Case collaboration with Chandra Sen, M.D. and with ever amazing guidance of Peter Kim Nelson, MD
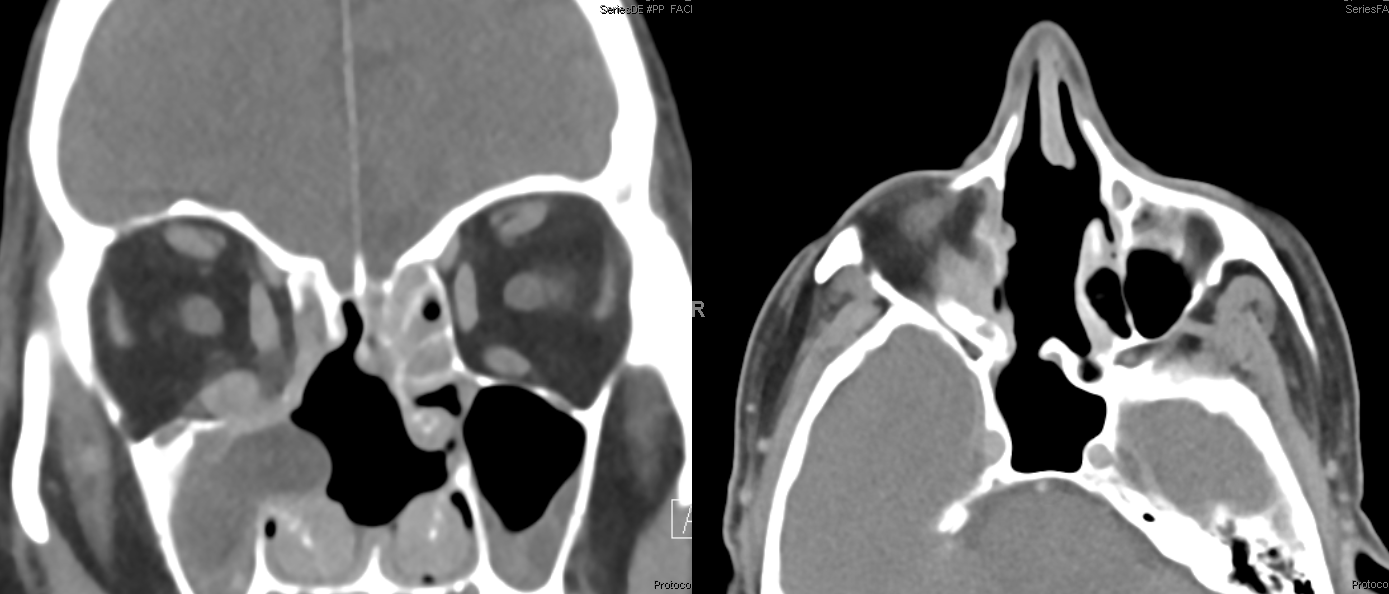
The value of preoperative embolization is best demonstrated in cases where it is more essential rather than more optional. This patient presents with painless right proptosis. There is a history of remote hypervascular primary carcinoma (type withheld for patient privacy reasons).
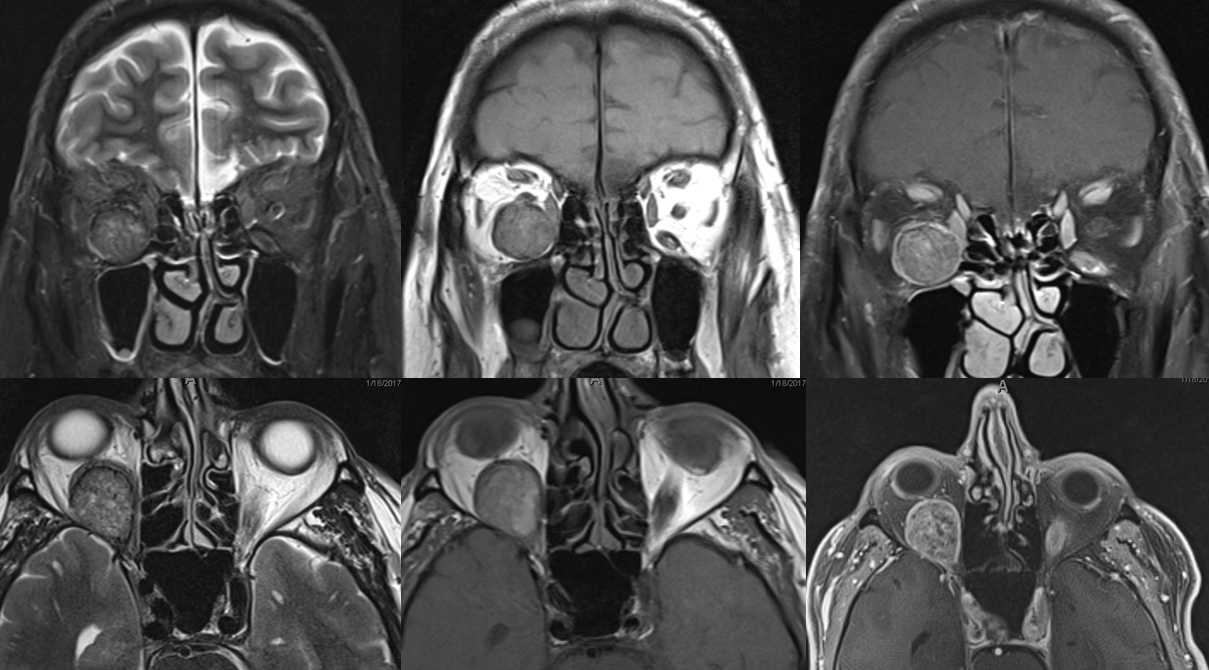
MRI demonstrates enhancing retrobulbar mass attached to the inferior rectus
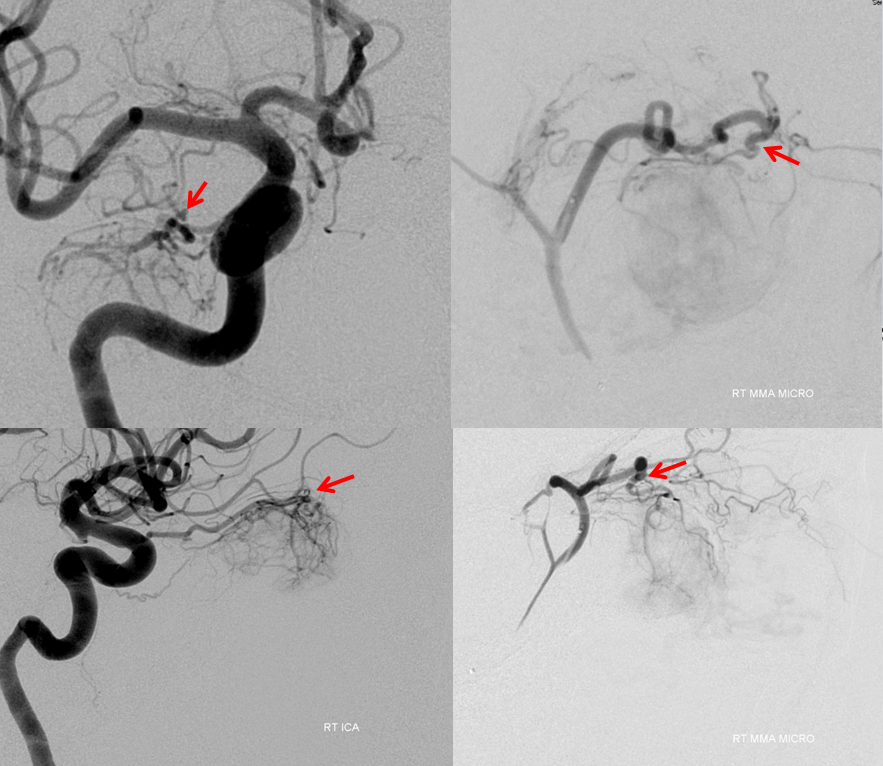
Angiogram shows prominent supply from the ophthalmic artery. Although the main pedicle supplying the mass is relatively distal (red), there is a proximal feeder (purple) adjacent to the expected location of the central retinal artery, as well as supply via the dorsal ophthalmic artery (white) from the ILT
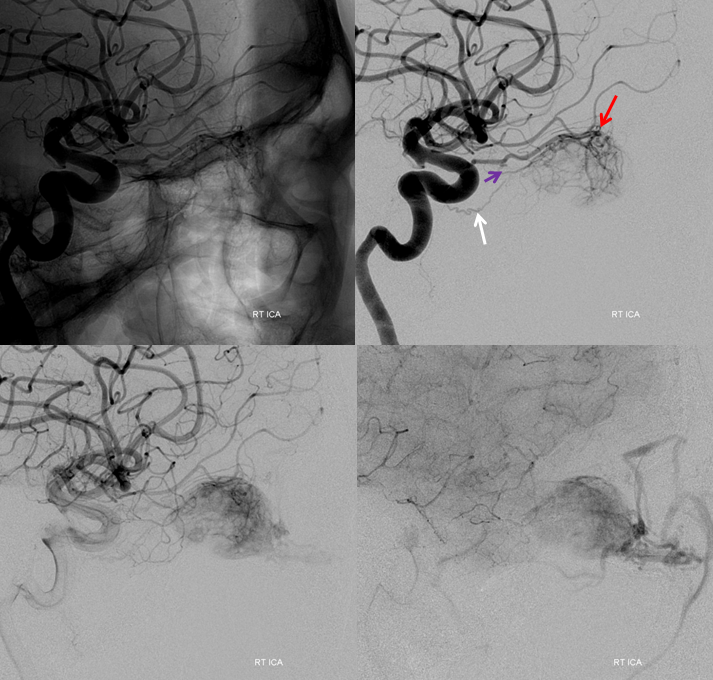
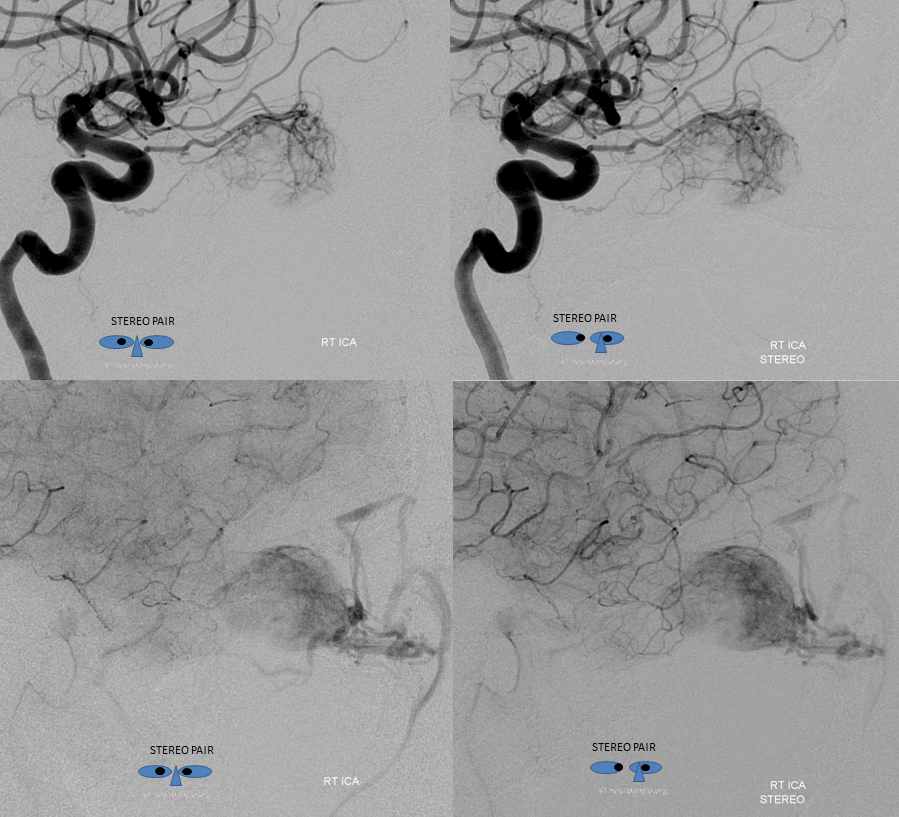
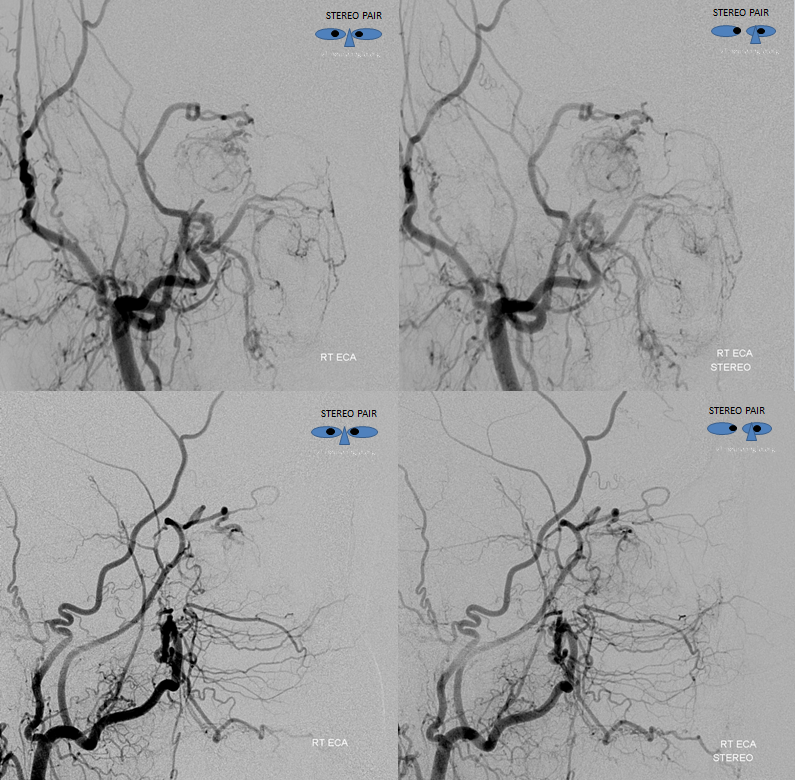
Lateral stereos in early arterial and parenchymal phases. These are pretty awesome
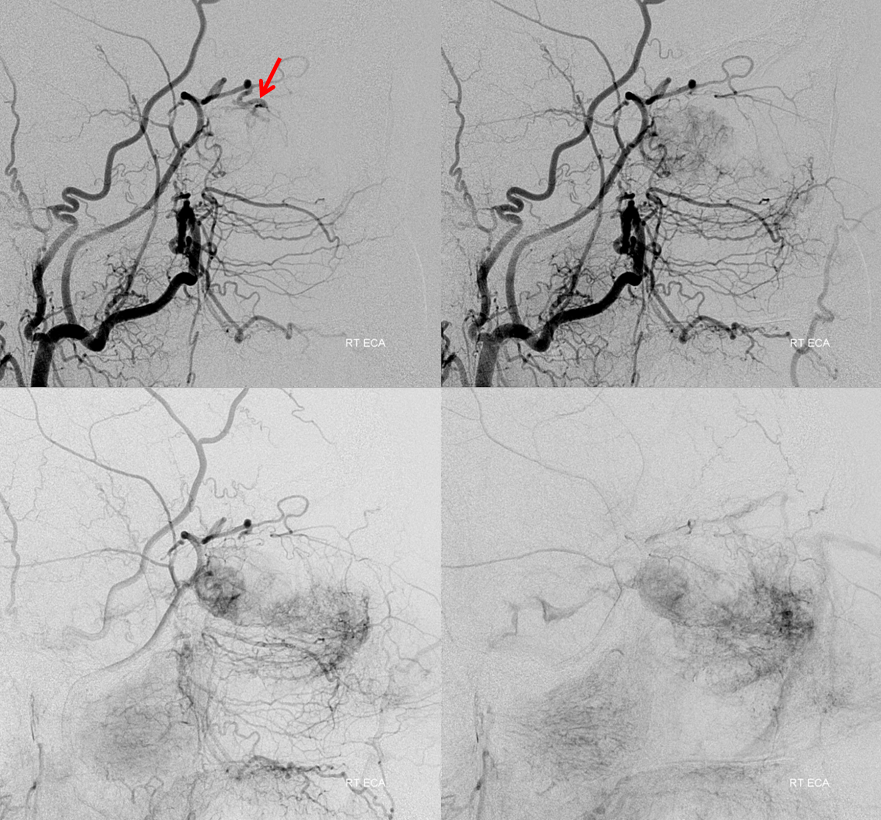
The above may not look too promising. Distal ophthalmic catheterization with particle embolization is not unreasonable in this case, however the external carotid injections provide an even better avenue. The tumor is opacified via the meningolacrimal branch. It is critical to recognize that both the ophthalmic and meningolacrimal branches (of the middle meningeal artery) come together to a common pedicle (red) which ultimately supplies the bulk of the mass. Notice also a very small feeder proximally (yellow)
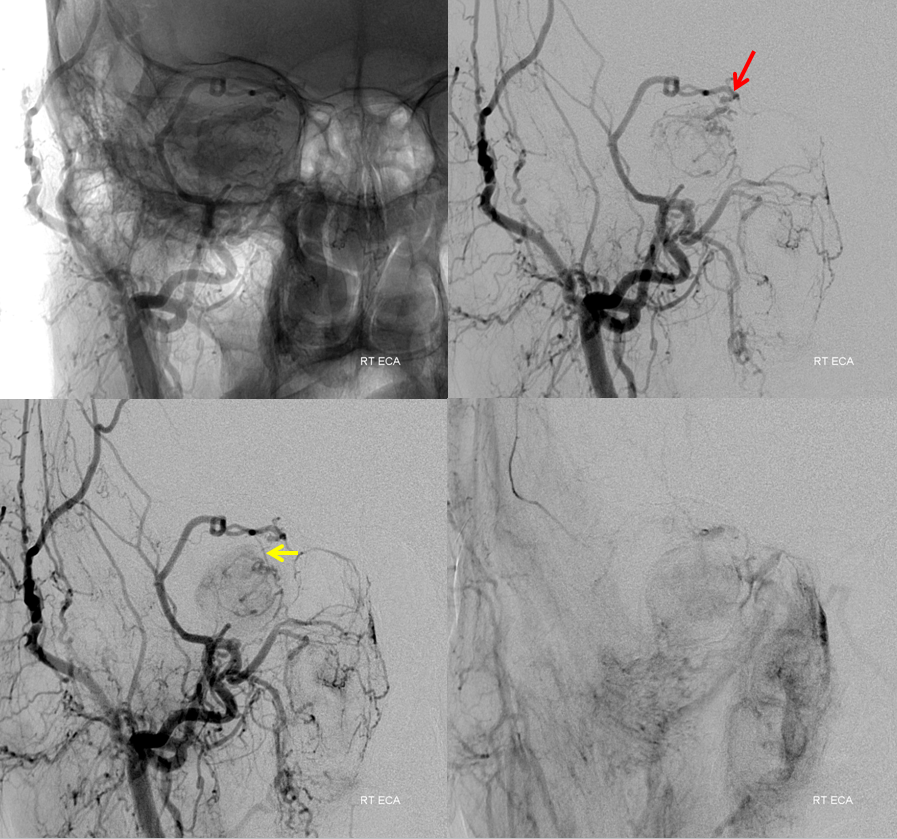
Lateral views of the external carotid injection. Notice intermittent visualization of the common tumor supply pedicle (red). It is not seen in the images on the right due to partial spasm of the proximal ECA.
Stereo pairs
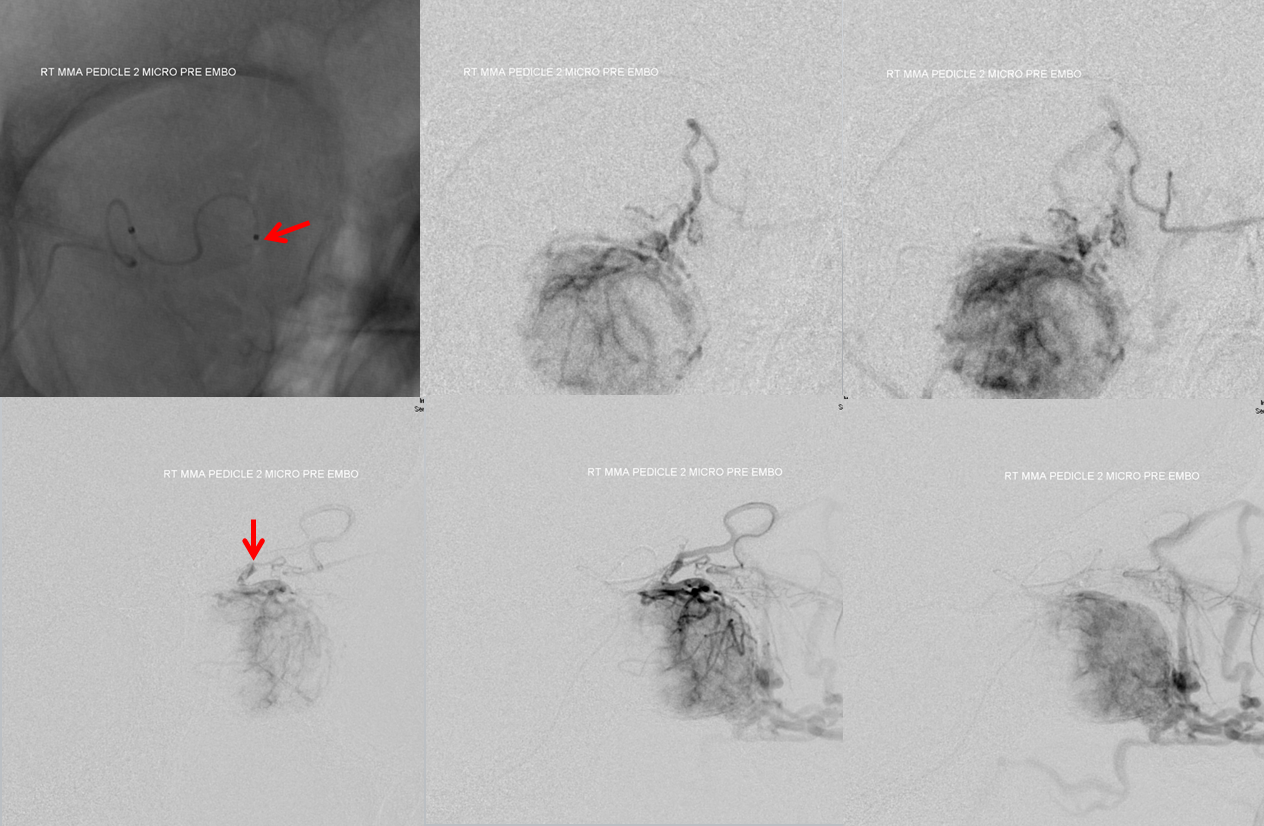
The embo starts by securing a position in the smaller, more proximal meningolacrimal branch (yellow). This allows for embolization of the posterior portion of the mass, which is also supplied by proximal ophthalmic and dorsal ophthalmic branches which, due to their proximal location in relation to the central retinal artery, would not be wise to use as embolization routes.
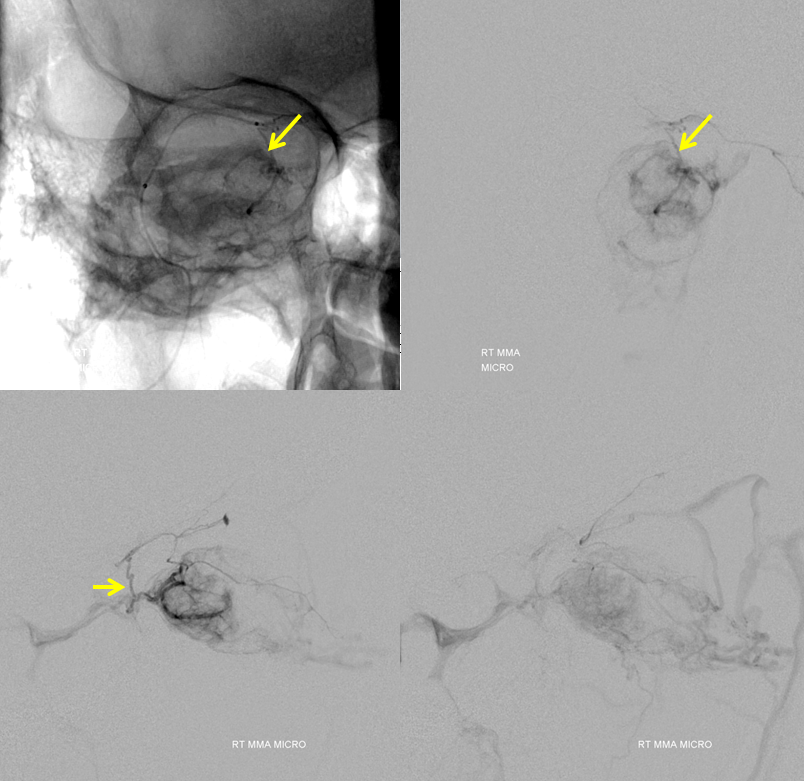
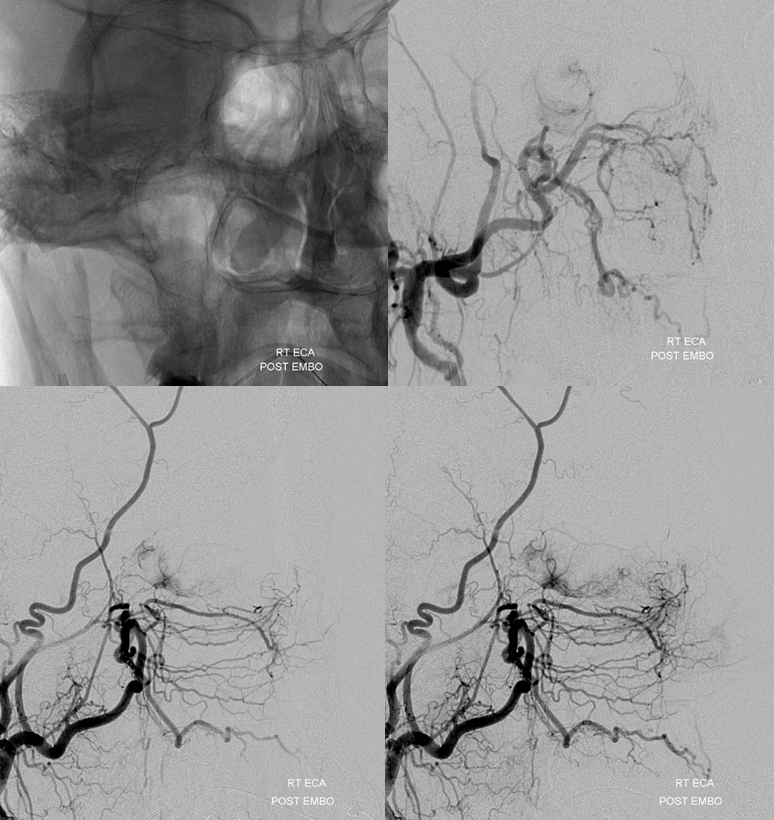
Embolization proceeds with small PVA contour particles (45-150 microns). Following embo in this position, the distal portion of the meningolacrimal artery is microcatheterized. The common pedicle with the ophthalmic artery is well-seen (red). However, there is too much proximal ECA spasm to carry particles from this position into the tumor. In order to achieve meaningful embolization, a much more distal catheterization just proximal to or into the common pedicle is necessary.
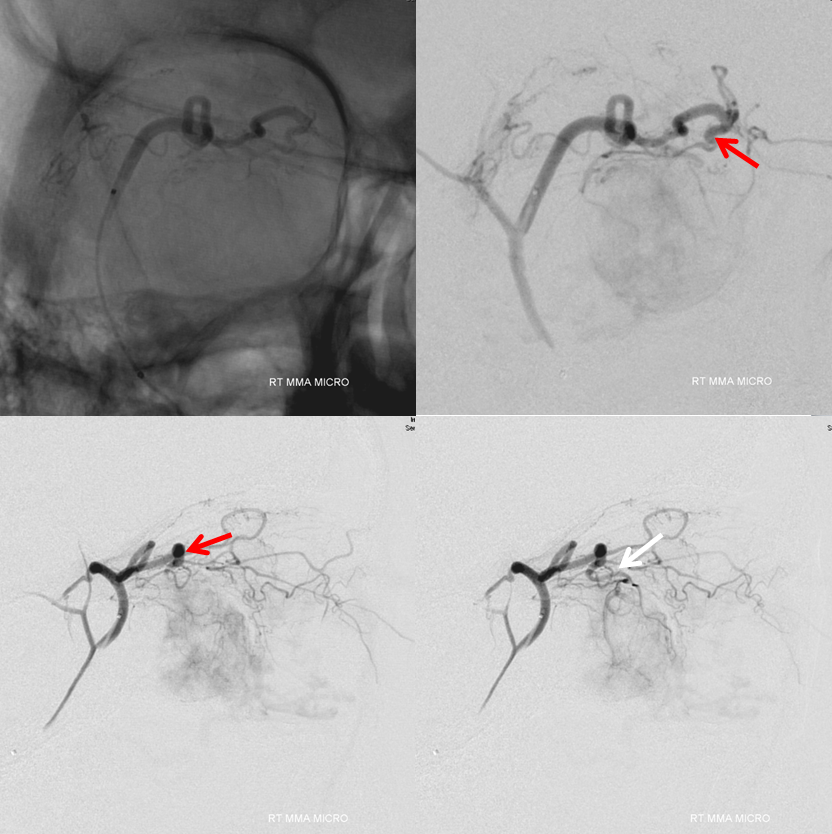
Here are side by side images of the ophthalmic and menigolacrimal contributions to the tumor, showing the same common pedicle (red)
Following distal catheterization, there is still prohibitive ECA spasm. However, from this position the ophthalmic artery inflow now allows the particles to be carried into the tumor bed. This allows for the same efficiency of tumor embolization as would be achieved from catheterization of the ophthalmic artery itself, without the need to do so.
After embolization with 45-150 micron Contour PVA particles, residual and quite minor supply still comes from the proximal ophthalmic and the dorsal ophthalmic branches. These are left alone given what was perceived as prohibitively high hazard to the retinal artery
Ophthalmic artery injection demonstrating the same branches with remaining supply as were seen on the preoperative views. The orbital blush is shown by pink arrow. This, by the way, does not mean that vision is preserved — the choroid is supplied by a different set of arteries than the central retinal (central retinal is usually more proximal). But it is a good sign.
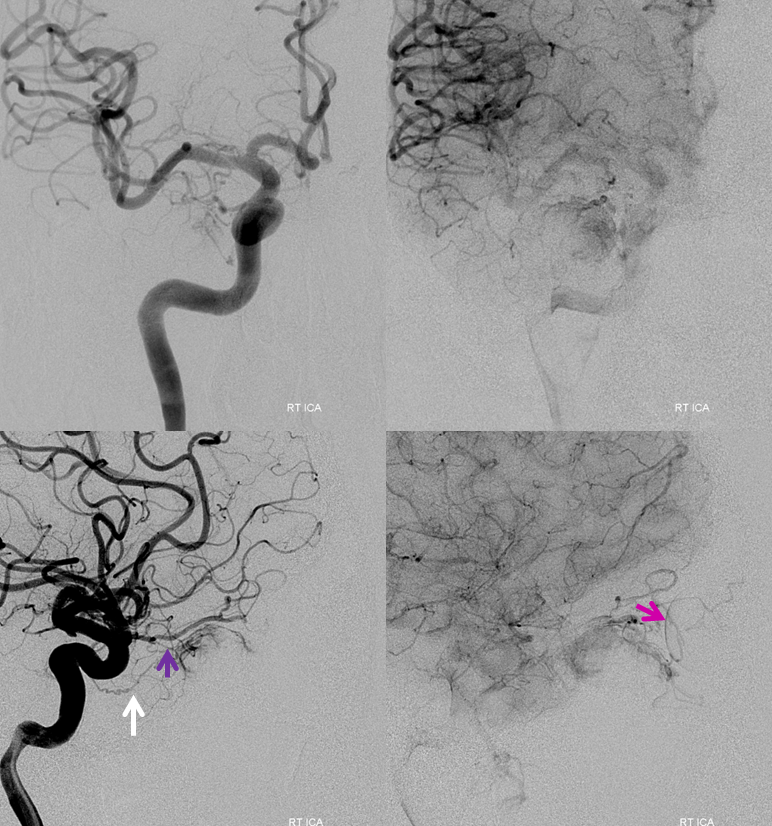
Several months post partial resection. Residual mass prior to chemo. Proptosis has resolved and normal baseline acuity was never changed.
See other Preoperative Tumor Embolization Cases
