Case Courtesy Dr. Eytan Raz
Most of the time, there is no MRI evaluation of acute stroke. Its CT scan, then maybe CTA and/or CT perfusion. CTs are faster to get and there are more of them then MRs.
Here is a young patient with left hemibody numbness. Usually a lacune, if its a stroke at all. Cortical branch (“large” or “medium” size vessel) occlusion is not suspected, so an MR is done a few hours later. The result is an awesome example of what hyperacute stroke looks like on MRI, MRA, and MR perfusion.
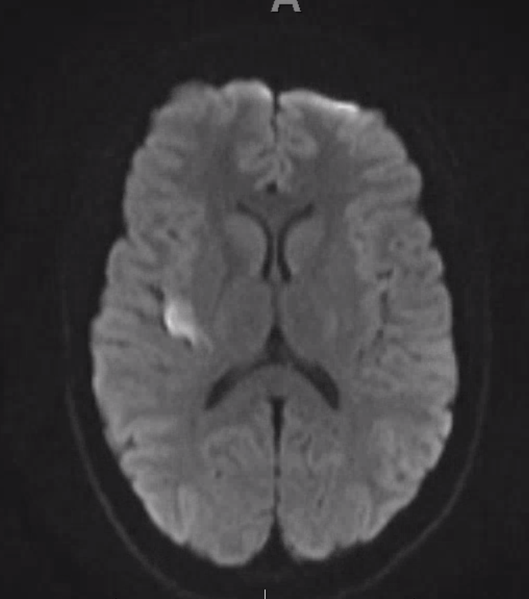
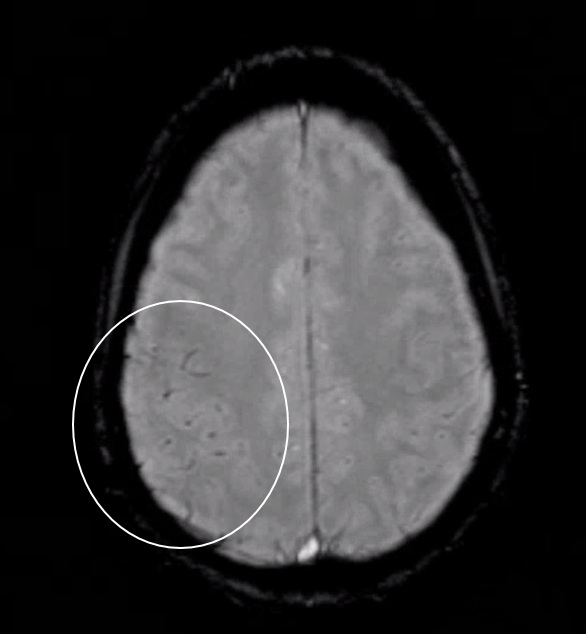
Diffusion shows a small right opercular lesion
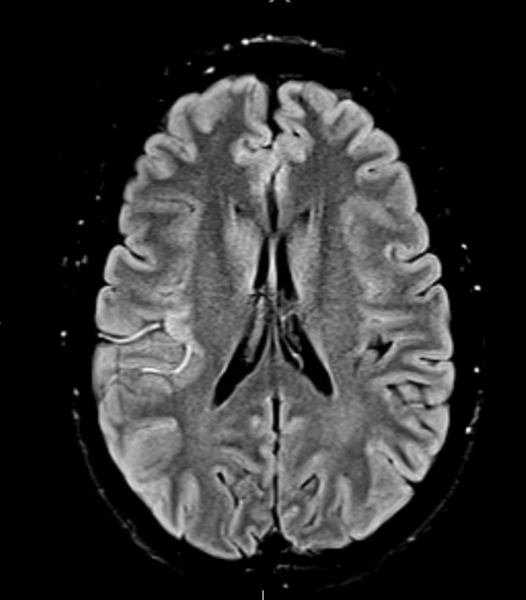
FLAIR shows “slow flow” in several MCA M3 branches emerging from the posterior Sylvian Fissure
Susceptibility-weighted imaging (SWI) shows embolus (with blooming artifact due to increased deoxyhemoglobin of red blood cells trapped in the clot)
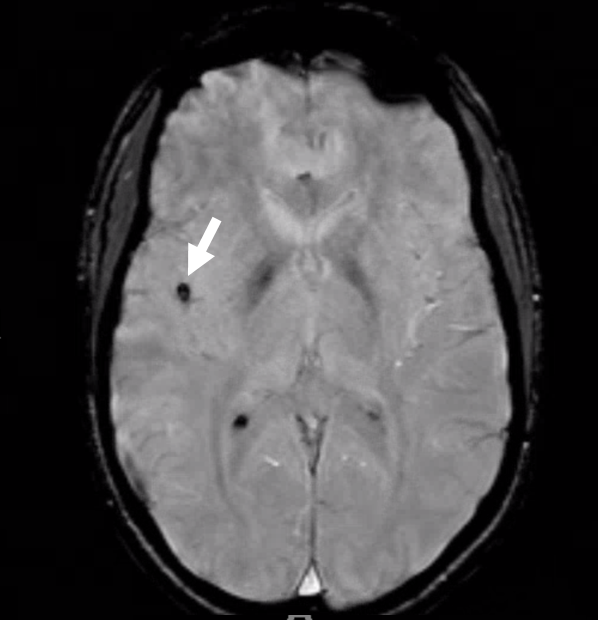
Slightly higher, there is susceptibility in veins that have more deoxyhemoglobin due to higher oxygen extraction
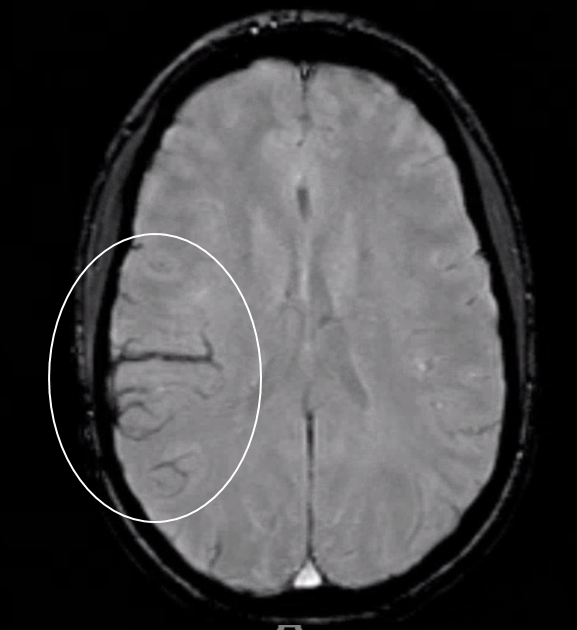
higher still, there is more deoxyhemoglobin in the arteries of the watershed area — ACA/MCA leptomeningeal anastomoses retrogradely supplying region distal to occlusion
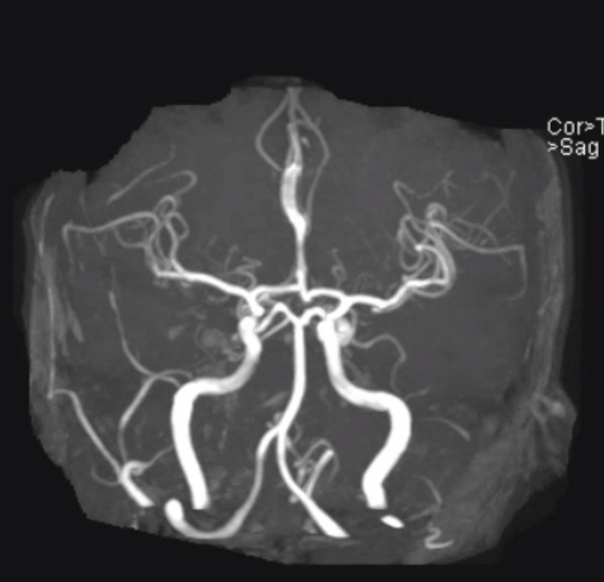
MRA is “negative” — the occlusion is too distal to be seen
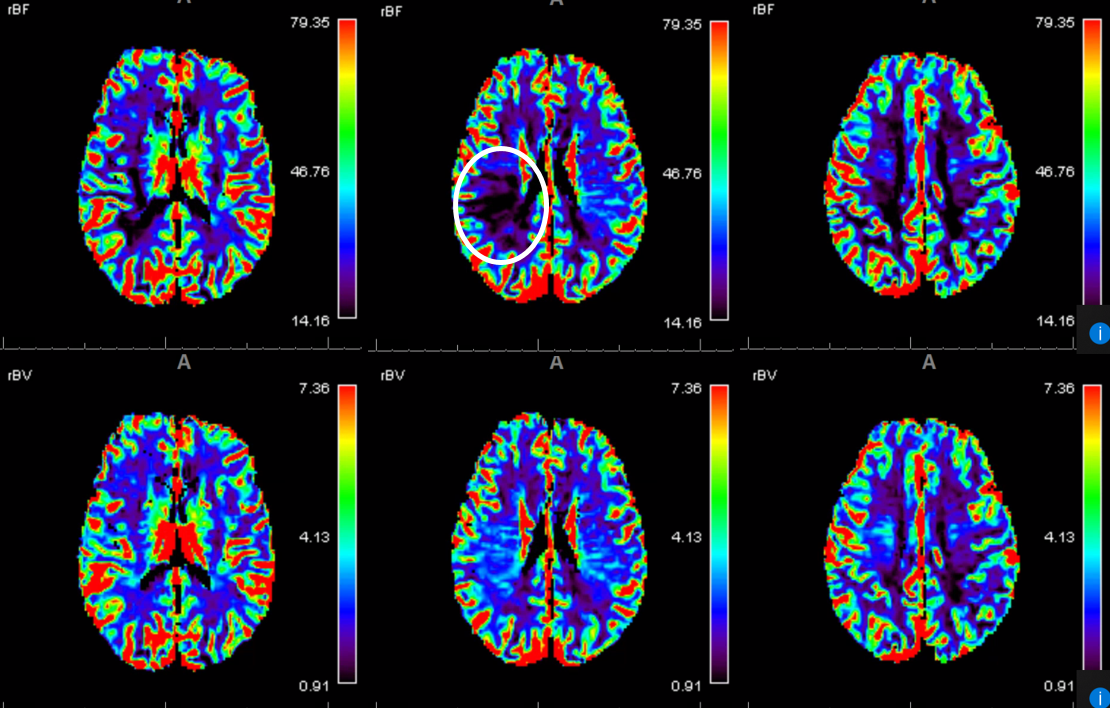
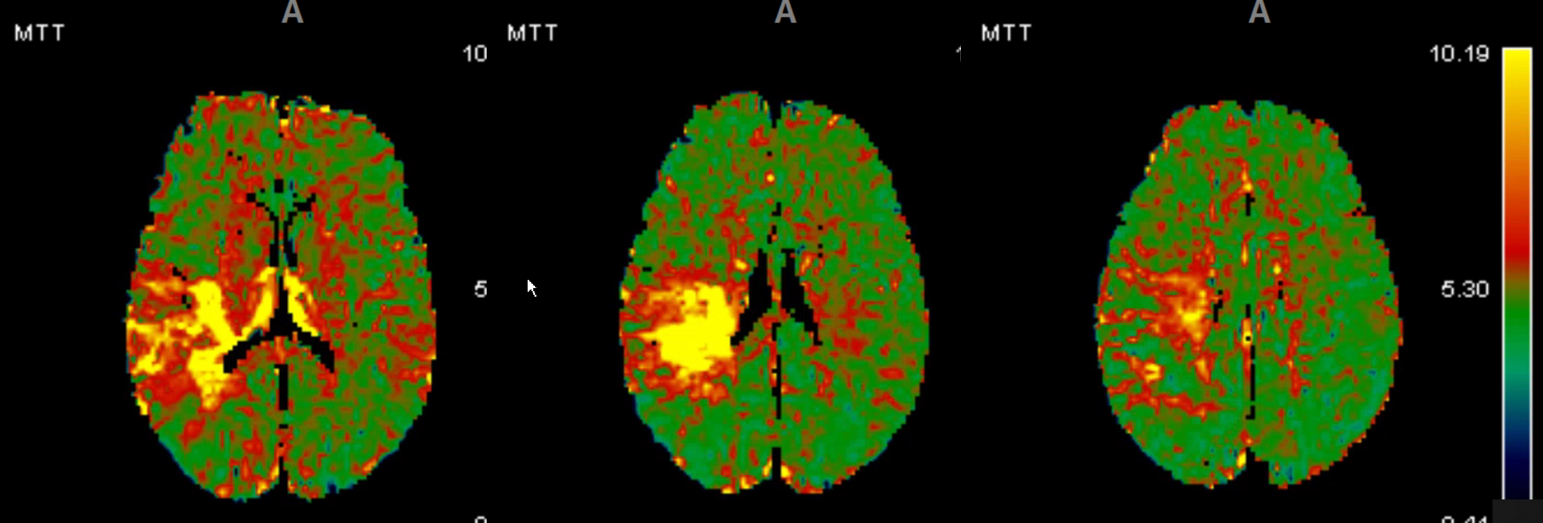
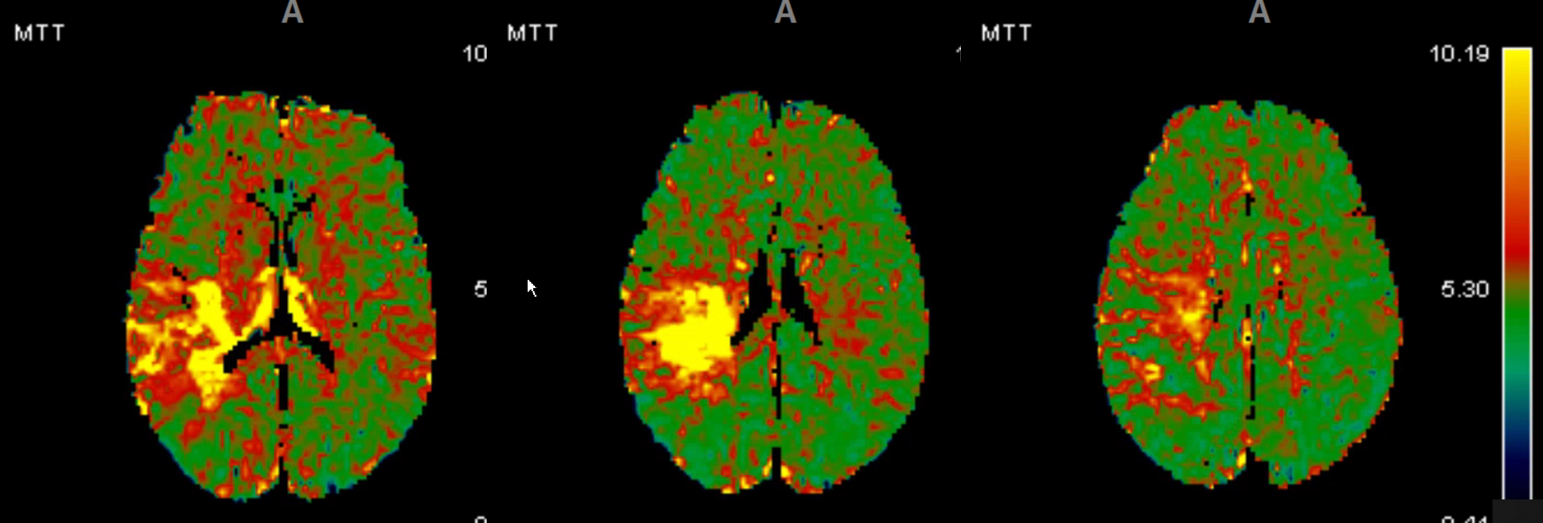
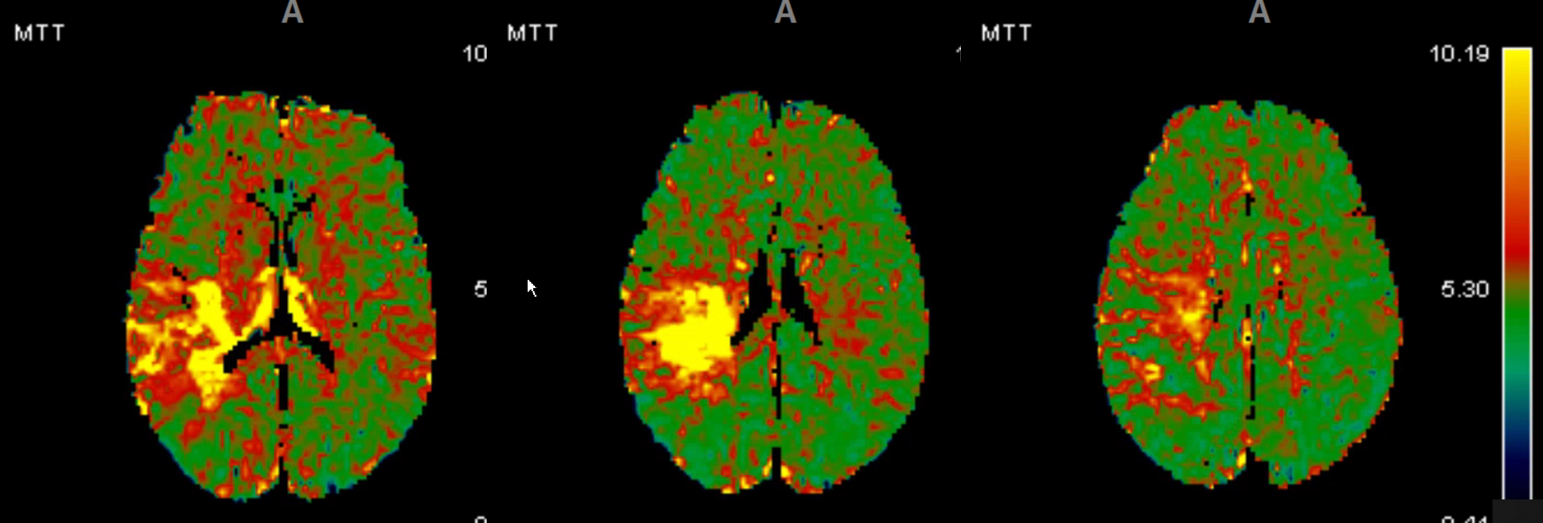
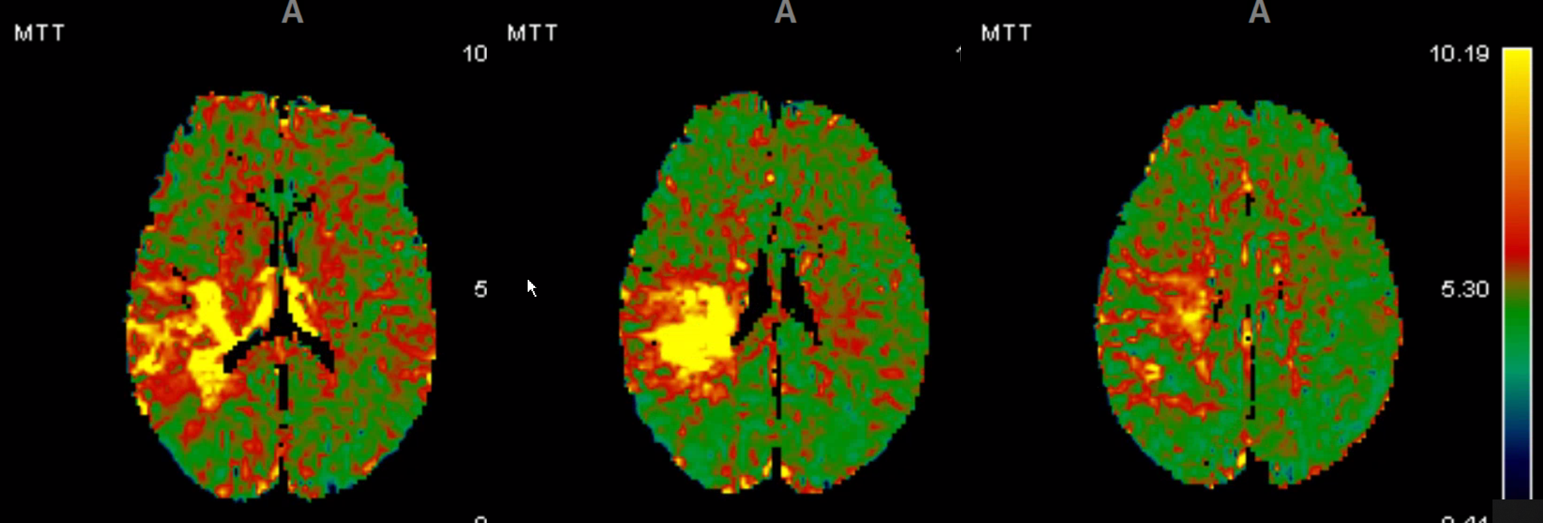
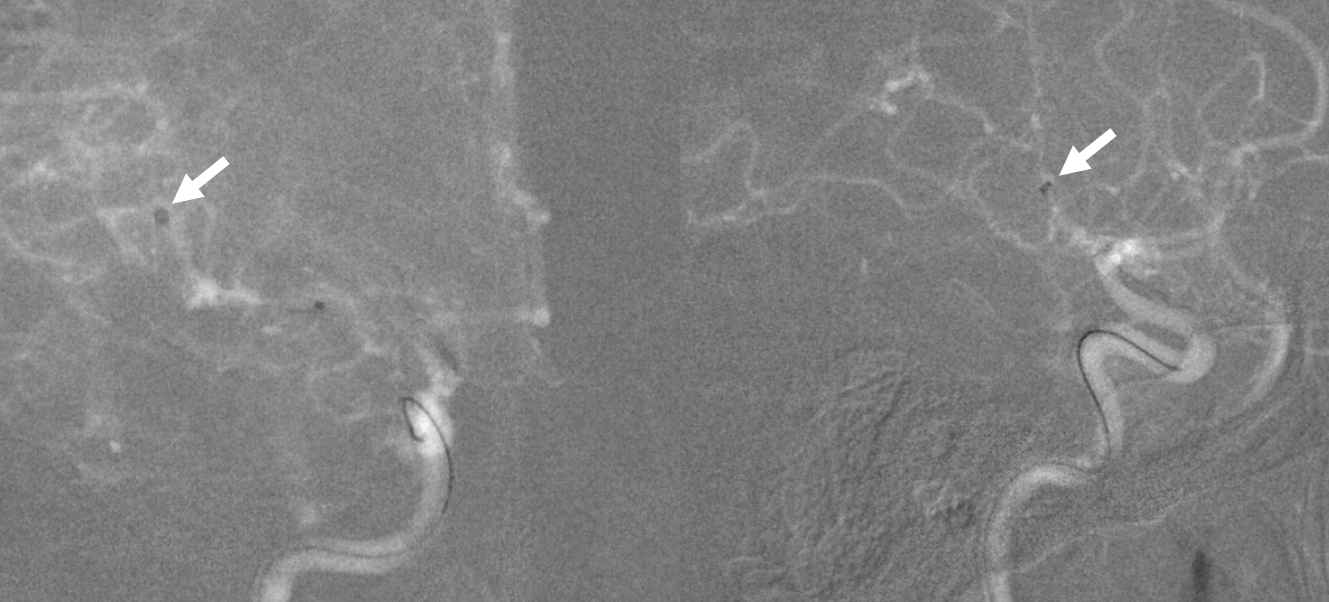
Now for MR perfusion. Reduced CBF (top row), preserved CBV (bottom row)
Increased MTT
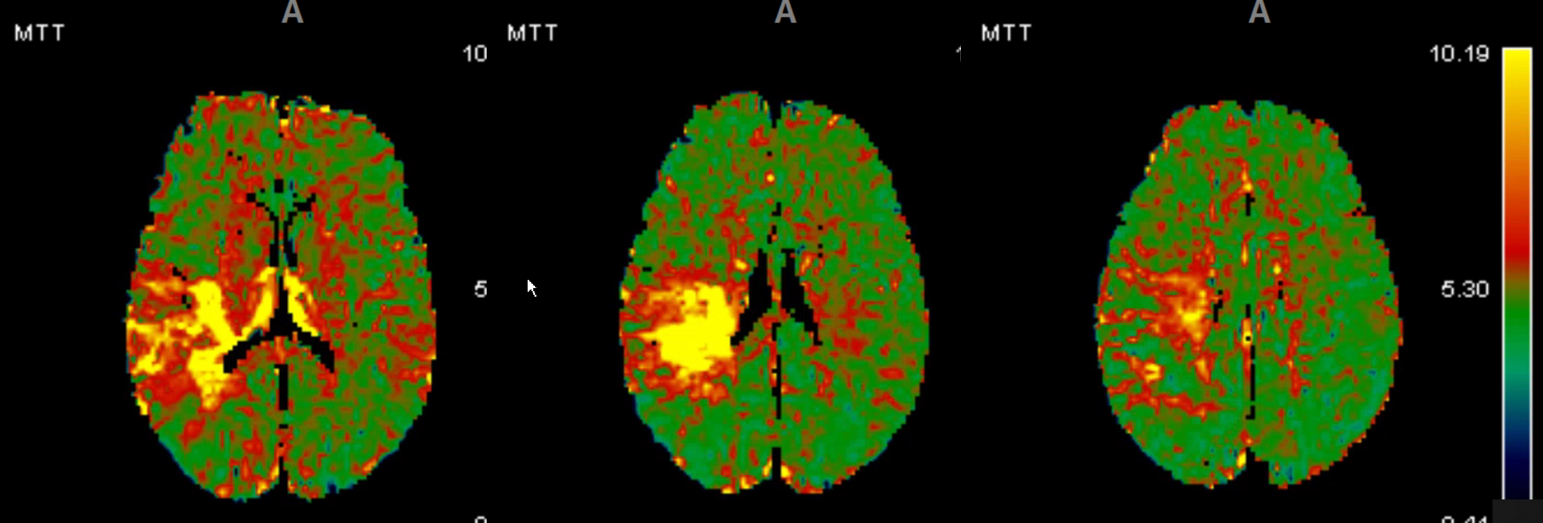
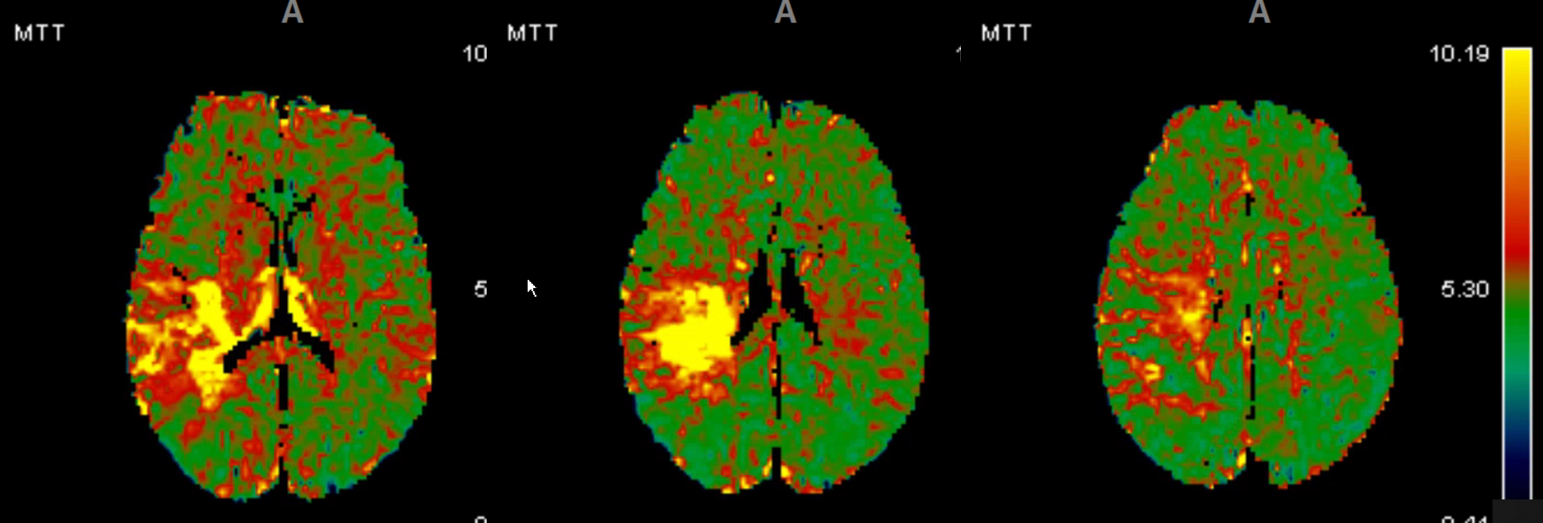 Increased “delay”
Increased “delay”
The sum total of MR finding is a beautiful set of classic penumbral images. Tiny diffusion core. Lots of penumbra. Lots of information seen on DWI and perfusion related to collateral reconstitution anatomy and physiology.
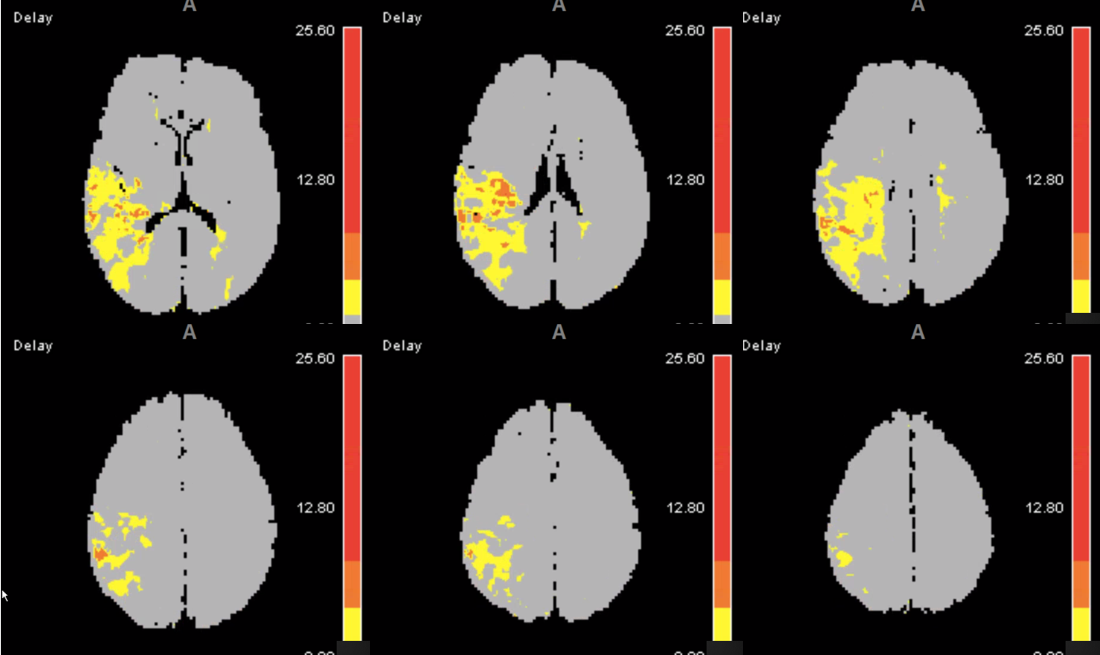
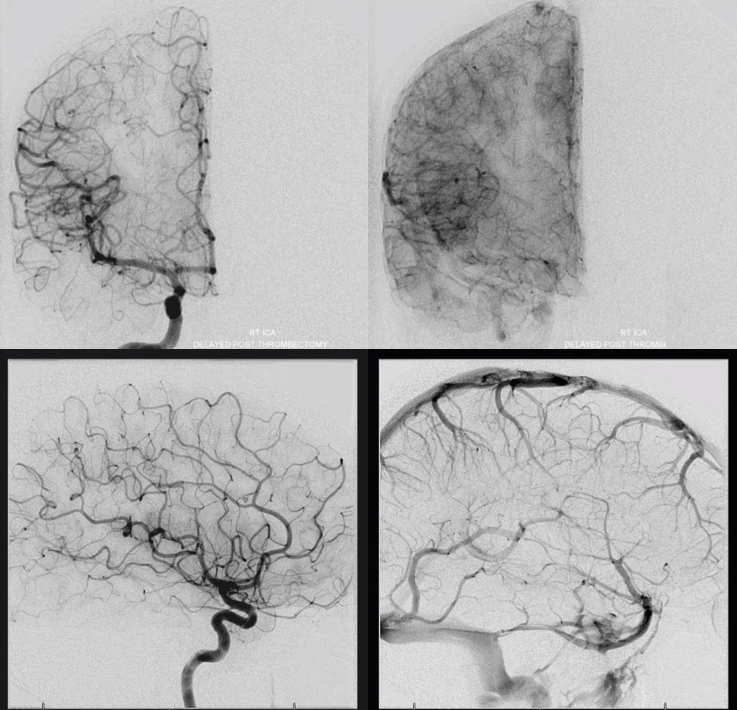
Patient is taken for thrombectomy right after the MRI — because that’s what we do. Angio shows embolus (arrow) in distal M2/proximal M3 segment, supplying parietal and parieto-occipital territories. Notice absence of true MCA “bifurcation” — life does not read books. The MCA can look like whatever it wants.
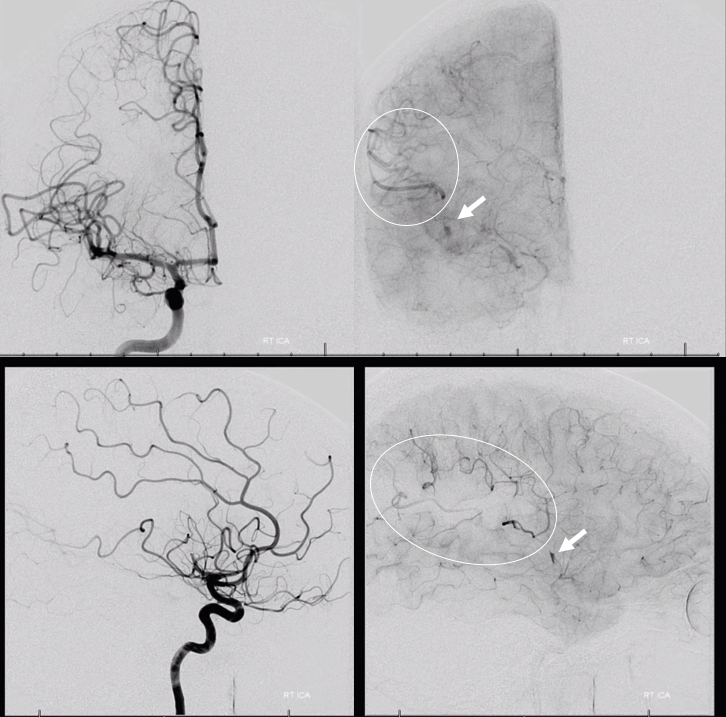
Sofia 5 aspiration catheter at the embolus location
Post reperfusion
Conclusion: Great MR images of acute stroke on many sequences. Its all about penumbra — there is no time cutoff for thrombectomy if there is still brain to save.
See other distal thrombectomy cases here
Literature:
