In collaboration with Donato Pacione, MD
The classical teaching holds that isolated spinal epidural hematomas are venous hemorrhages, and no angiographic investigation is warranted. This is certainly true in the majority of cases, especially when supported by typical history of an elderly individual on various anticoagulation / antiplatelet medications — most often Warfarin. However, one must always be cognizant of exceptions to every rule. This young person presented with 1 week of new and severe upper thoracic neck pain, followed by sensory / proprioceptive deficits in the lower extremities. Motor and bowel/bladder functions were intact.
MRI of the thoracic spine: There is a heterogeneous dorsal (posterior) epidural mass (white arrows), with a hypointense internal line (black arrows) that suggests compartmentalization / presence of internal heterogeneity, with cord compression. Notice multiple enlarged vascular channels in the adjacent paraspinal musculature (purple). The collection is more prominent on the left (yellow)
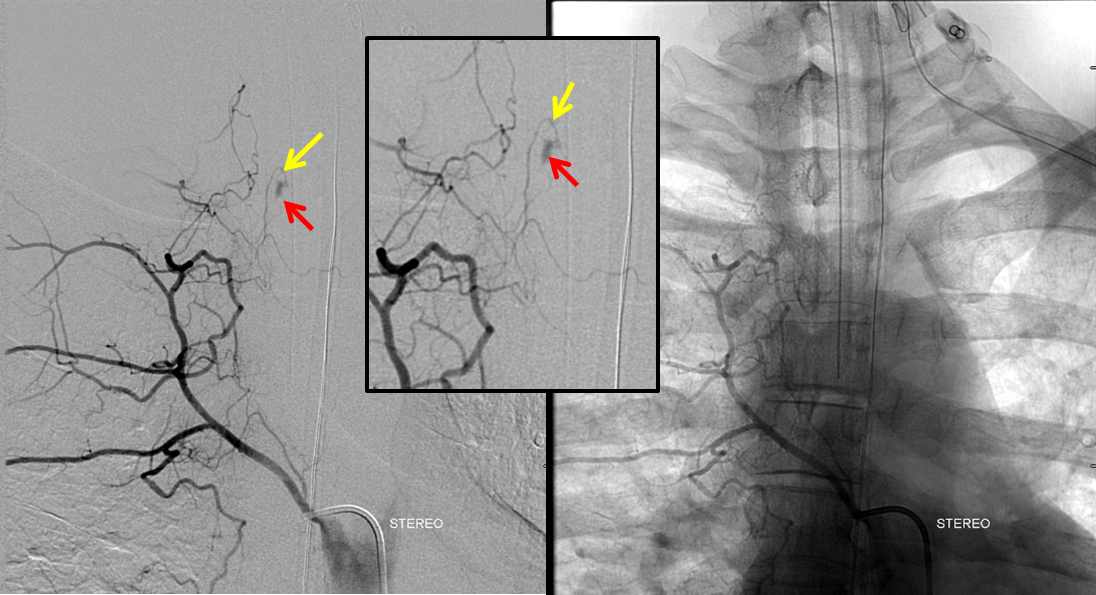
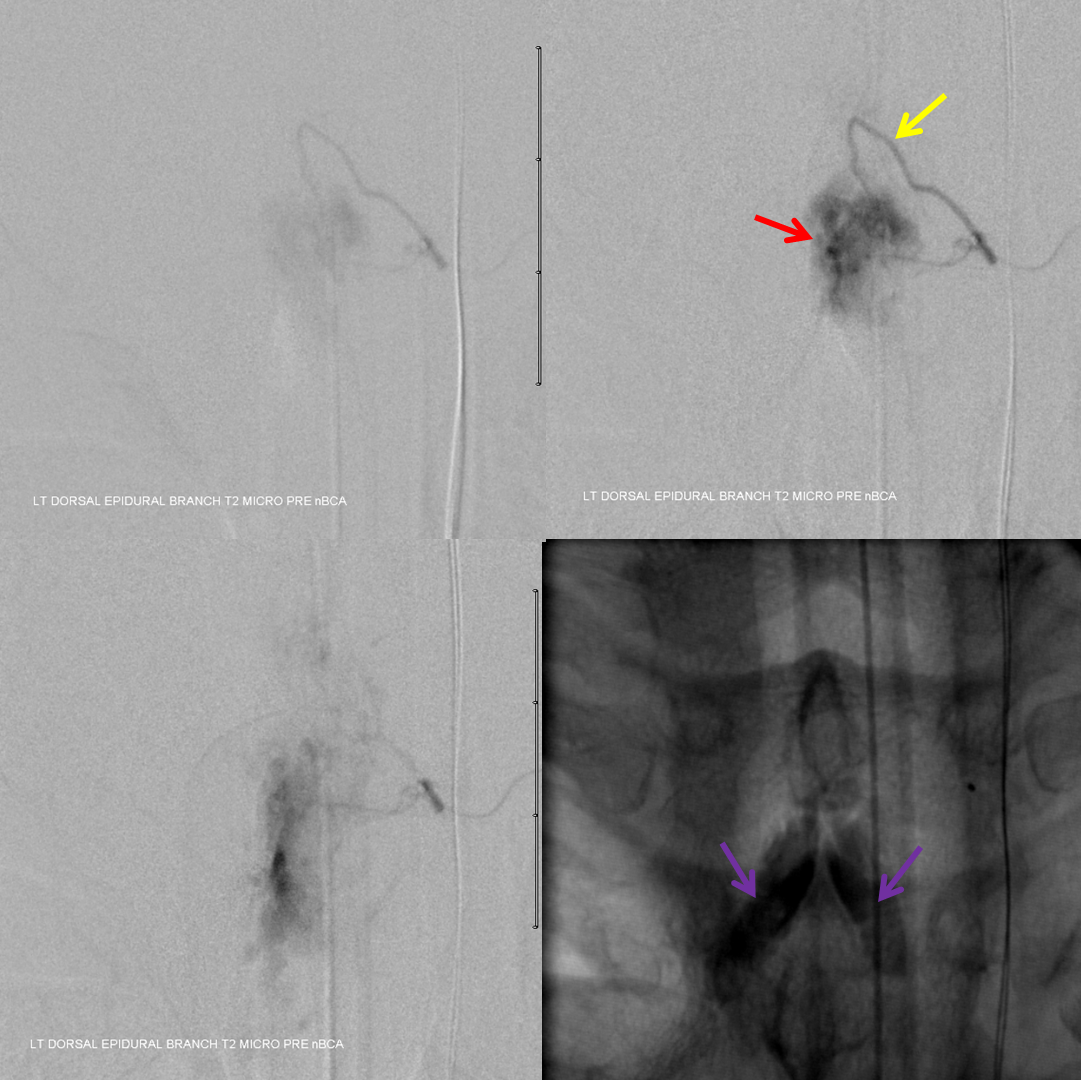
Arch injection demonstrates contrast collecting over the upper thoracic midline (red) in late arterial phase, washed out by the venous phase.
Spinal angiography demonstrates multiple routes of supply to the same posterior epidural arcade of upper thoracic area, delineating rich collateral networks. Right supreme intercostal injection, with dorsal epidural (yellow) branch supplying the malformation (red)
The longitudinal homolog of supreme intercostal is the costocervical trunk, from which the same AVM is seen, in STEREO, looking from the back
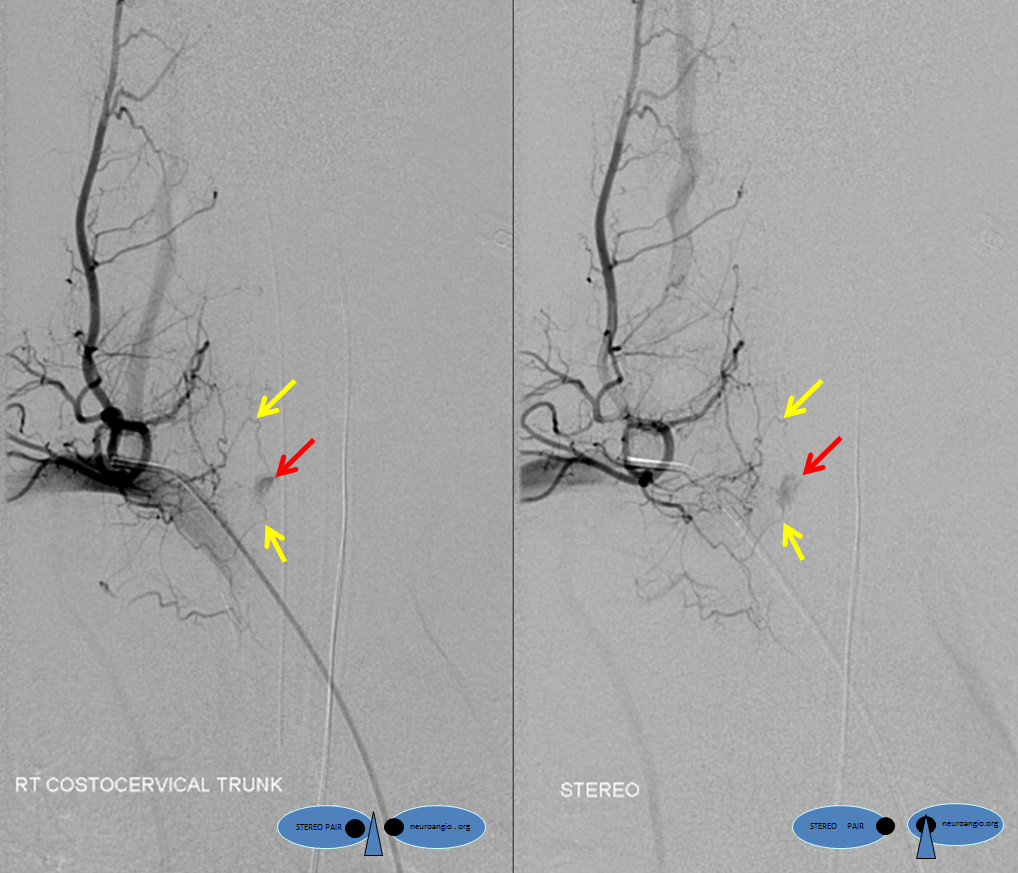
Next up is the left costocervical trunk, in stereo. Notice how dominant supply to the AVM corresponds with preponderance of hemorrhage in the left posterior epidural compartment on the MRI. The multilevel epidural arcade is beautifully displayed (yellow arrows). Notice minimal view (dot) of the right costocervical trunk through the upper right T2 level epidural branch (not labeled)
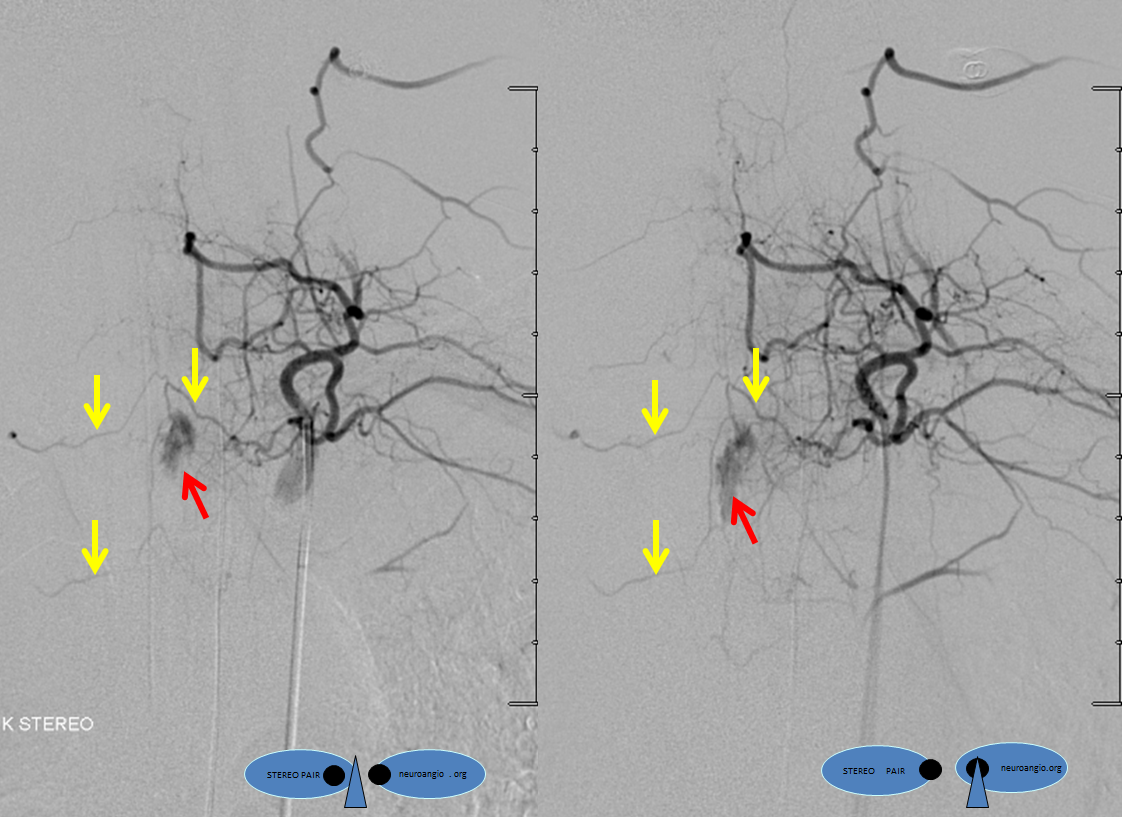
Selective diagnostic catheterization of the dominant pedicle shows a sequence of AVM opacification. Notice contrast collecting in venous phase in a plexus on both sides of the T3 spinous process (purple arrows) — corresponding to the MRI
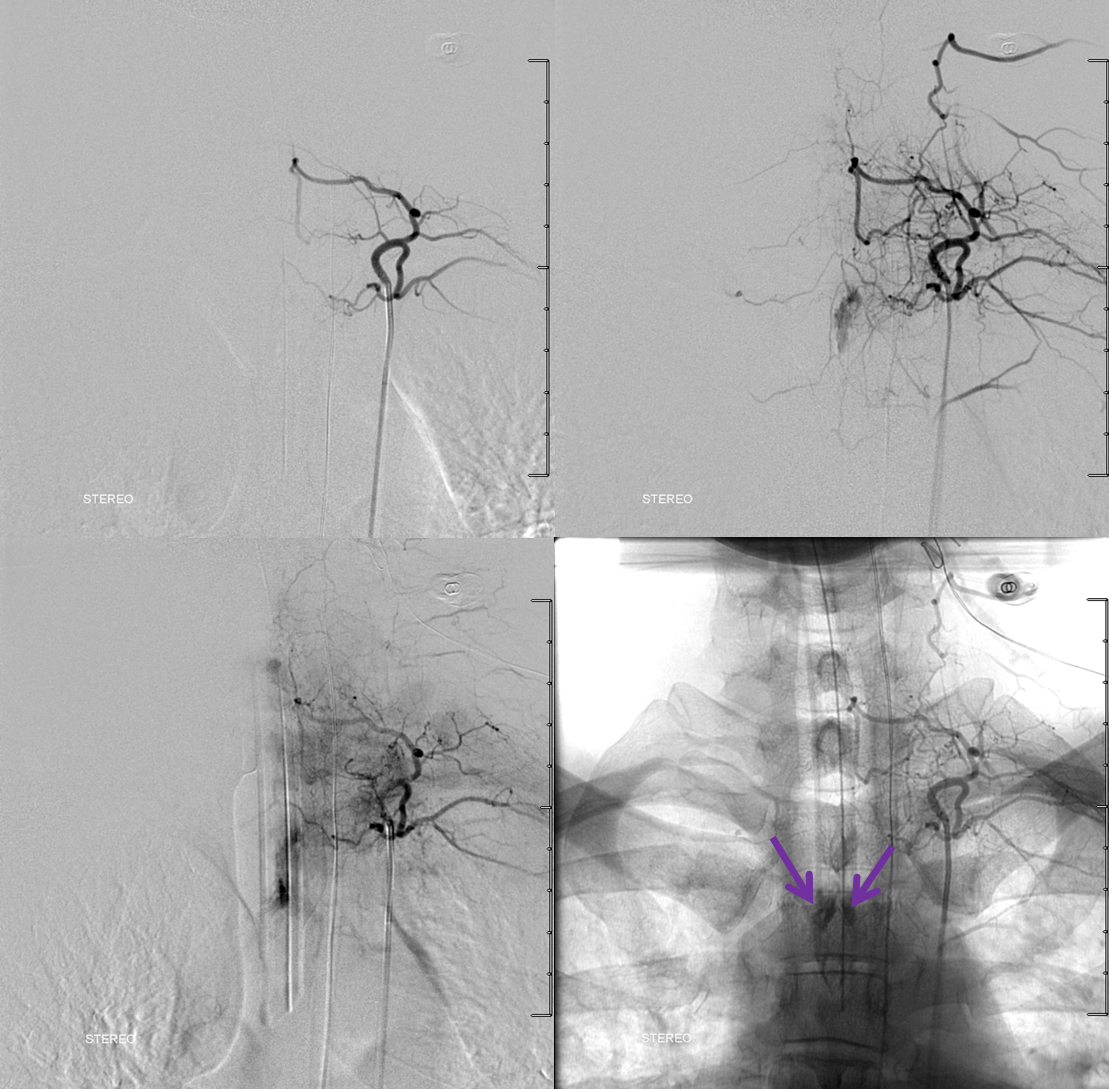
Subselective Marathon catheterization of the right T2 epidural branch, the dominant feeder, in a flow arrest (wedge) position demonsrates AVM microanatomy.
nBCA is the embolic material of choice. Complete penetration of the nidus is achieved, with reflux into regional epidural network to seal off collaterals.
Control post-embolization angiography must always be done from potential collateral vessels to assure the shunt is closed. Injections of the right costocervical trunk and bilateral supreme intercostal arteries show no residual
Post-embolization CT scan shows glue in the left dorsal epidural space (yellow) and stagnant contrast in the paraspinal venous network (purple)
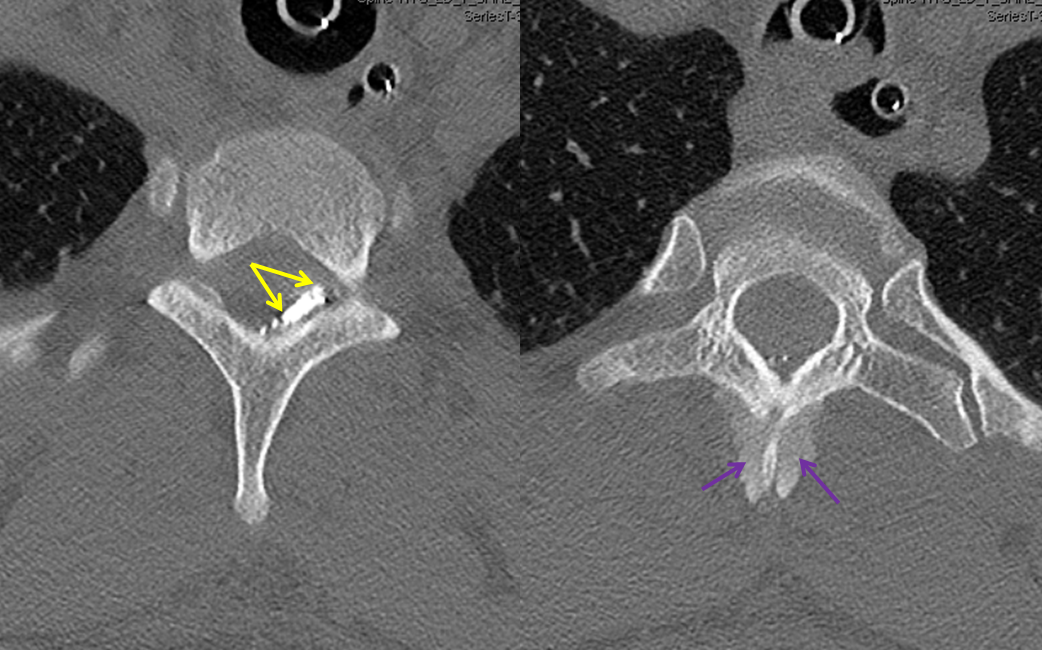
Check out this !STEREO MOVIE! of pre-op imaging and non-stereo nBCA injection. Notice on the micro run how much larger the AVM is than the epidural space, extending to the paraspinal muscular space where prominent vascular channels were first seen on the MRI. The nBCA injection only penetrates the epidural space. A “glob” of glue during the injection is likely the rupture point, now filled with nBCA. According to Prof. Willinsky (see article below), one must be careful of mass effect from nBCA in the epidural space.
Patient is taken to OR immediately after embolization for planned decompression (post-procedure neurologic exam was at baseline). Clinical outcome is excellent.
Related Article: http://www.ajnr.org/content/24/9/1901.full
Back to Case Archives
