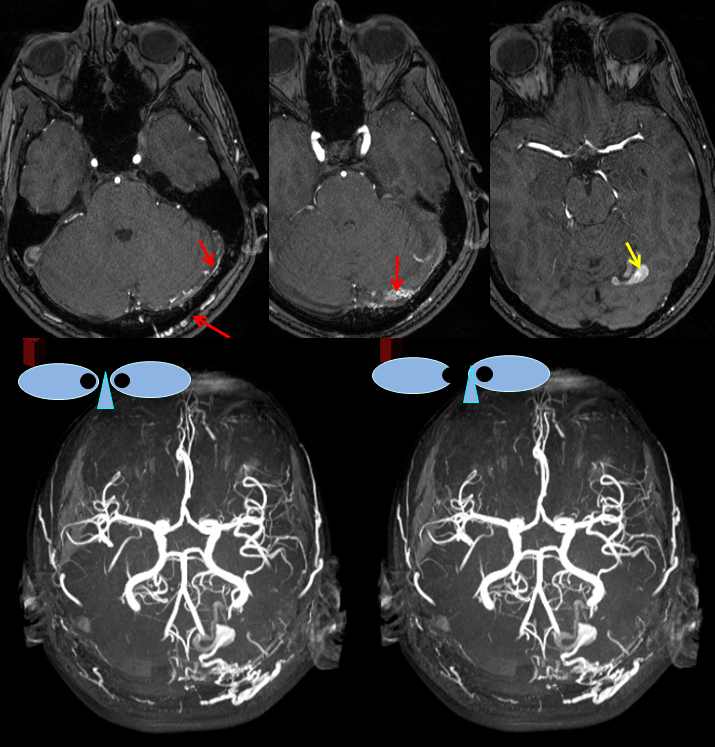
MRA images (top) and stereo MRA composite (MIP) images on the bottom, demonstrating multiple intracranial and extracranial vessels (red arrows) feeding the fistula. An aneurysm near the fistula is suspected (yellow arrows)
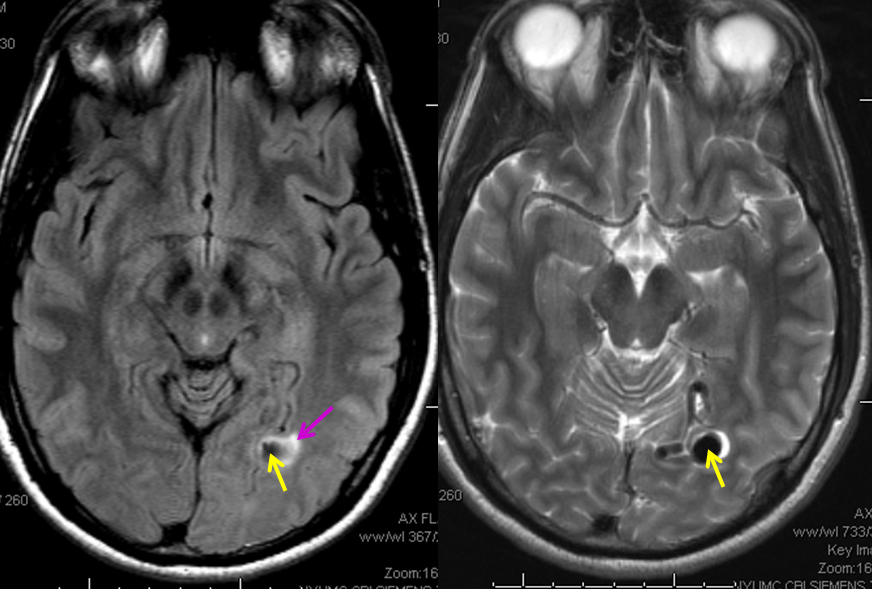
MRI images showing the aneurysm (yellow arrows) associated with the fistula; commonly, these aneurysms are located on the venous side, immediately distal to the fistula; in fact, identiflying such dilatation is helpful in deciding where artery ends and recepient vein begins. There is edema (swelling) present in the surrounding brain (pink arrow), as might be expected based on clinical presenation.
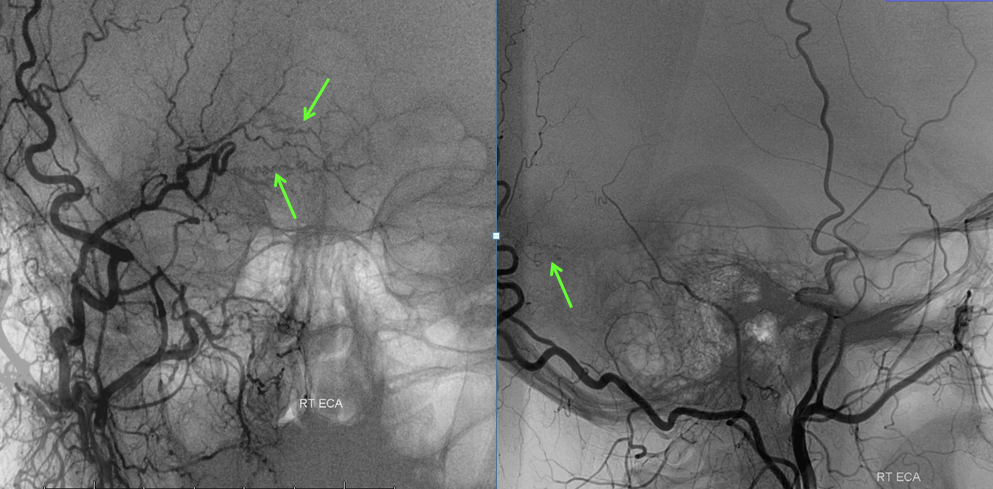
Angiographic view of the right external carotid artery injection, showing small transmastoid
occiptial artery vessels leading to the fistula (just a hint of what’s ahead). The fistula is off to the left.
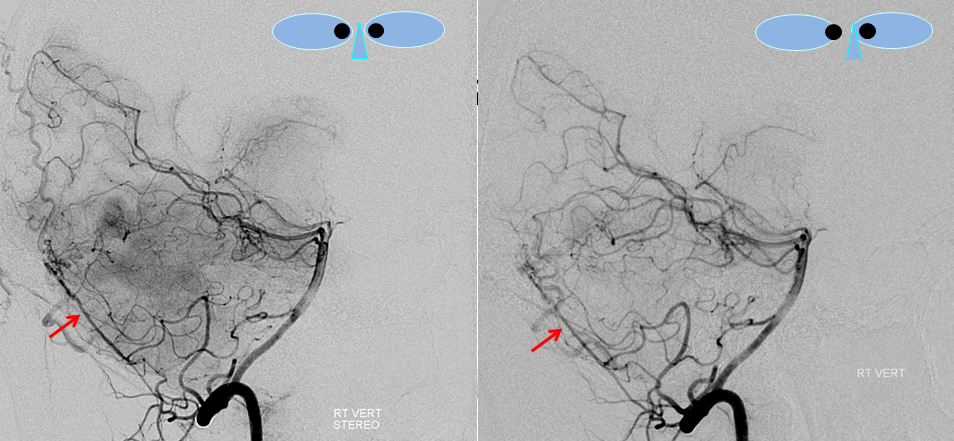
Stereo views of right vertebral artery injection, showing an enlarged artery of the tentorium cerebelli (red arrow), with a hint of the aneurysm (not labeled)
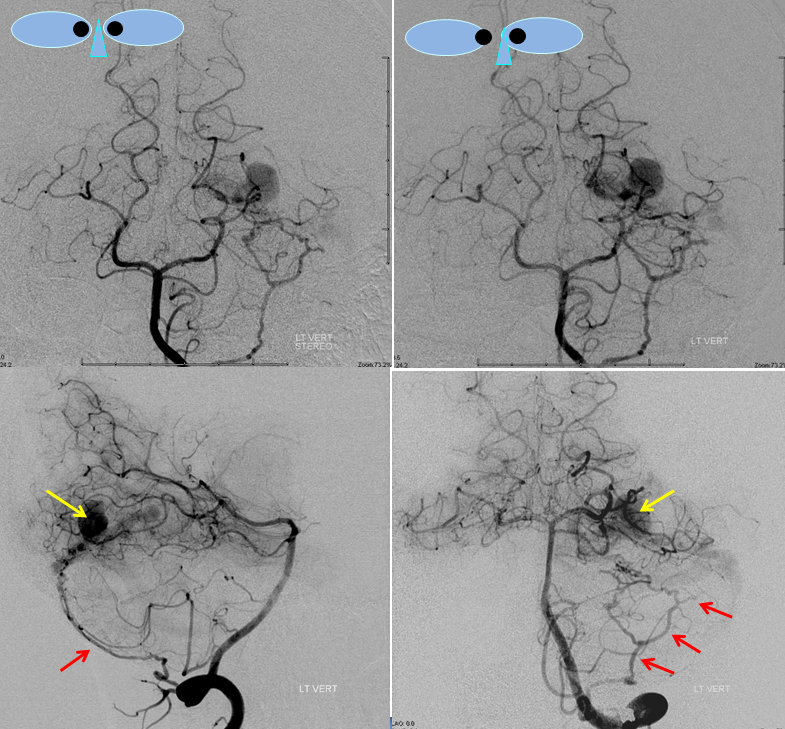
Injections of the left vertebral artery now clearly show the fistula and the associated venous aneurysm (yellow arrows); the fistula is supplied, in this case, by the posterior meningeal artery (red arrows).
An AVI movie of the same injection (lateral vertebral projection)
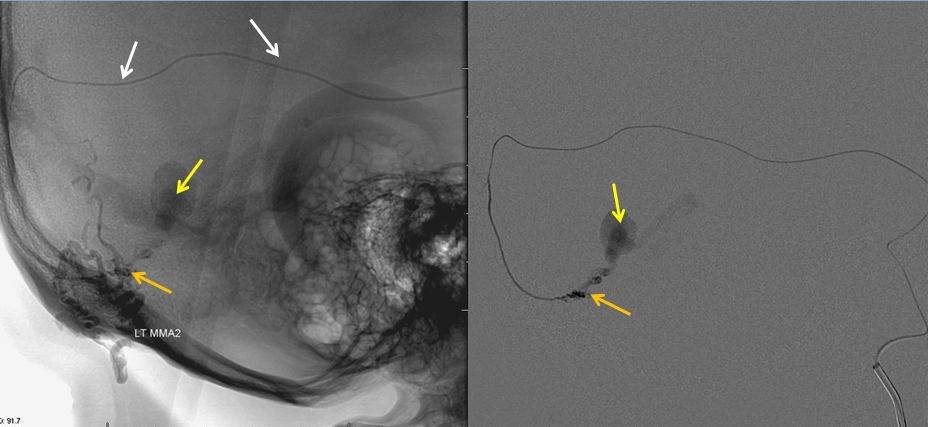
Finally, views of the left external carotid artery, showing transmastoid occipital artery (red) and middle meningeal arteries (pink) supplying the fistula. The fistula point is marked with orange, at convergence of feeding vessels, and venous aneurysm in yellow. Treatment plan was transarterial n-BCA embolization, with goal of filling the aneurysm (thereby assuring that the fistula is also filled).
A microcatheter (white arows) has been navigated into a small branch of the middle meningeal artery (it is obviously safer than going through branches of the vert), and the fistula (orange) is demonstrated from this position. An AVI movie of the same micro-injection is shown below.
Glue was injected through the microcatheter to close the fistula.
A cast of glue is now present in the back of the head (purple arrows) outlining the arteries where the glue went. The aneurysm is not seen, and the fistula remains open and “alive”
The microcatheter has been positioned into another branch of the middle meningeal artery, showing residual fistula and aneurysm. More glue is injected from this position.
A new glue cast (pink arrows), larger than the first one, also shows glue in the aneurysm (yellow arrows). This is very good indication that the fistula is now “dead”.
Post-embolization views of the left common carotid artery, showing that the fistula is gone.
Right vertebral artery injection, also showing no more fistula.
References: Good sources of information on dural AV Fisulas
http://stroke.ahajournals.org/content/33/5/1233.full.pdf+html or http://stroke.ahajournals.org/content/33/5/1233.full
Natural history of untreated or partially treated fistulas with cortical reflux
http://radiographics.highwire.org/content/24/6/1637.full.pdf+html or http://radiographics.highwire.org/content/24/6/1637.full
Comprehensive discussion of DAVF and their treatment strategies, which somewhat differ from ours, but are equally valid.
Neuroendovascular management of dural arteriovenous malformations
McConnell, Kathleen A; Tjoumakaris, Stavropoula I; Allen, Jason; Shapiro, Maksim; Bescke, Tibor; Jabbour, Pascal M; Rosenwasser, Robert H; Nelson, Peter K 2009 Oct;20(4):431-439, Neurosurgery clinics of North America — our own NYU contribution to the cause
Back to Parent Page — Techniques of Dural Arteriovenous Fistula Embolization