A great case, in collaboration with Dr. Eleanore Kim of NYU Oculoplastic Surgery
A rare opportunity to help someone with an orbital AVM. There are important anatomical, strategical, and technical points here. For anatomical background to much of what happens here, see Ophthalmic Artery page.
Presentation is progressive pain, proptosis, diplopia, and glaucoma, exhausting medical options
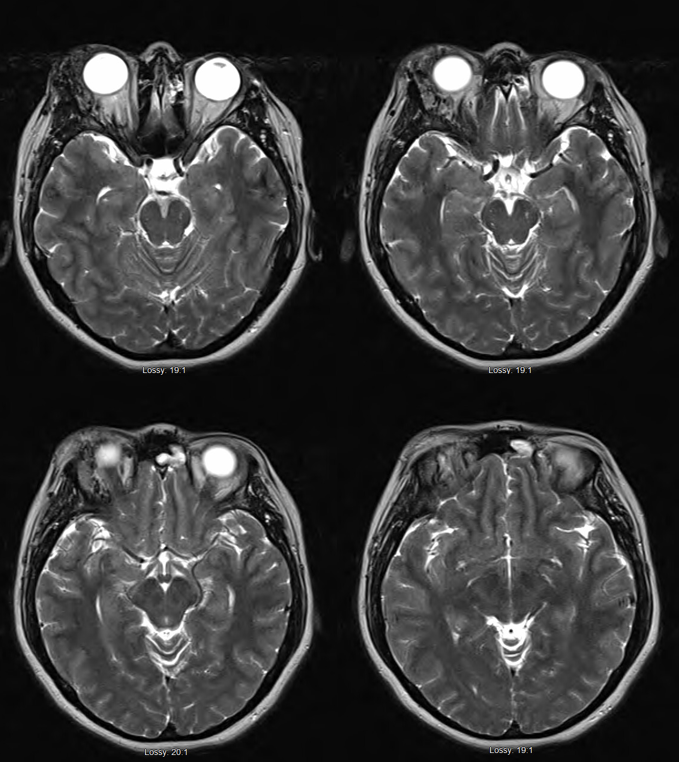
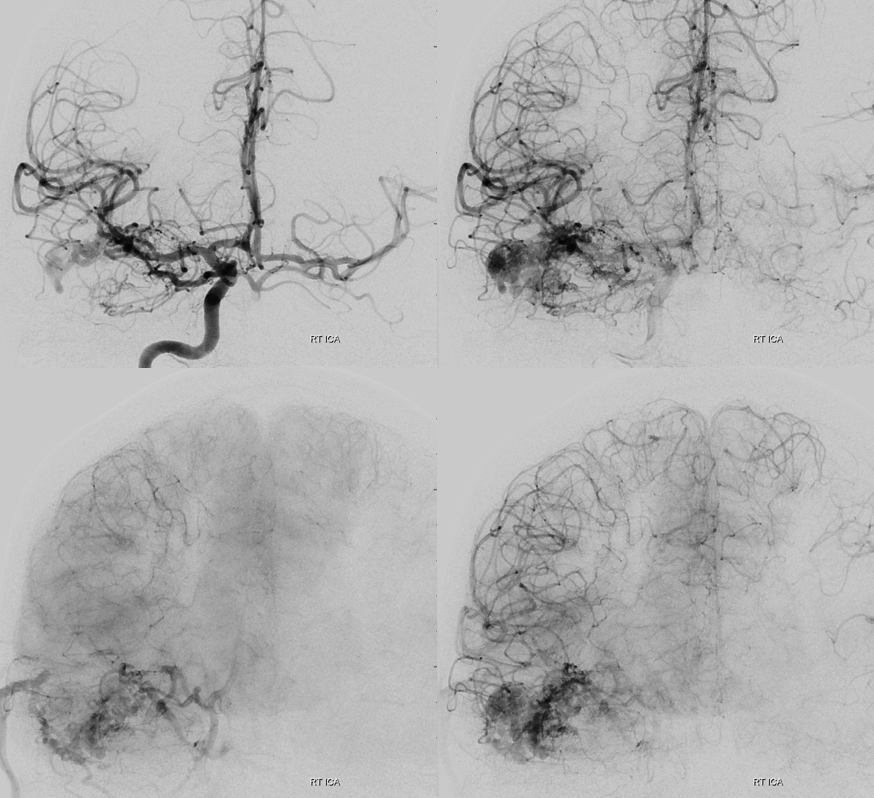
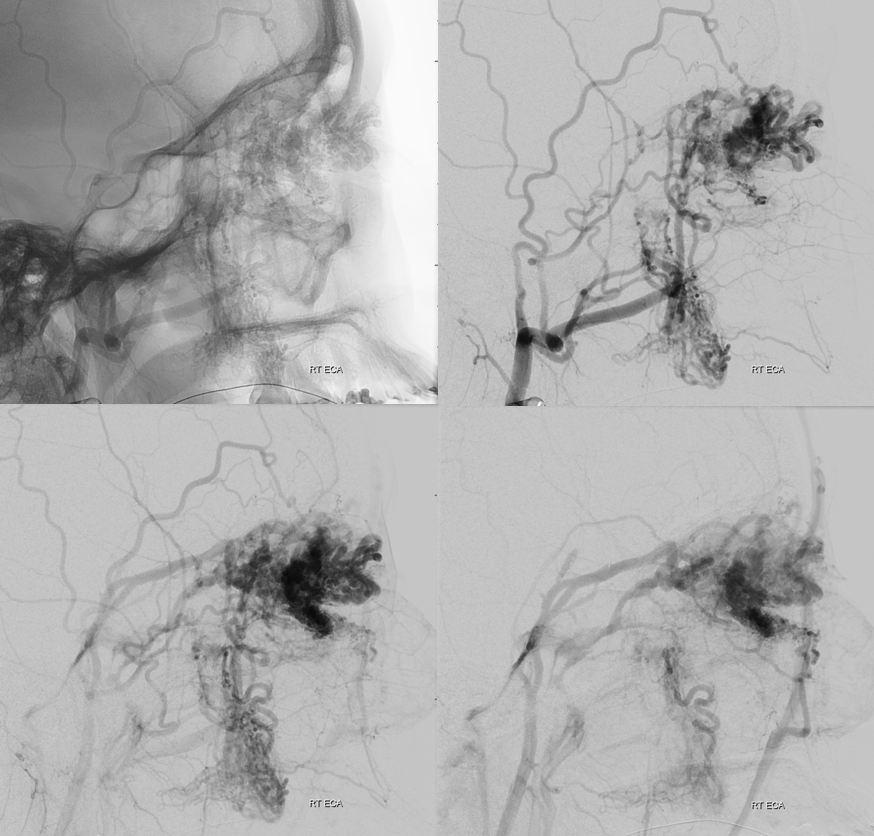
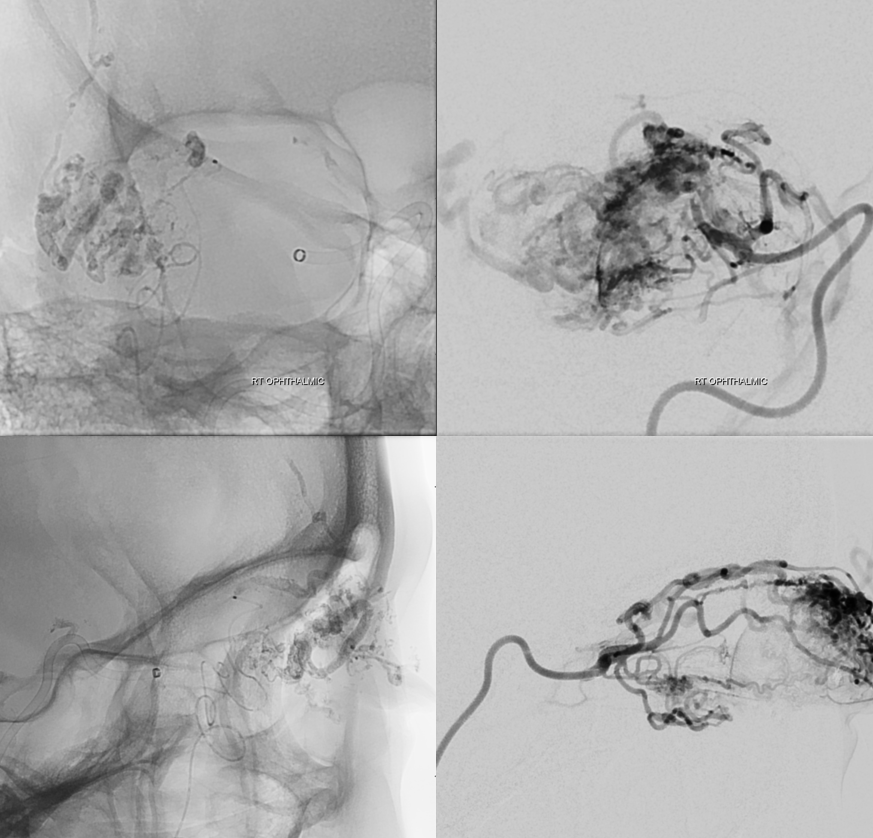
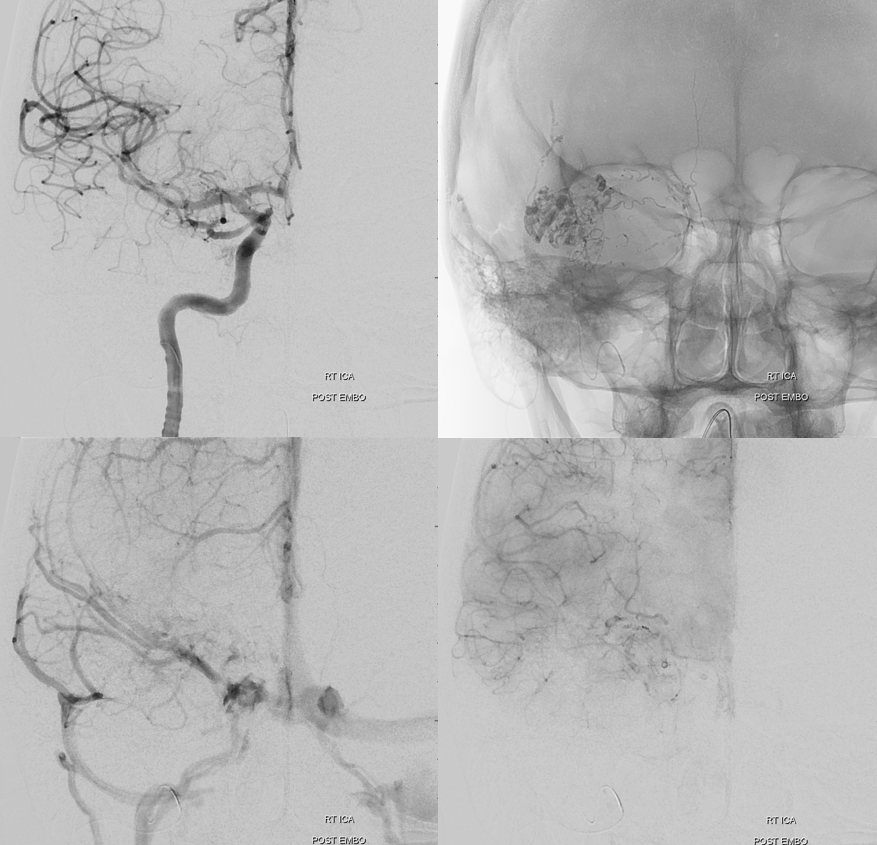
Diagnostic angio
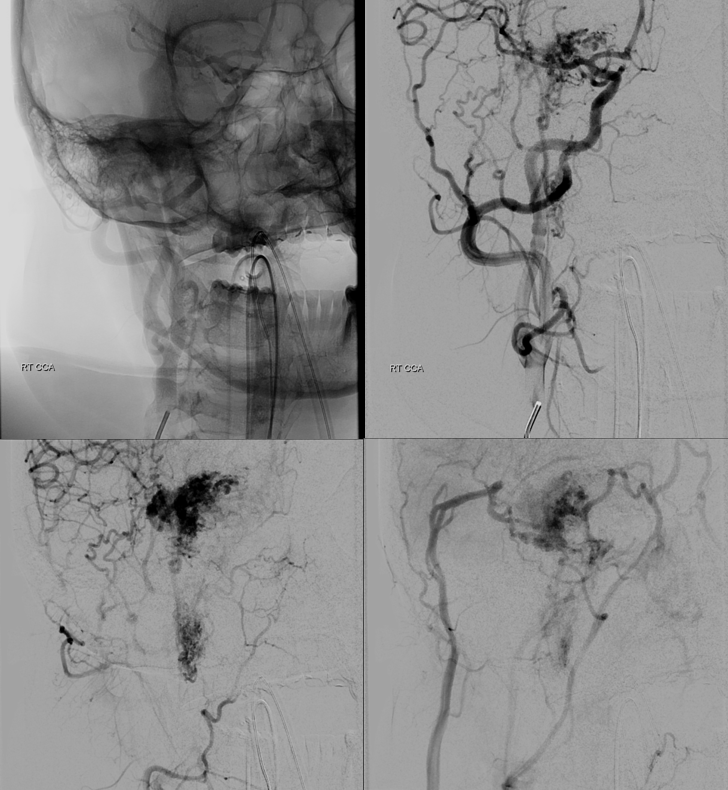
Old machine…
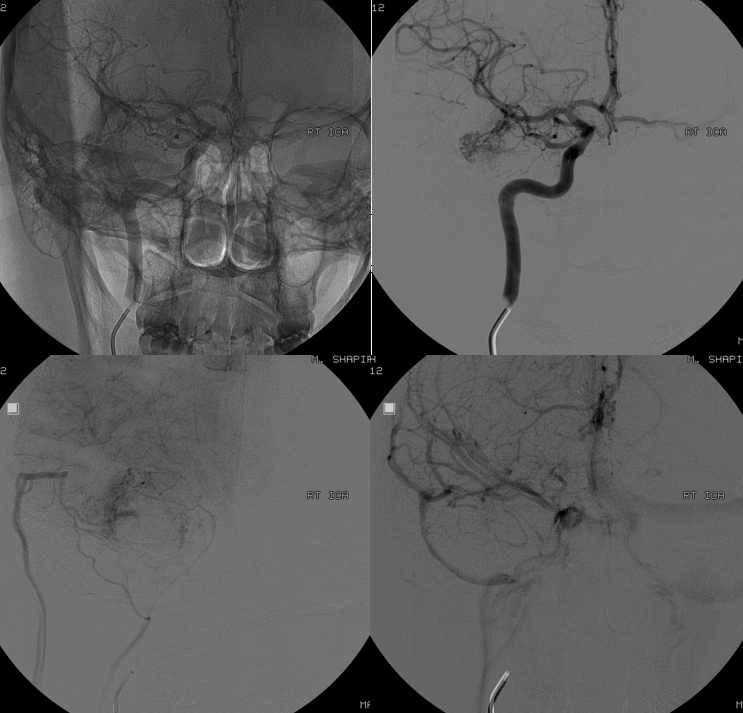
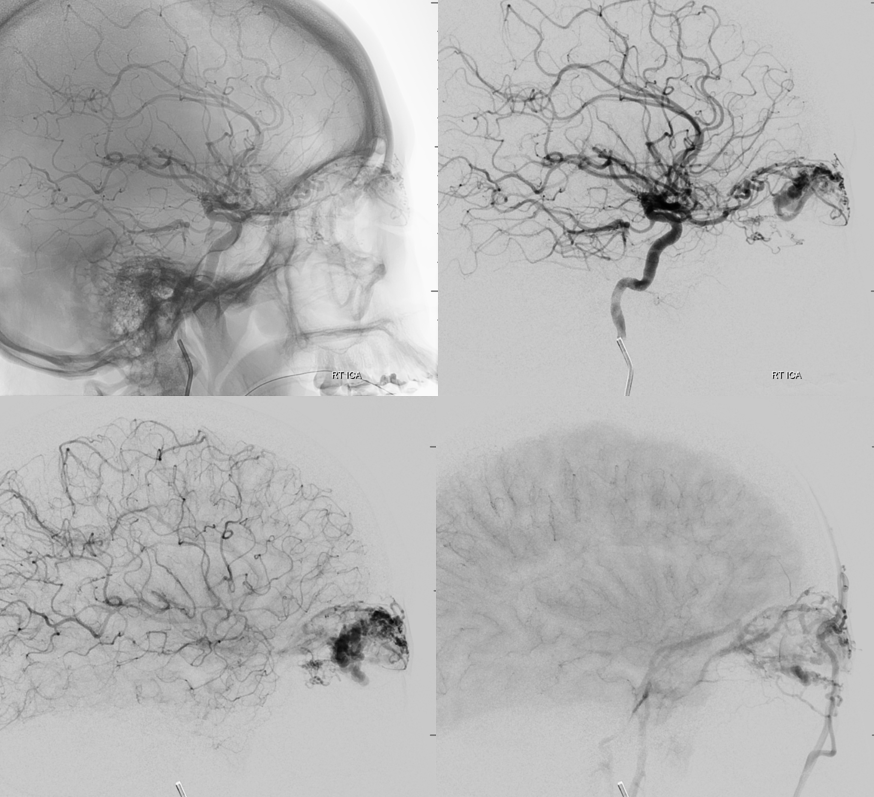
Stereos are very helpful when DYNAs are not an option
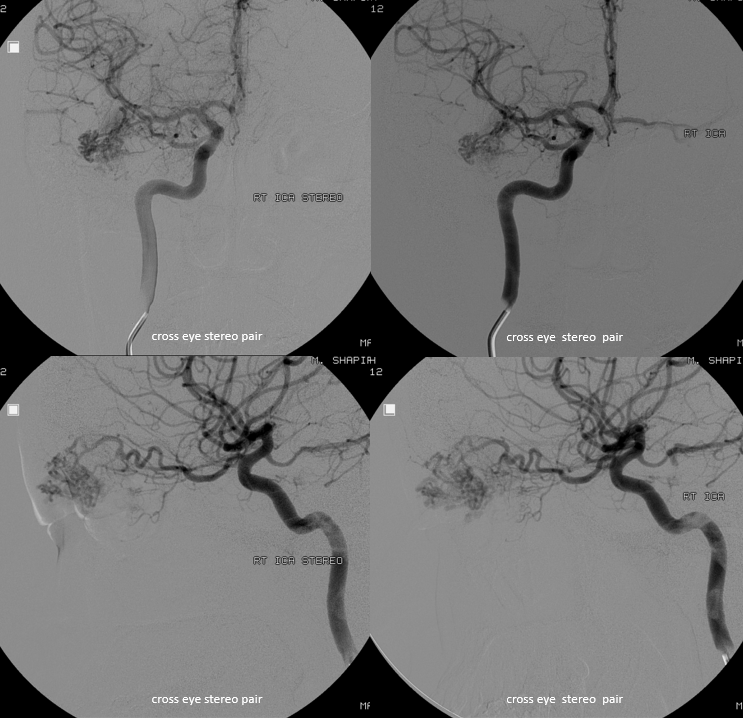
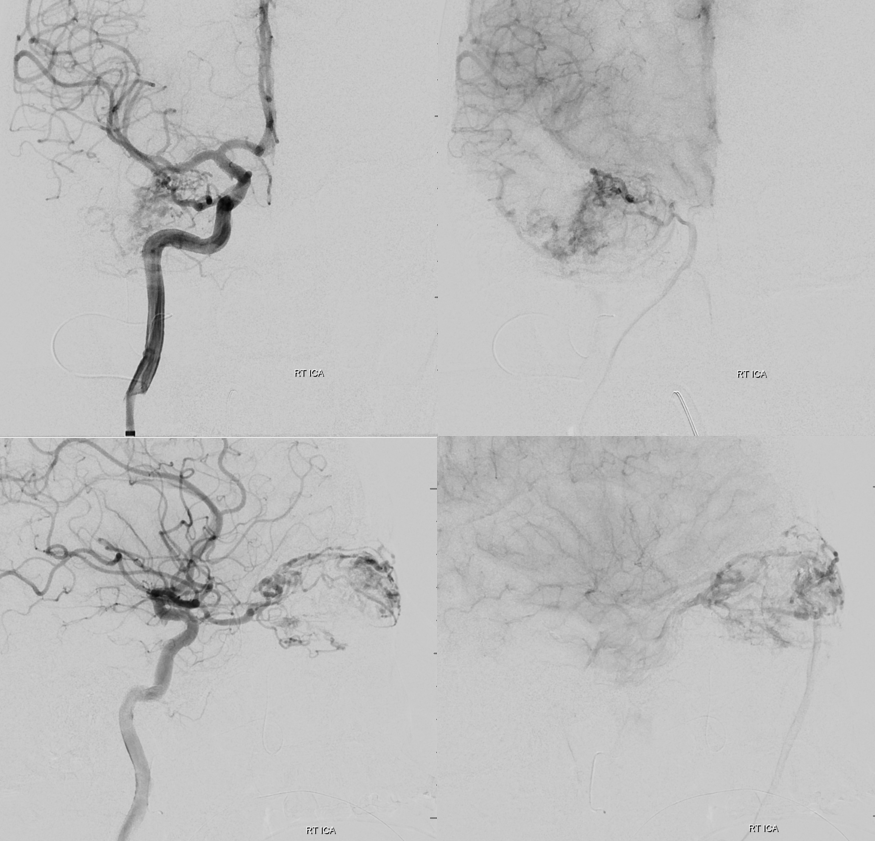
The reality is that DYNA is not necessary here. Basic ophthalmic artery anatomy is enough here. The AVM is lacrimal. Ophthalmic artery course is classic — ICA origin, crossing over the optic nerve. The ciliary and central retinal arteries will arise from that turn (ovals in image below). See Ophthalmic Artery page for extensive anatomical information.
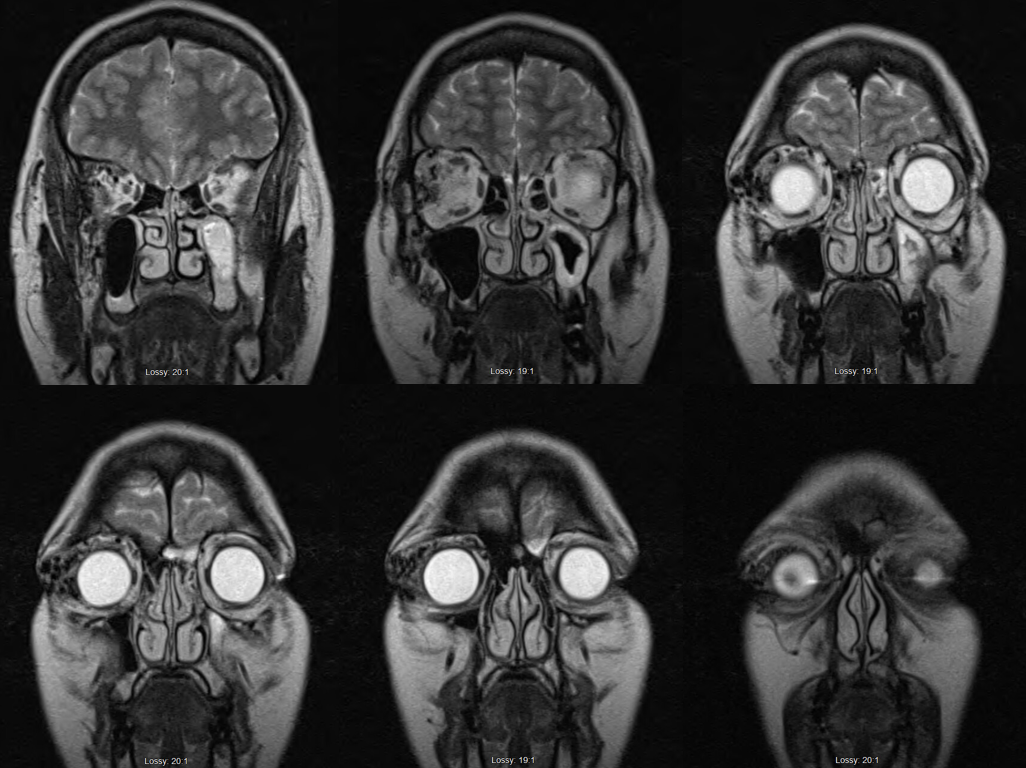
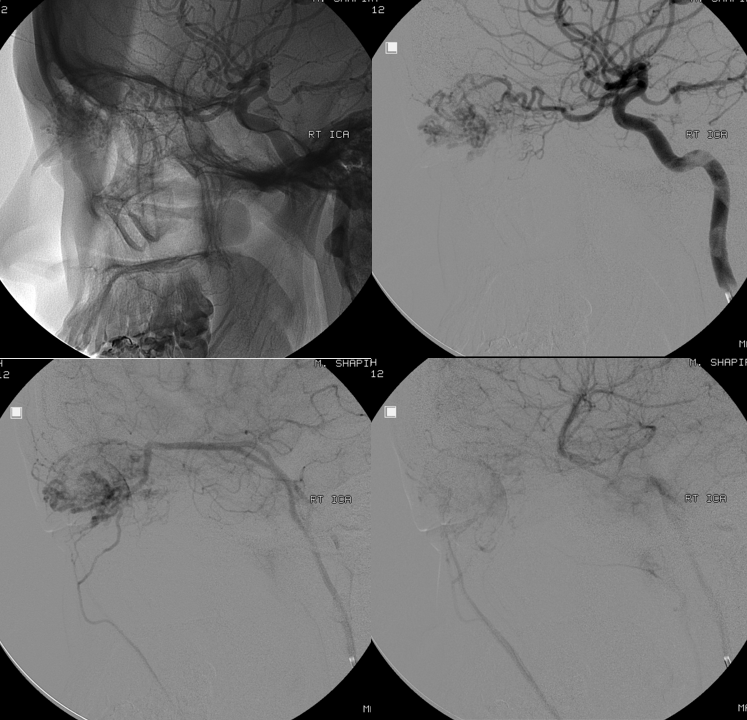
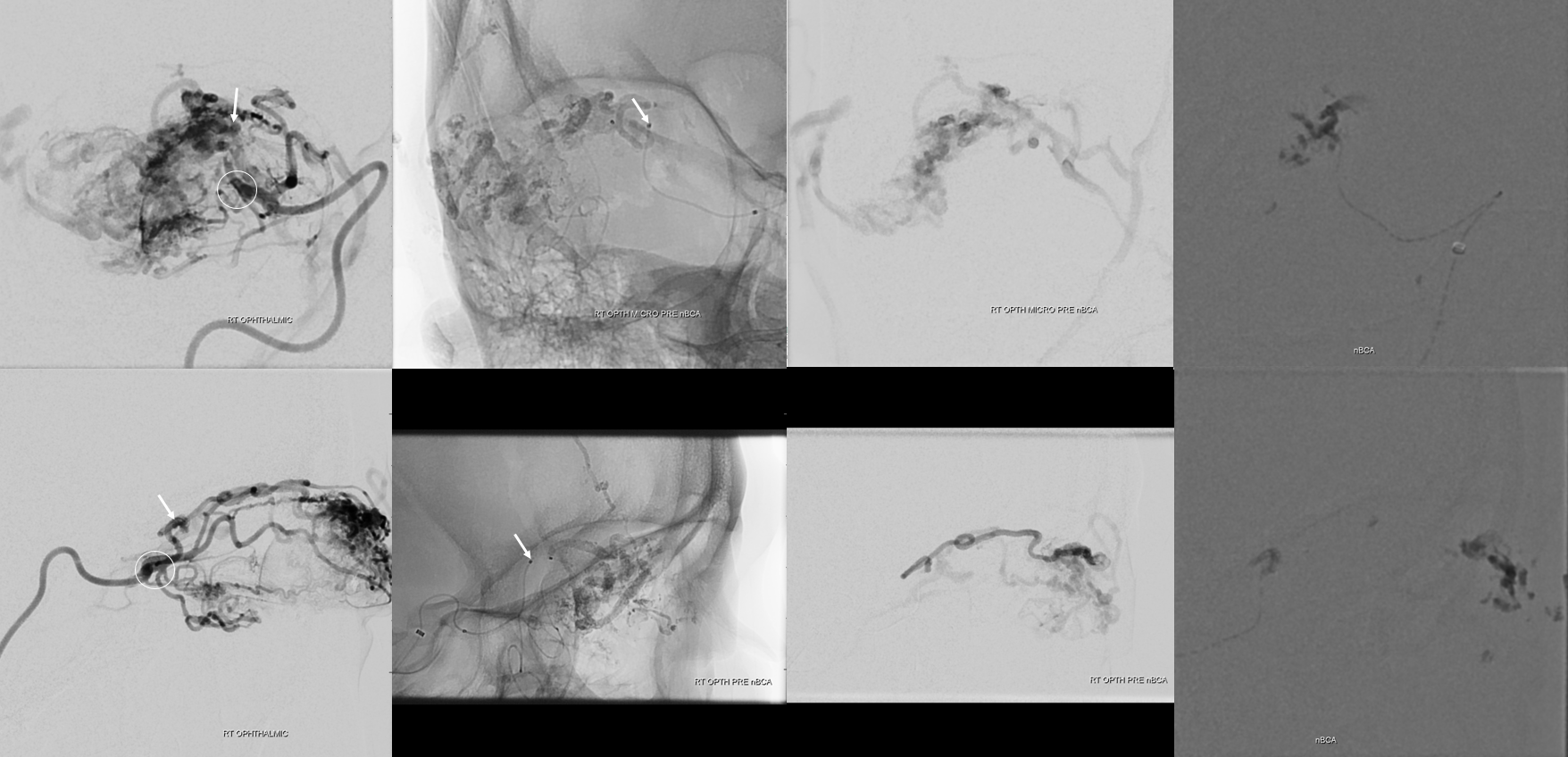
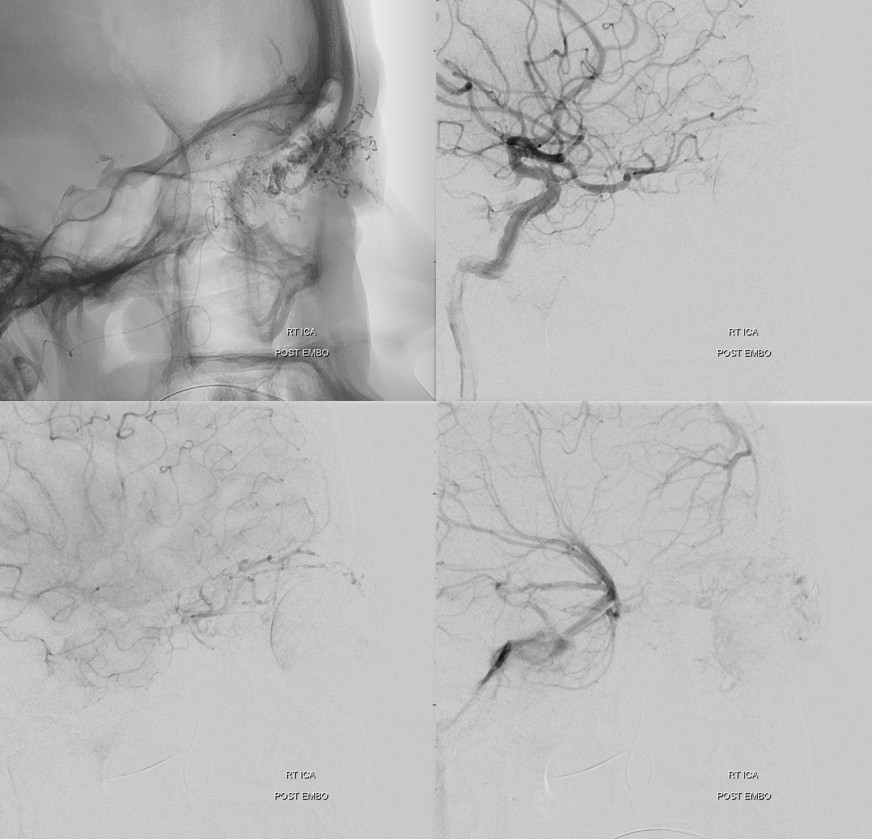
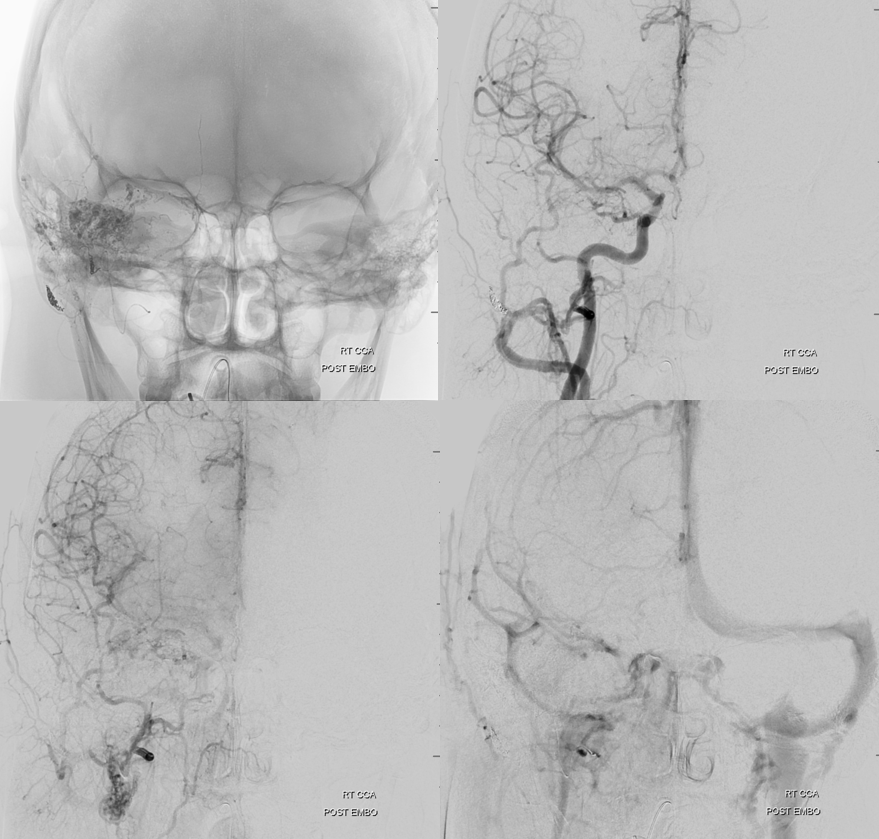
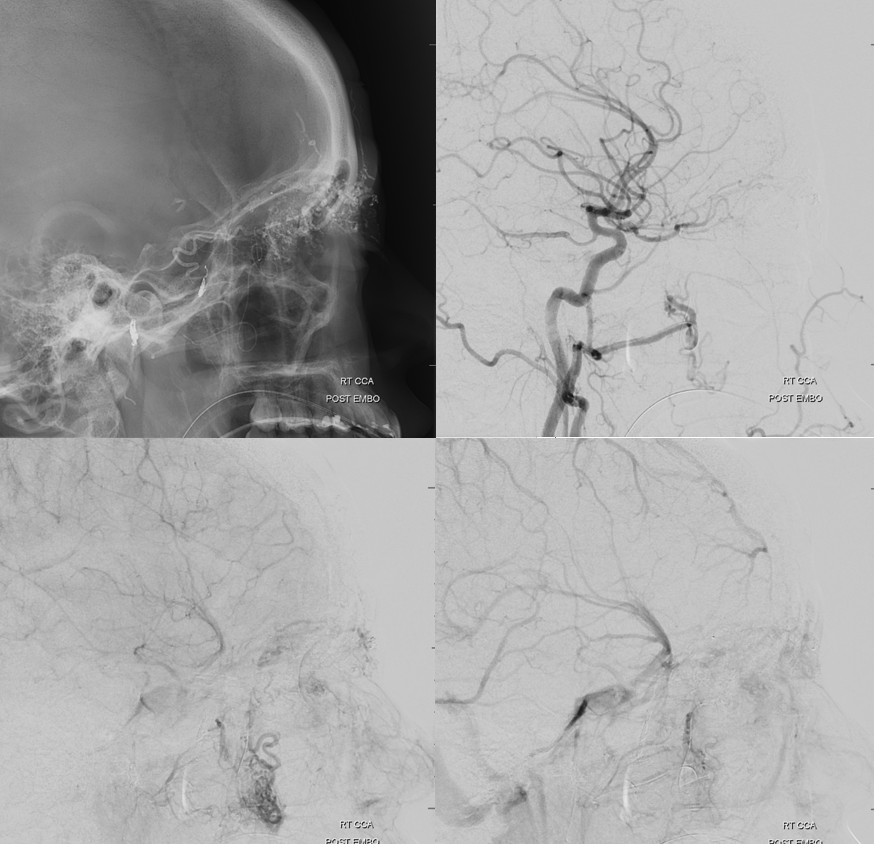
New machine arrives just in time for embolization — with much better images and much less radiation to the globe
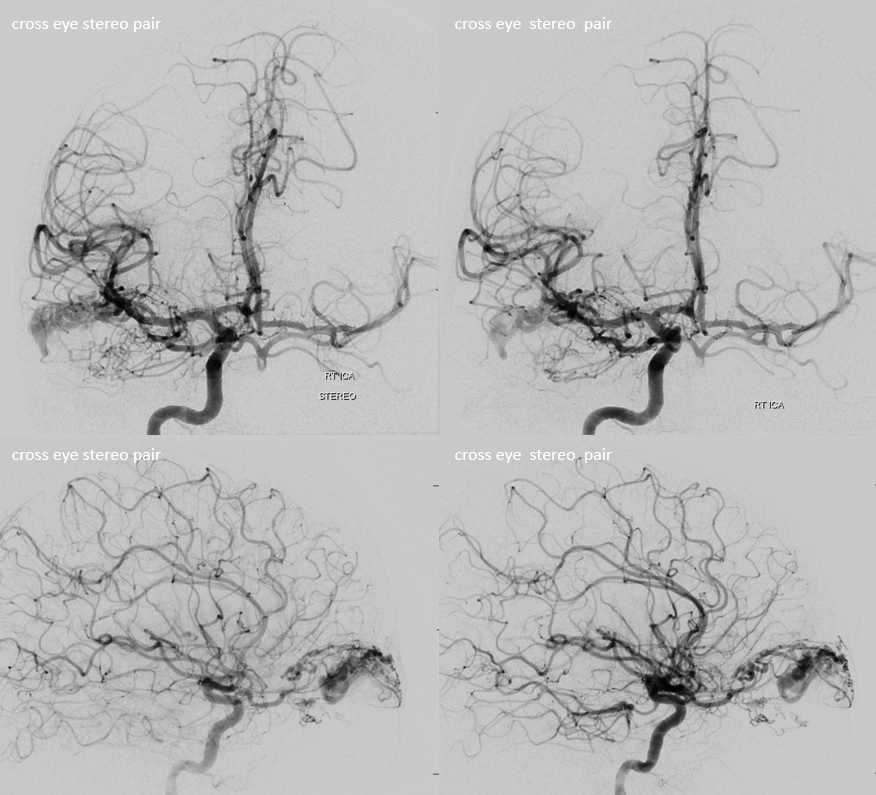
Its important to understand how exactly ECA contributes to AVM supply so as not to fall into a trap. Some of it will be direct — via infraorbital, superficial temporal, anterior deep temporal branches. Other will be indirect and thus treacherous — joining the ophthalmic artery proximally — embolizing these pedicles is the same as embolizing from a proximal ophthalmic position.
Start with the safer ones — whatever nidal penetration we get is gravy — but we didn’t get much.
These are cutaneous facial branches, with embolization position away from nidus. There is no role for Onyx here, in my opinion. The best option is nBCA
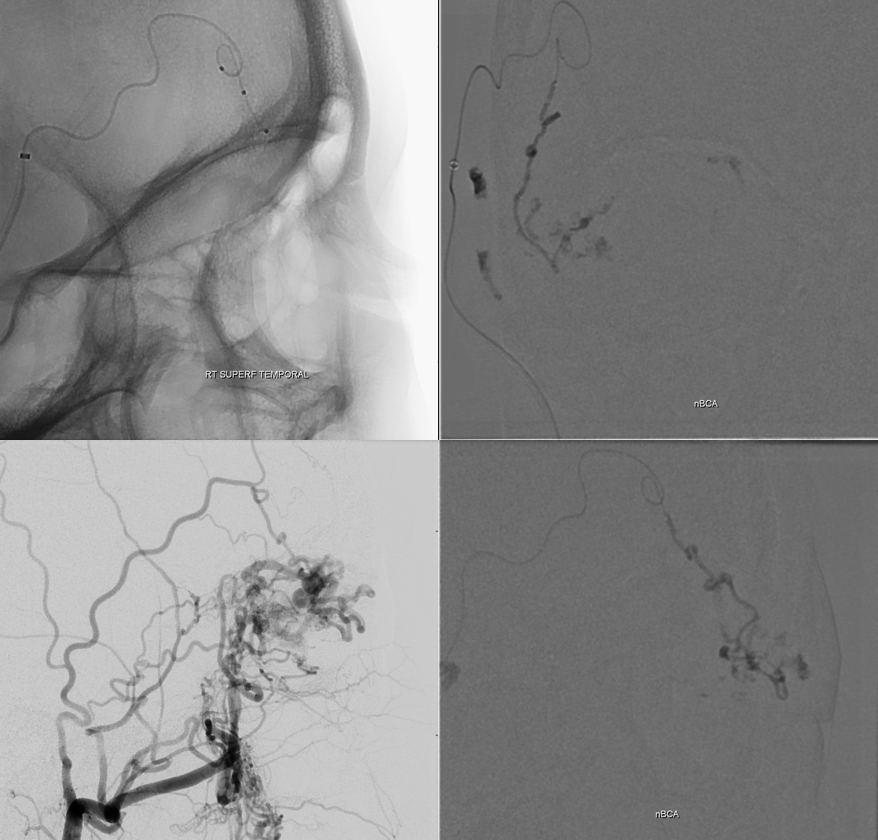
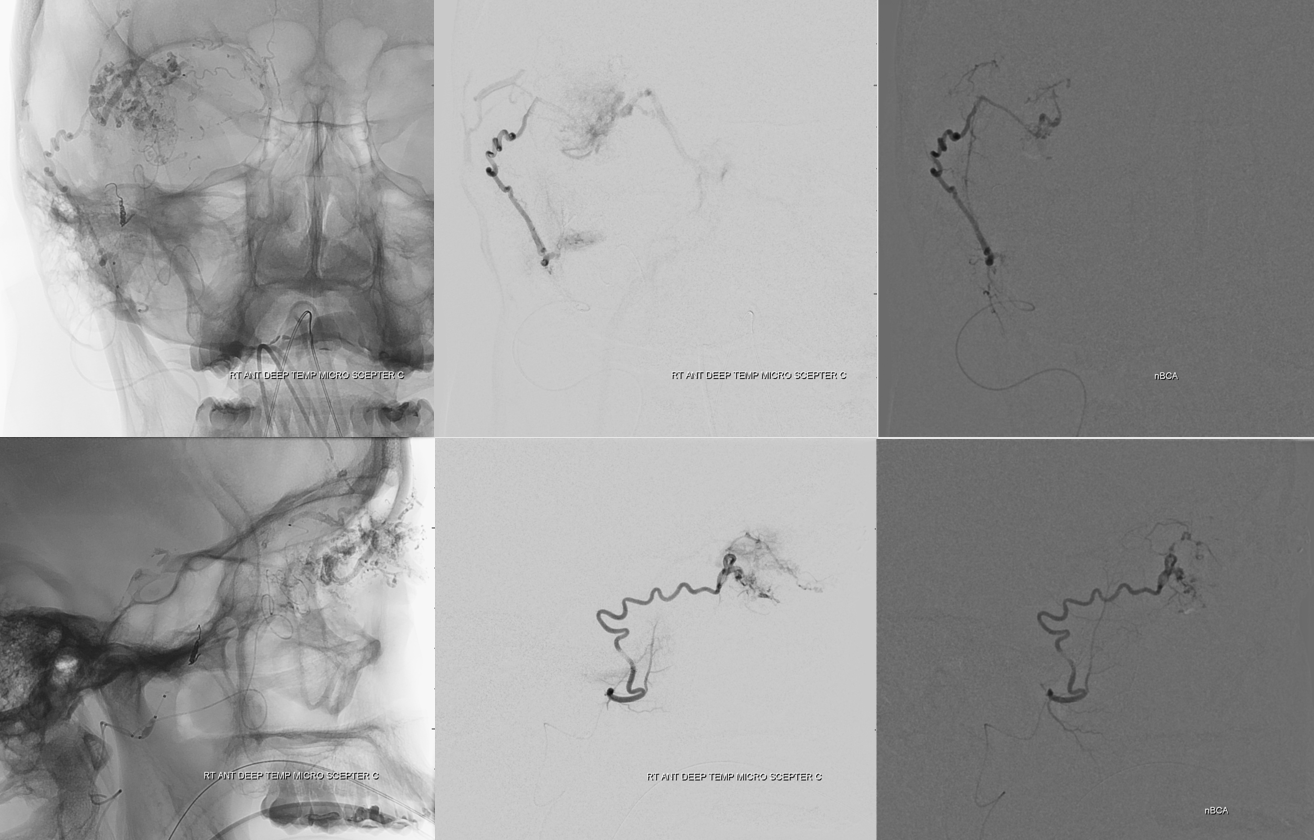
Look where the catheter tip is — deep in superolateral orbit, in the lacrimal branch — via an an indirect route (anastomosis with the infraorbital artery). This is the safest of options — we are quite distal from ciliary and retinal vessels, and not in the ophthalmic. The only thing to worry about here is reflux along the ophthalmic trunk. Got some good penetration here.
Another indirect position — in the ophthalmic artery itself — just at the top of the curve. Its more treacherous — see how the tip of the catheter is pointing posteriorly? Any reflux into the proximal ophthalmic will be a close call — so the nBCA injection is stopped as soon as cast forms in the main pedicle
Post stage 1
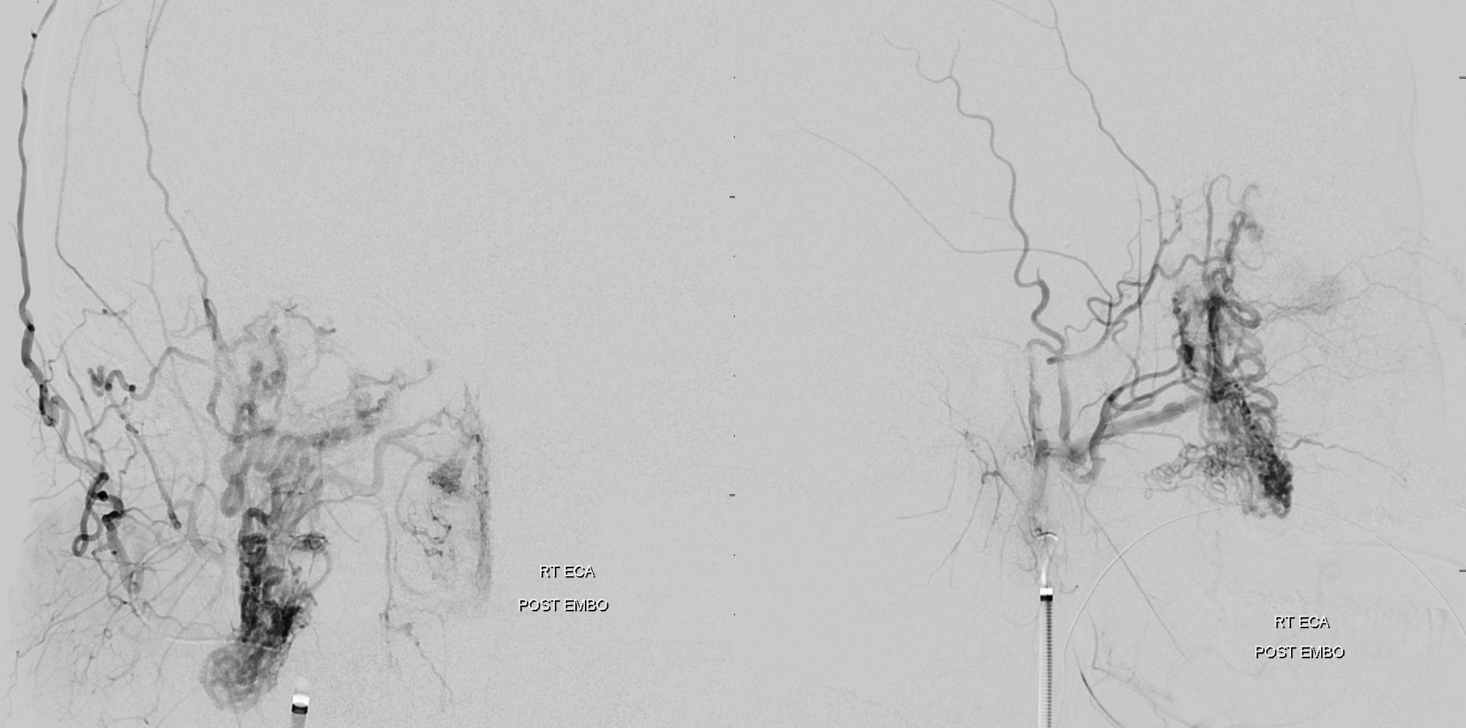
Look how much less there is to be seen from ICA also — all benefits of indirect embolization. But there is still plenty to go, and there will be no way of avoiding ophthalmic catheterization next time.
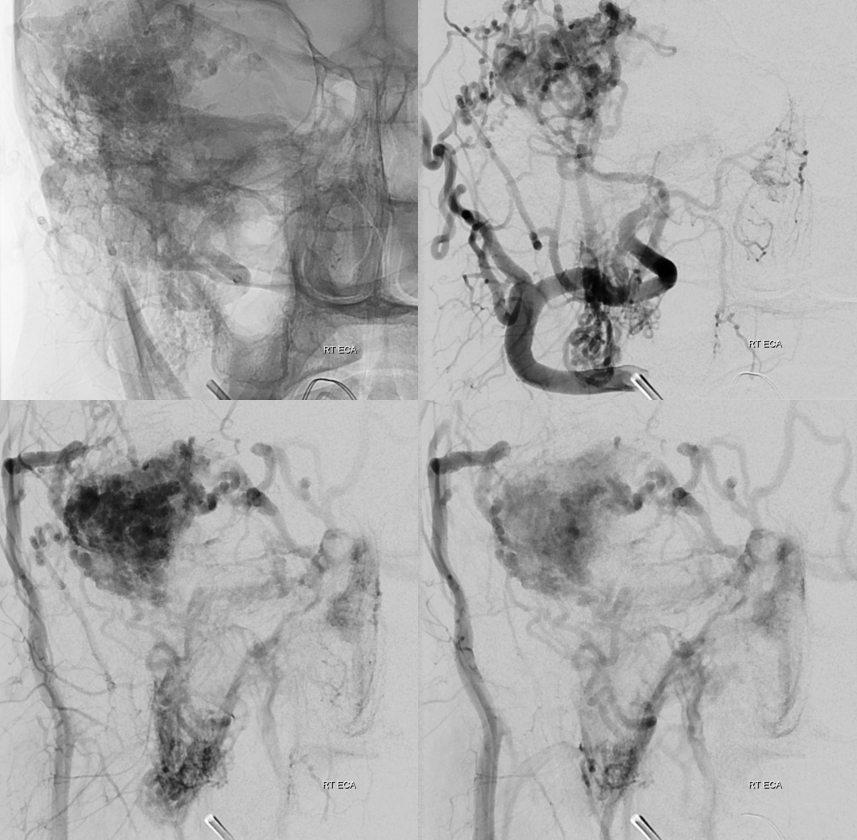
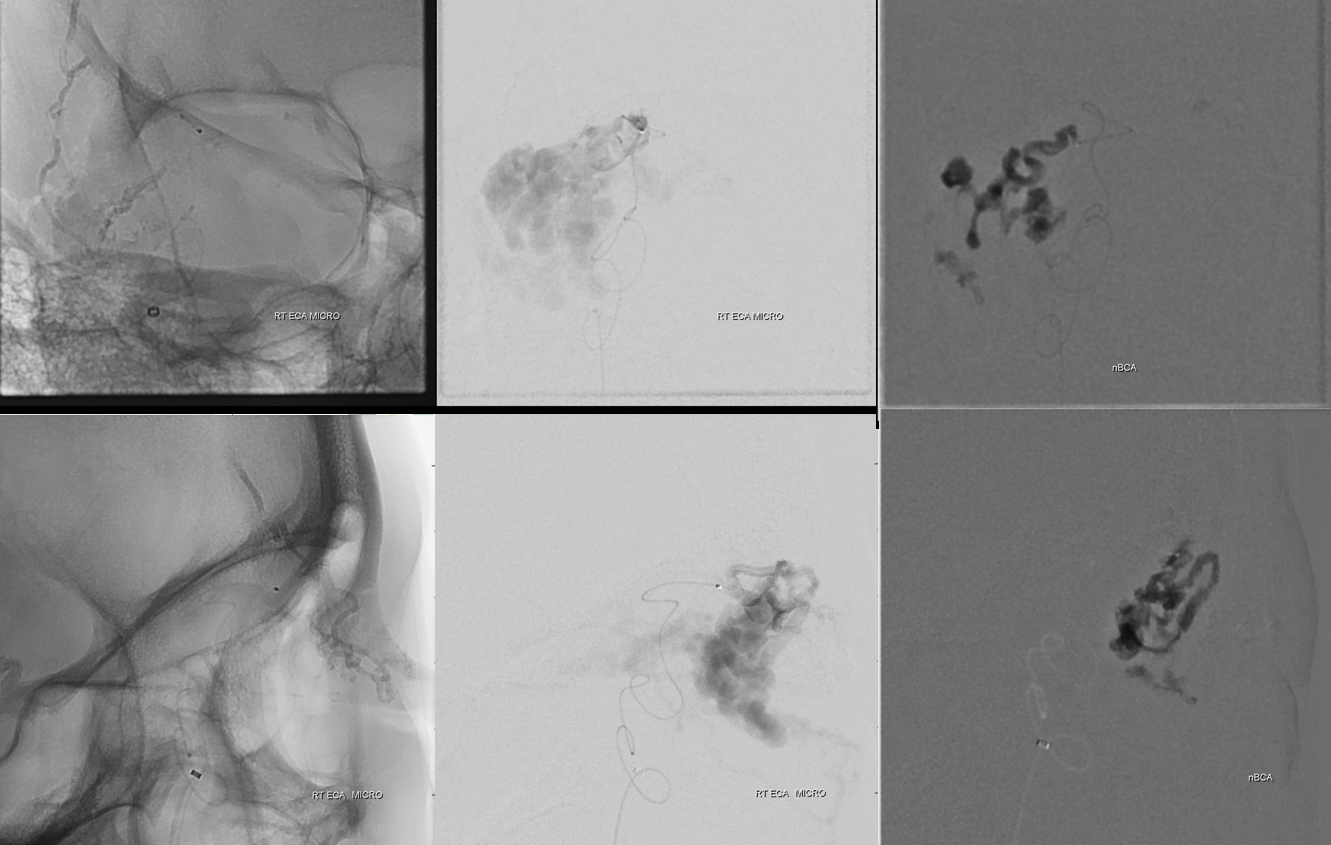
Stage 2 — more supply has been recruited from ECA over the 2 weeks in-between
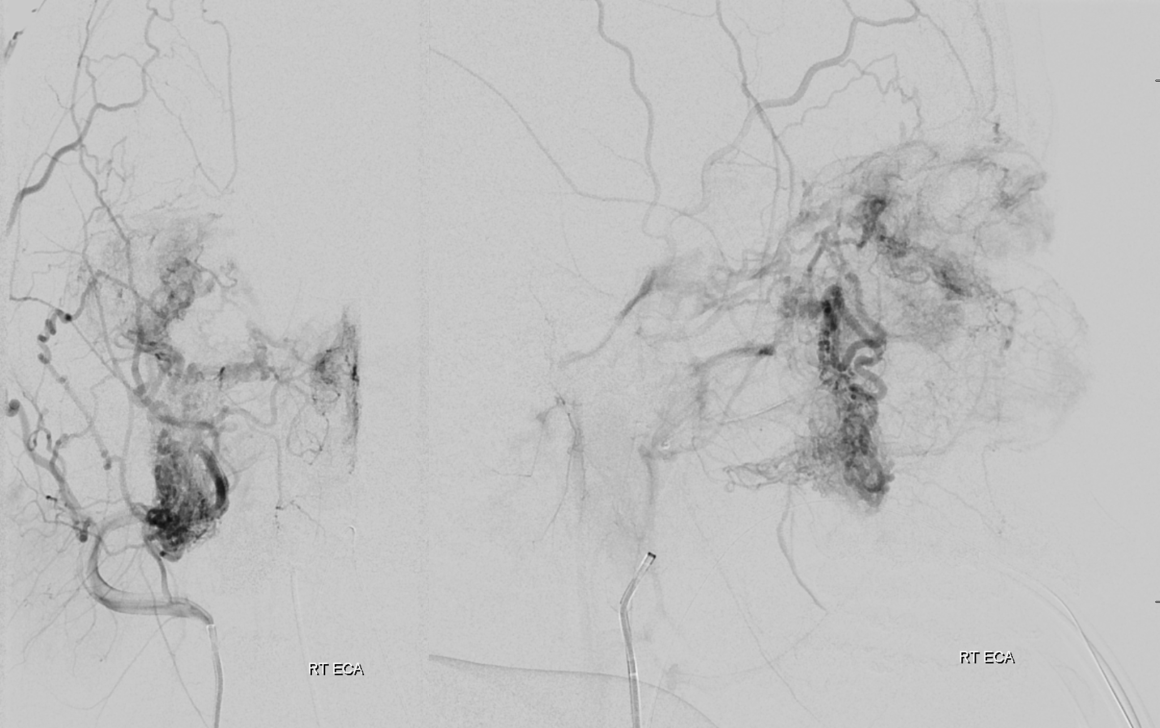
There is more also now from ophthalmic — mainly inferior stuff, at deep aspect of nidus
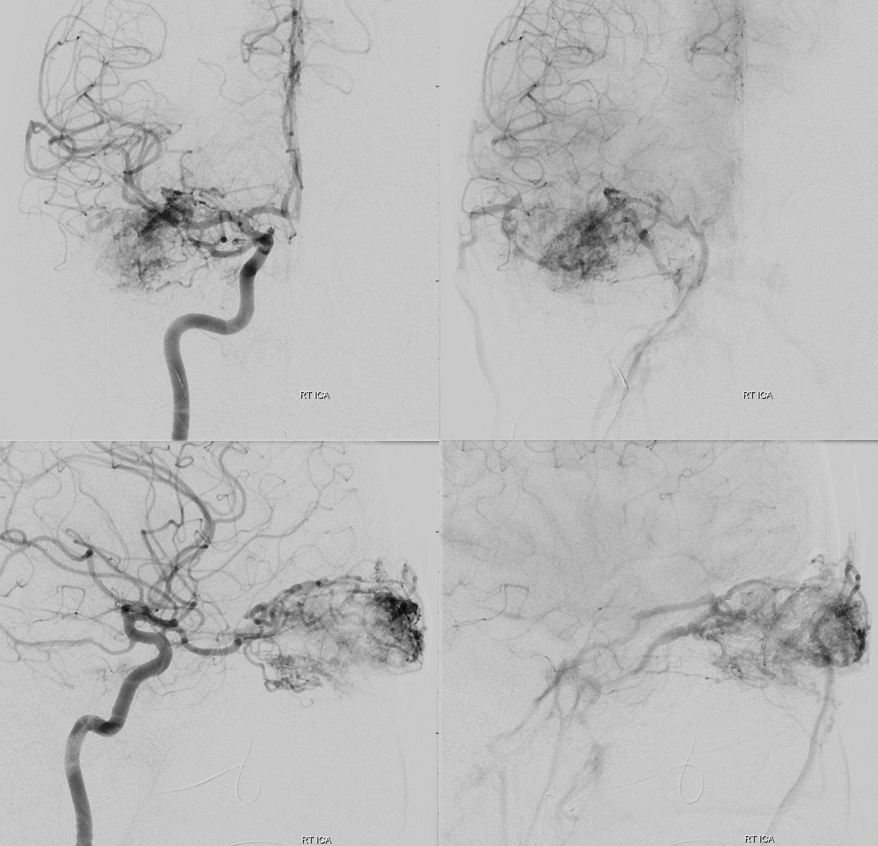
A Sofia 5 in the ophthalmic artery… No joke. Was hoping to have it there for stability and avoid re-catheterizing the ostium, but there was too much spasm so had to keep it in the cavernous segment.
Notice something else also — see anything strange?
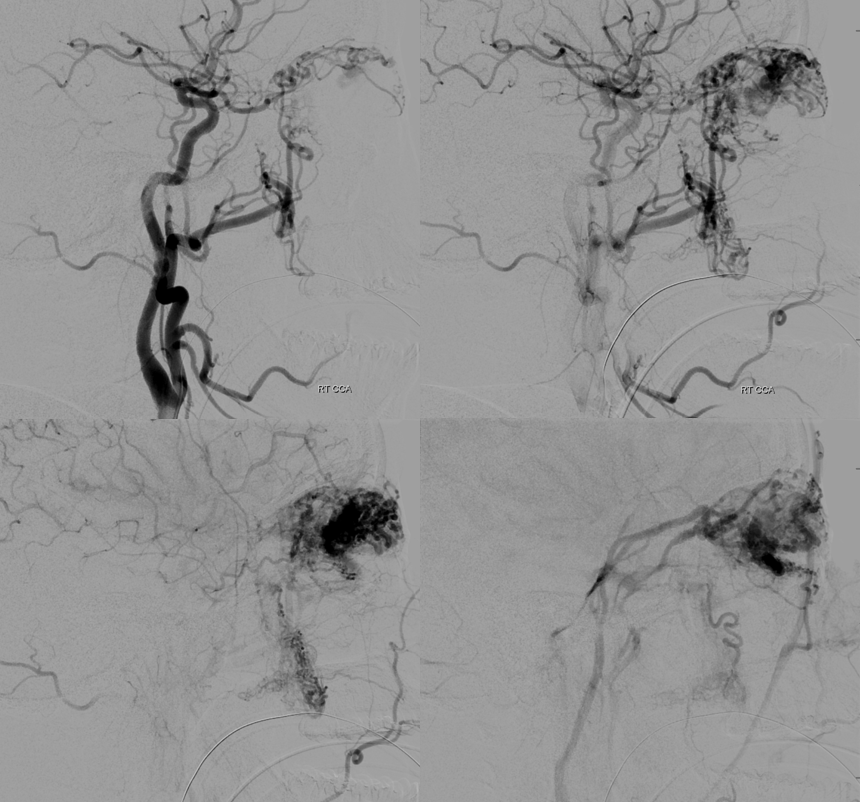
So, now we go into the ophthalmic. Nothing magical here — just careful catheterization, aspirating back on microcatheter to get bubbles out (yes, that’s completely safe — you wish you could suck clots out with a marathon or magic — nothing bad happens, only bubbles don’t go into the retinal artery).
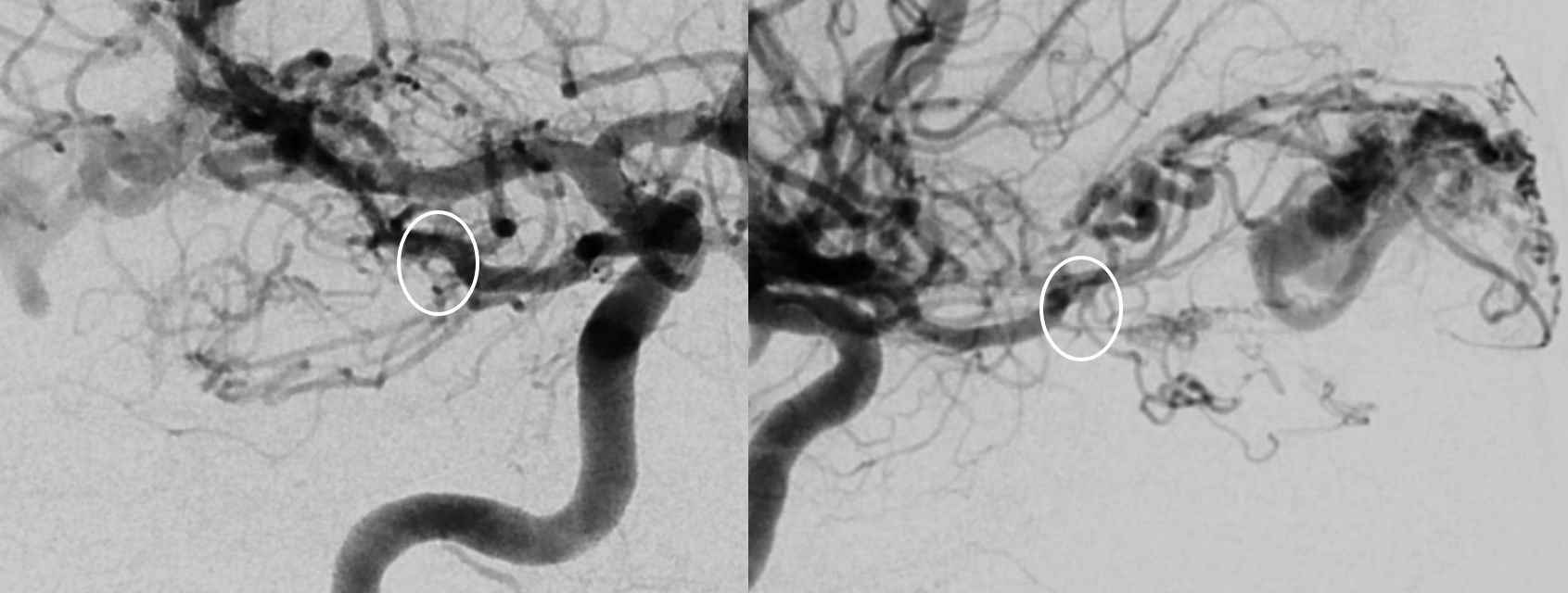
The tip of the catheter is shown by white arrows, and the reference images on left show which branch its in. The circles show the location of “angle” and thus where ciliary and central retinals come from. Images on right a glue cast. This is the safest of the branches — lacrimal family, at the top of the bend / angle, and so beyond the origins of globe vessels. Again, its nBCA, no role for Onyx here (cant have reflux, don’t want to “pull”, not enough safety for a detachable tip). The main consideration with nBCA is not to reflux. There is a small risk of glue breaking off during the nBCA pull — the less reflux, the less that happens, since there is no glue around the catheter. Much of this is technique, and anatomy also.
Next branch is actually medial — and very indirectly supplying the AVM via the superior and inferior palpebral branches (dashed arrows). Safe, but a long shot across the eyelids. Probably could have used the sandwich technique here, but didn’t. The little glue in the upper eyelid was ok actually.
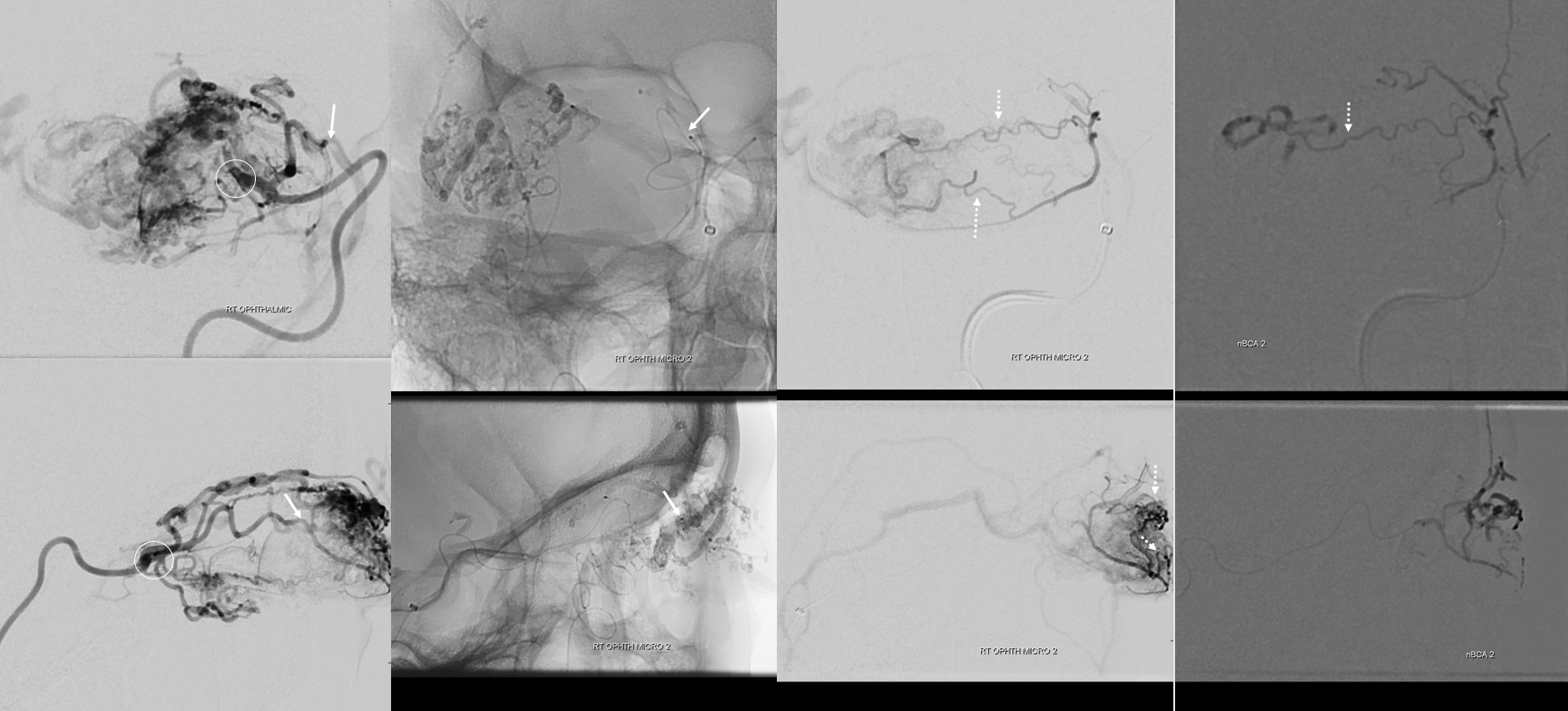
This shot is the most hazardous — the catheter is in the inferior rectus branch, barely engaged in it from the main ophthalmic trunk, and proximal to the “angle”. Any reflux here would end up in the ophthalmic. Not that this would blind the patient for sure, but certainly the risk is much higher. The technique here is to use dilute nBCA (3:1) — as in injections above also — and to inject relatively quickly, to push the glue into the nidus. As soon as the pedicle starts to fill, the injection is terminated, before more glue sets up in the proximal part of pedicle and starts to reflux. In none of these situations did we have “flow arrest” — its all about dilute glue and reflux avoidance.
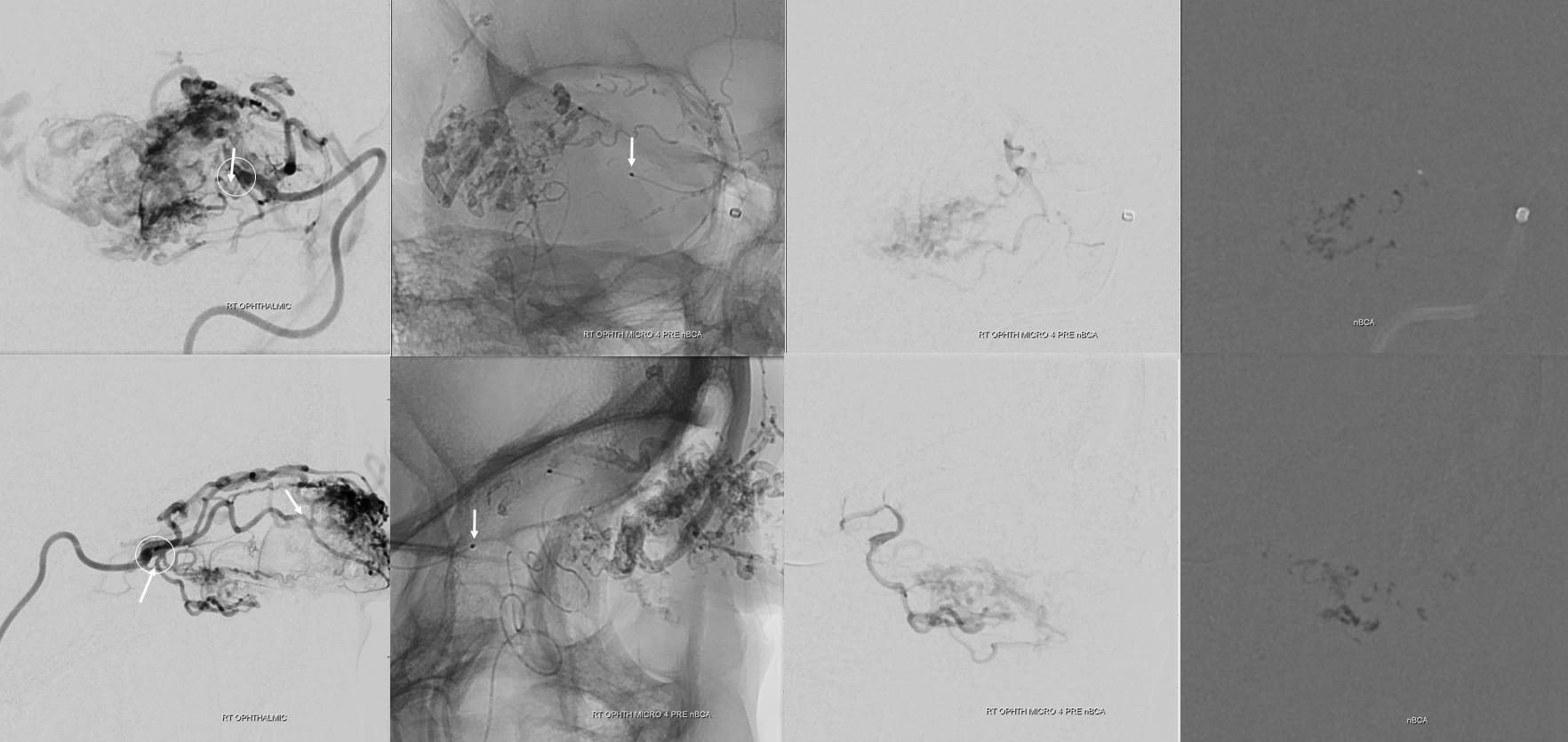
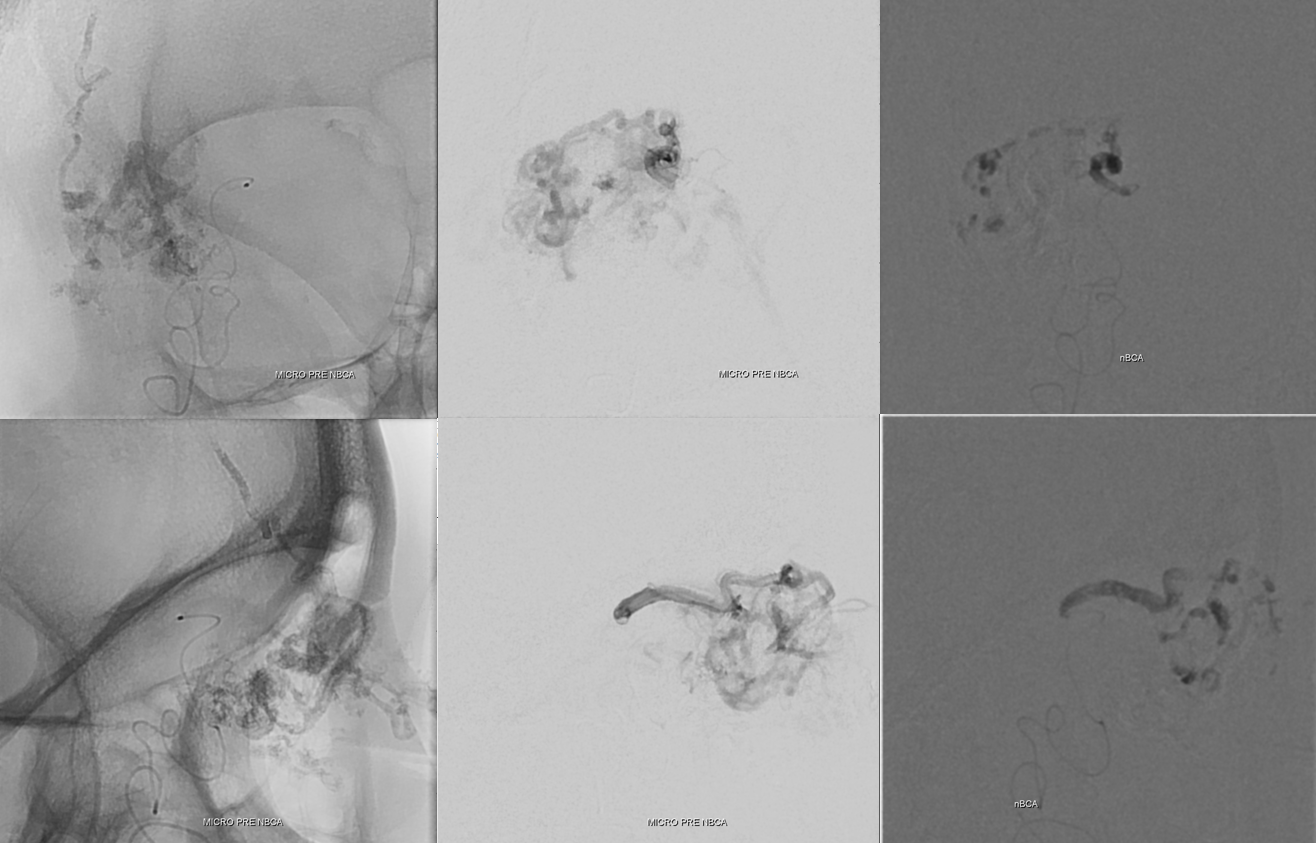
Post ICA
ECA — there is minimal supply remaining. We glued more from the anterior deep temporal
Minimal residual, through a very curious arterial network of the distal IMAX. We weren’t really sure what to make of it. There is no shunt, and it would be strange to have such an extensive collateral network relatively far away from the AVM. Remains a mystery, and may be a kind of “pure arterial malformation”.
We shut down the remaining supply to the avm (ovals) with particles — because the pedicles supplying the AVM were cutaneous and unrelated to the ophthalmic system. But it is a risk — particles go anywhere flow does, and if we miscalculated, the central retinal artery is about 220 microns in diameter — a single particle can take out the whole thing.
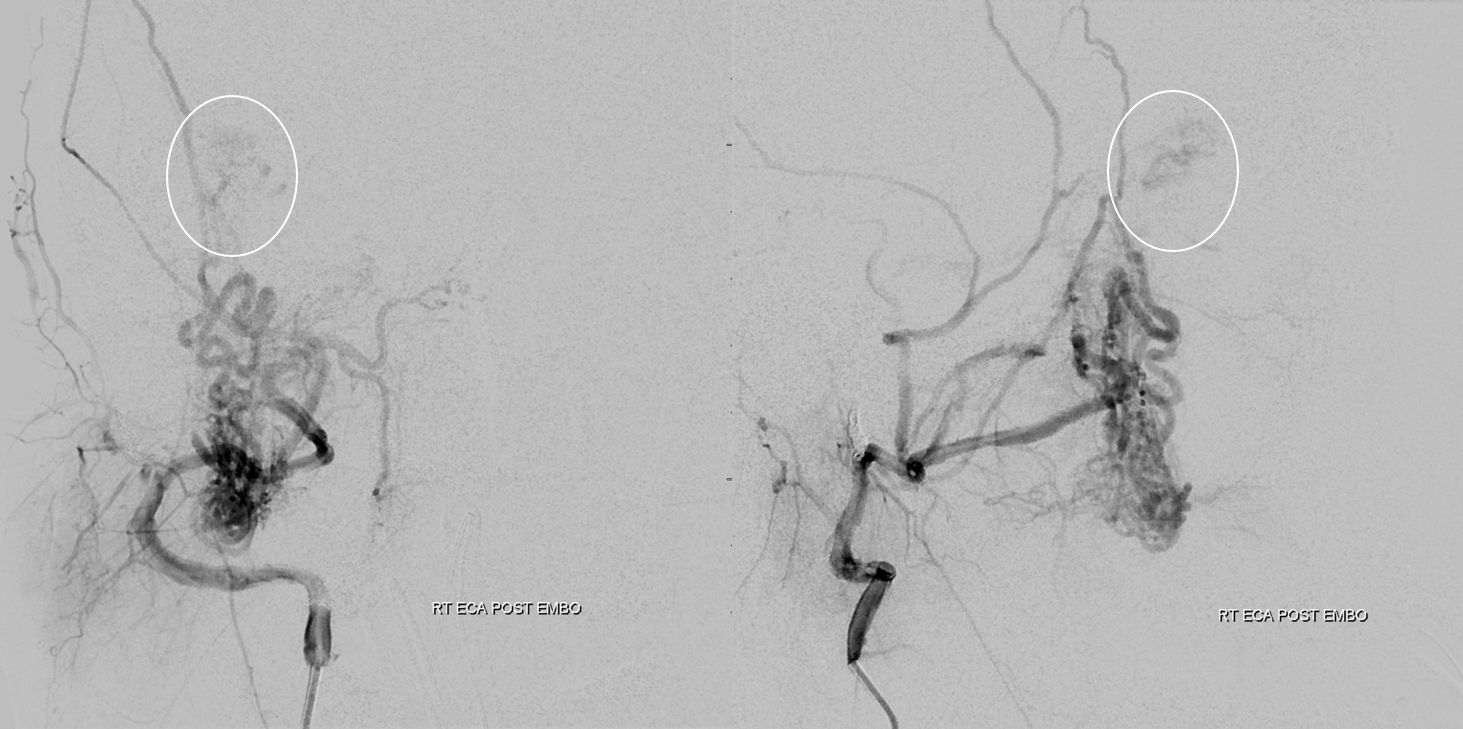
Final common injection. Its dry. Notice anything curious? (remember question above)
Operative pictures — there are many more that we can show outside of this setting. It was a dry field. The arrow points to the tip of retained catheter which is the curious thing above. The rest of the catheter was pulled out also. It was retained at the end of first embolization stage. Very rare these days to end up with that — this one broke during the pull. And just like in the old days — retained catheters are overwhelmingly safe. Trying to remove them is usually not. This was in the external, so completely benign.

Delayed MRI/A post resection. Apart from needing moisturizing eye drops (the lacrimal gland is part of the specimen) the patient is completely normal.
See Ophthalmic Artery page for more, including links to other trans-ophthalmic interventions.
