This key part of the venous system connects the superficial / cortical veins and the subependymal / periventricular veins of the deep venous system. Thus, the white matter drains into both superficial and deep venous systems. These veins have been well-studied ex vivo, but not so well in vivo because of their small size. Thankfully, high field susceptibility-weighted MR imaging and DYNA/flat panel CT angiographic methods are offering more in-vivo insights.
Bottom line is that, like everything, this system is in balance. Part drains superficial, part deep. In some people, one dominates over other. Excellent background material is found in Surgical Neuroangiography of Lasjaunias, Berenstein, and Ter Brugge — Charles Raybaud contributed very heavily to the venous chapter. The key contributions of Yun Peng Huang and Okudera, among others, in angiogrpahic study of this system, have been known worldwide at the time (60-80s) but are now being forgotten — so dont forget! See in particular the many slides Dr. Yun Peng Huang donated to neuroangio.org — link above. Especially telling is lack of recognition of Huang’s pioneering work in understanding how medullary veins relate to what became known as the Developmental Venous Anomaly.
The basic idea is that subcortical white matter drains superficially, and deep white matter drains deep. There have always been postulated trans-cerebral veins which link the two systems. They definitely exist in a macroscopic state in the spinal cord. They also come into very macroscopic existence in the brain if there is some kind of chronic drainage problem (like venous congestion due to dural fistula). However, in nonpathologic states they seem pretty small and far between on angio — certainly not 300 microns, more like 30 maybe. Variation is the rule — some of us have more of them, others less. More seems better…
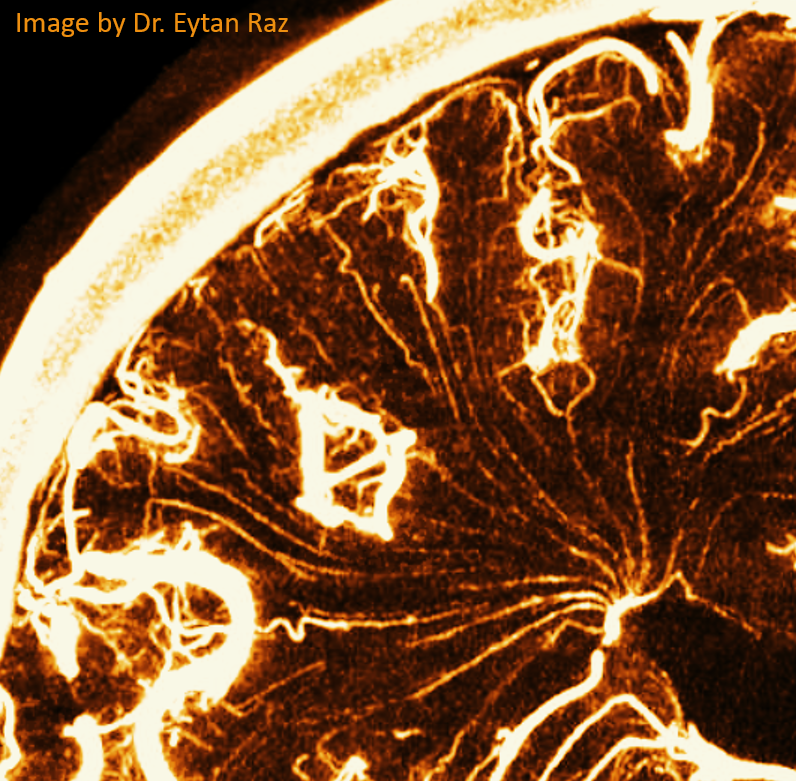
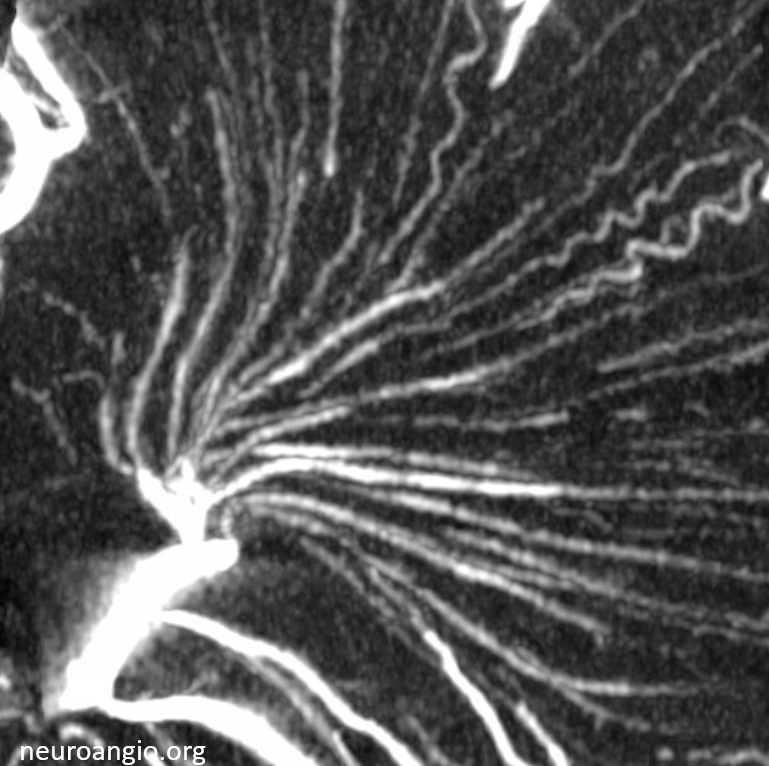
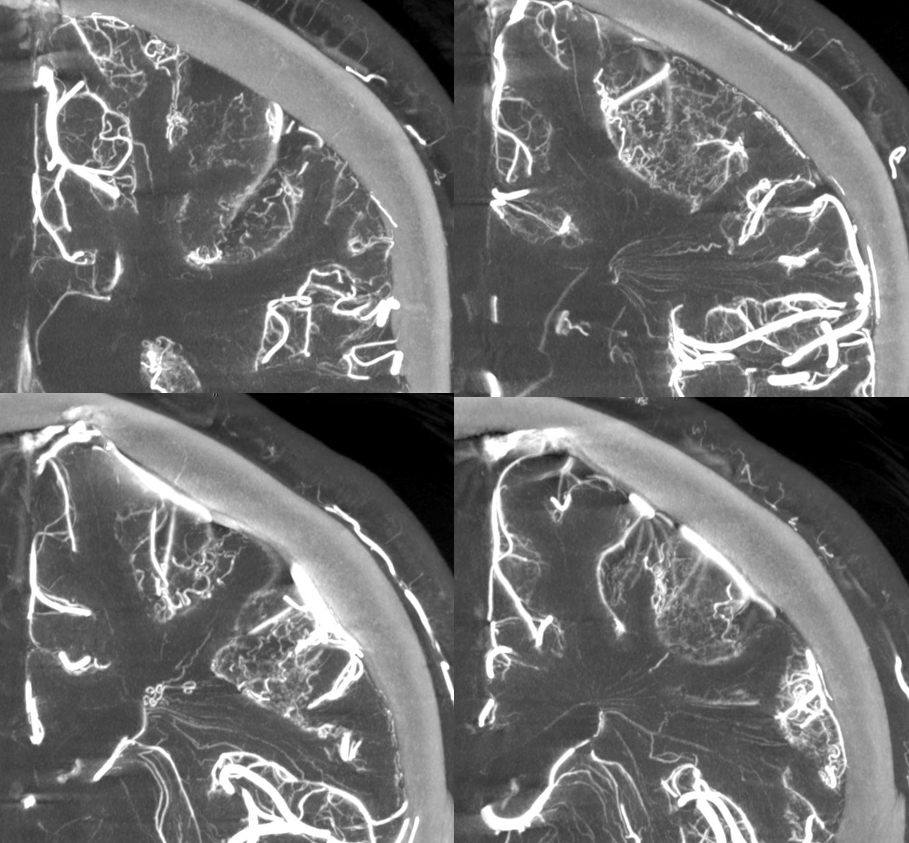
This person below seems to have lots of transmedullary veins — and meningitis…
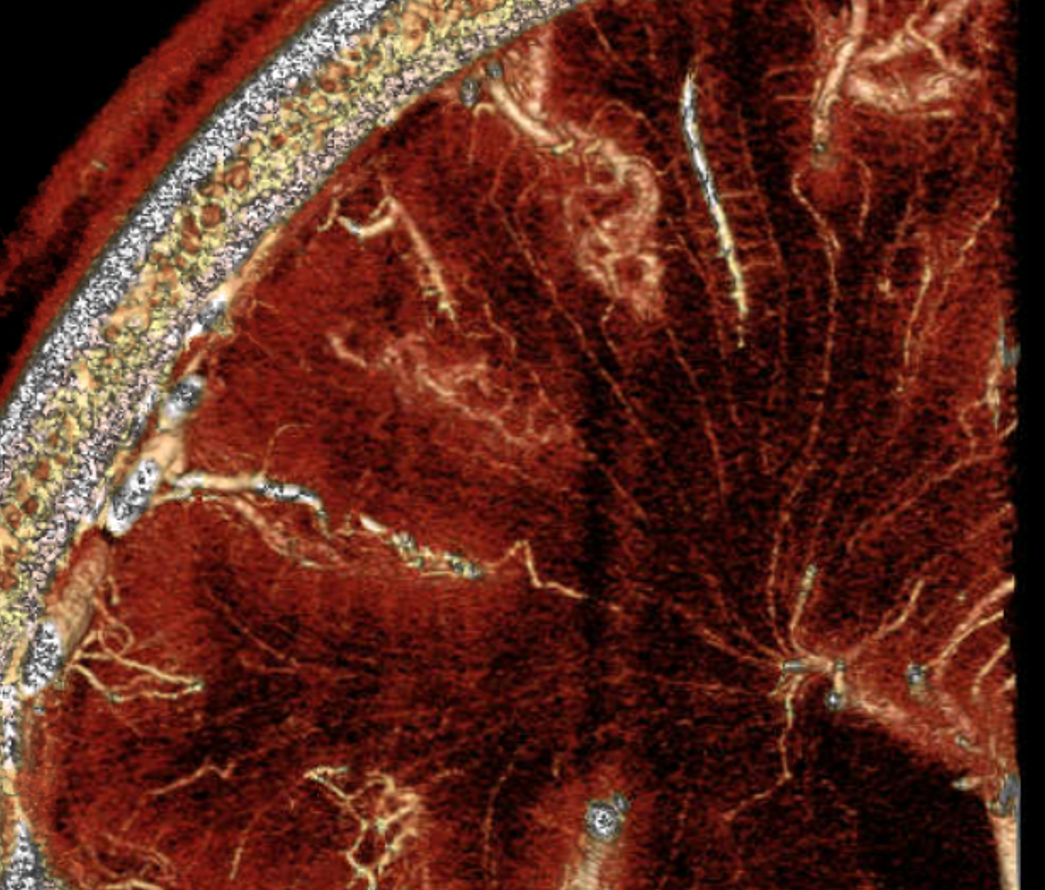
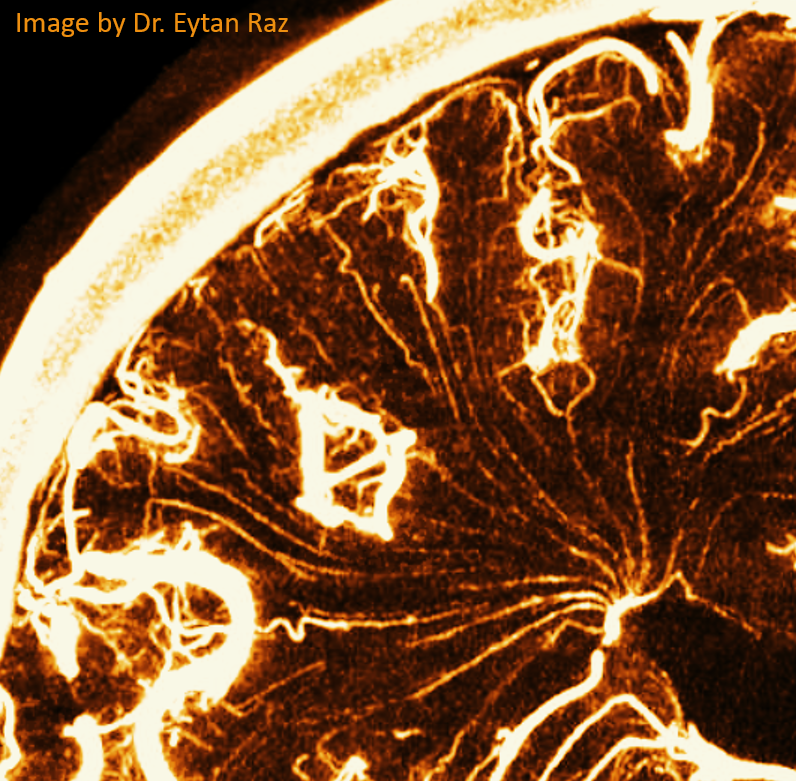
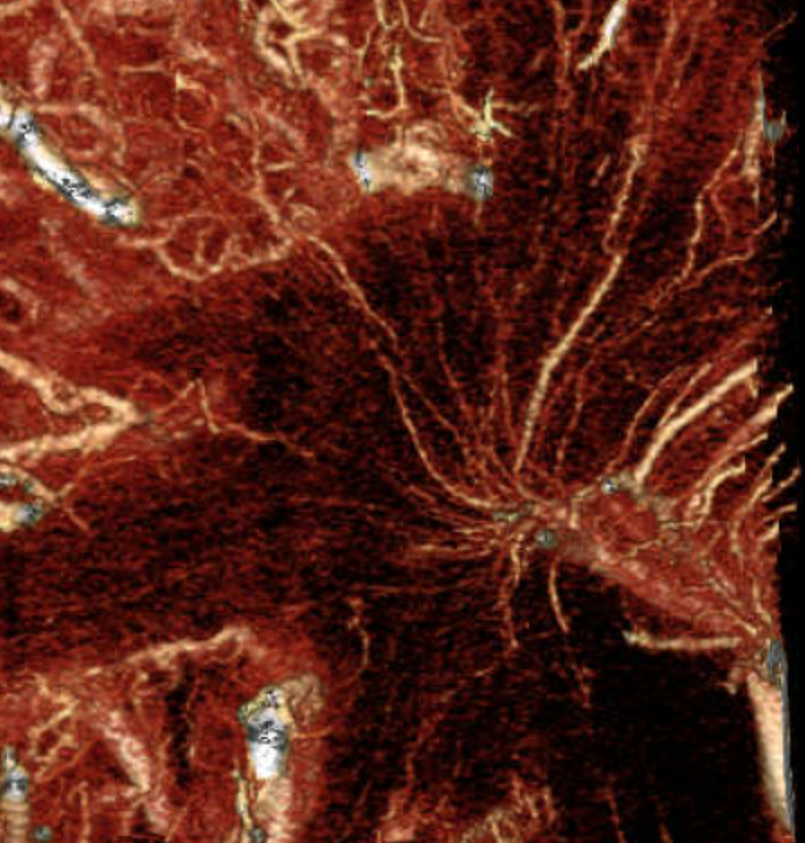

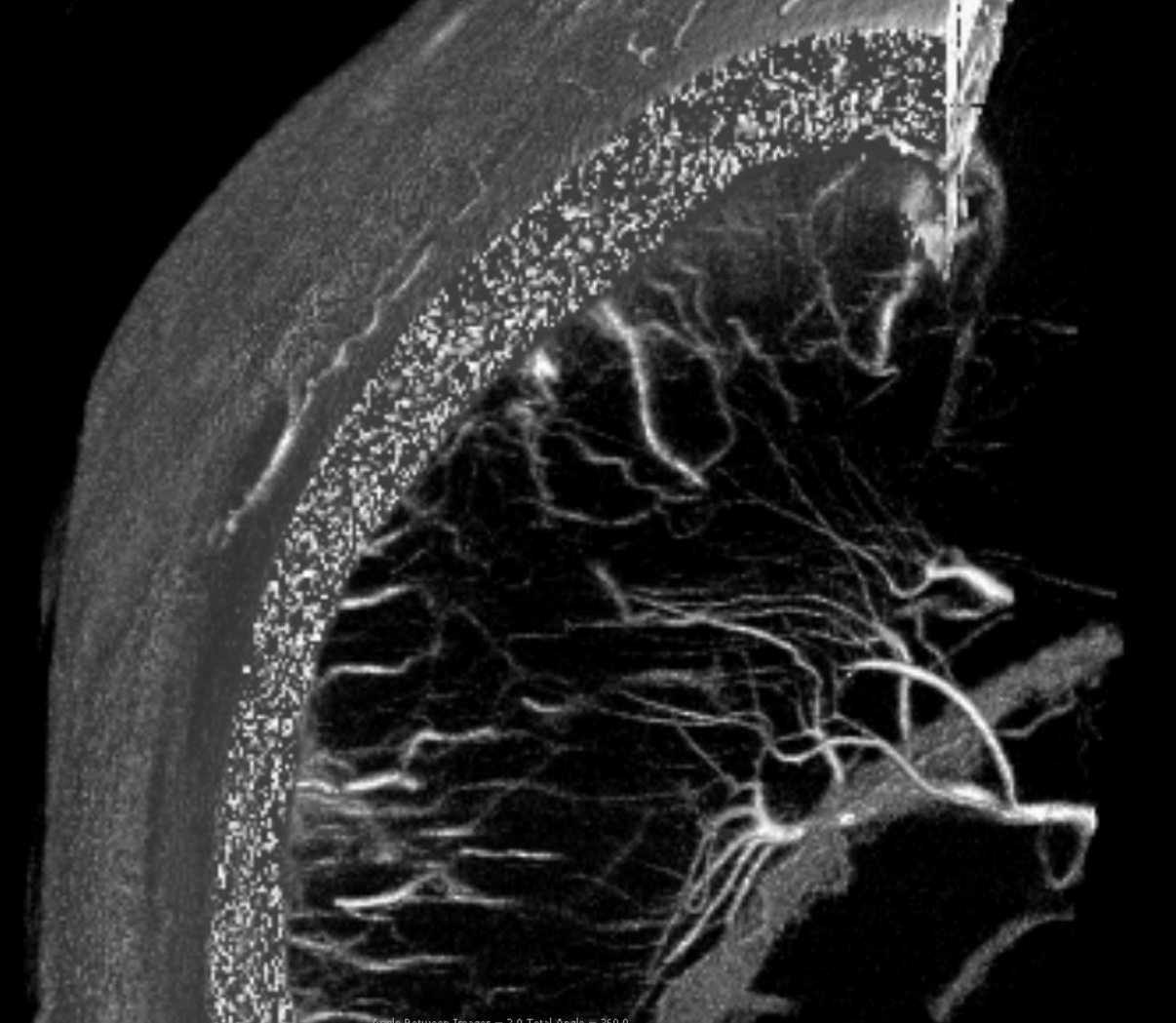
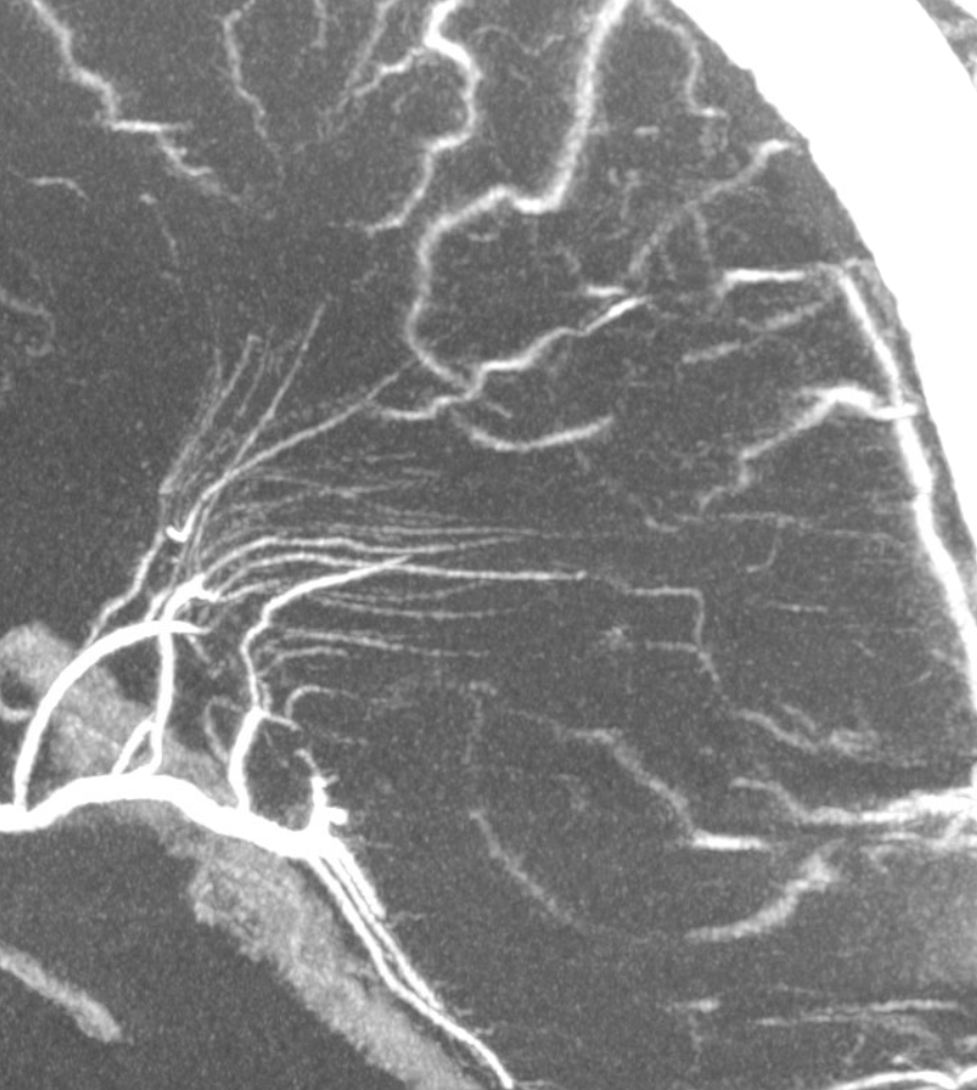
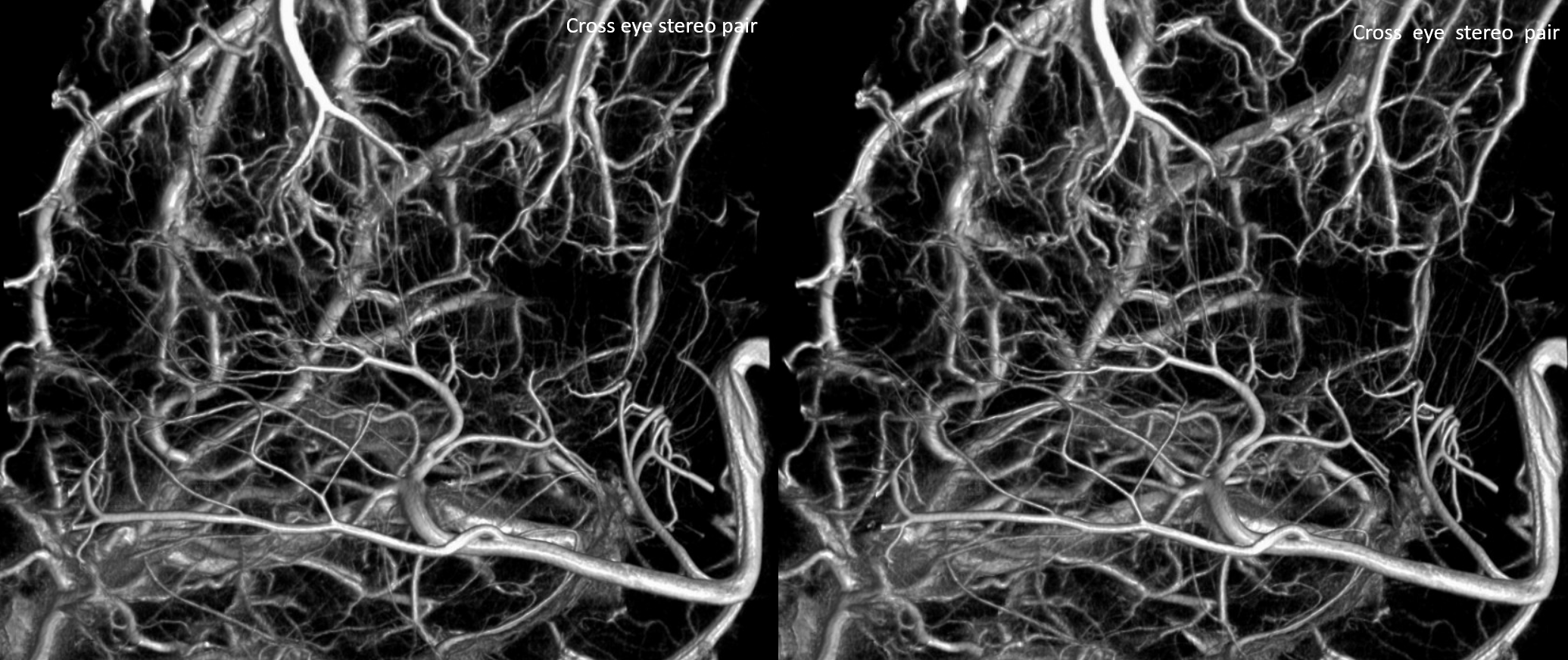
Mixed phase images below — both arteries and veins are shown — in the white matter most by far are veins. Not so many transmedullary ones in this one
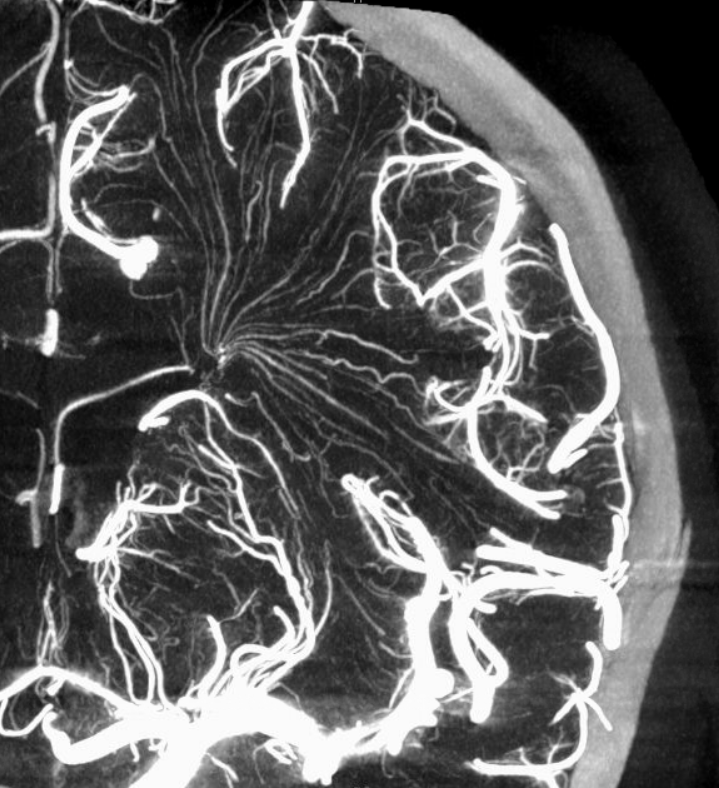

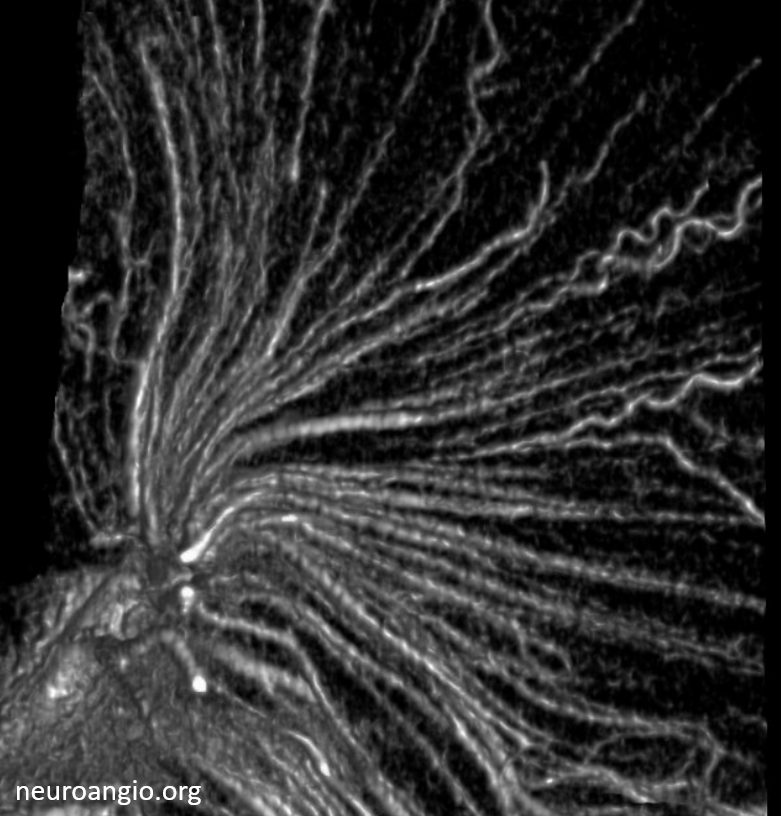
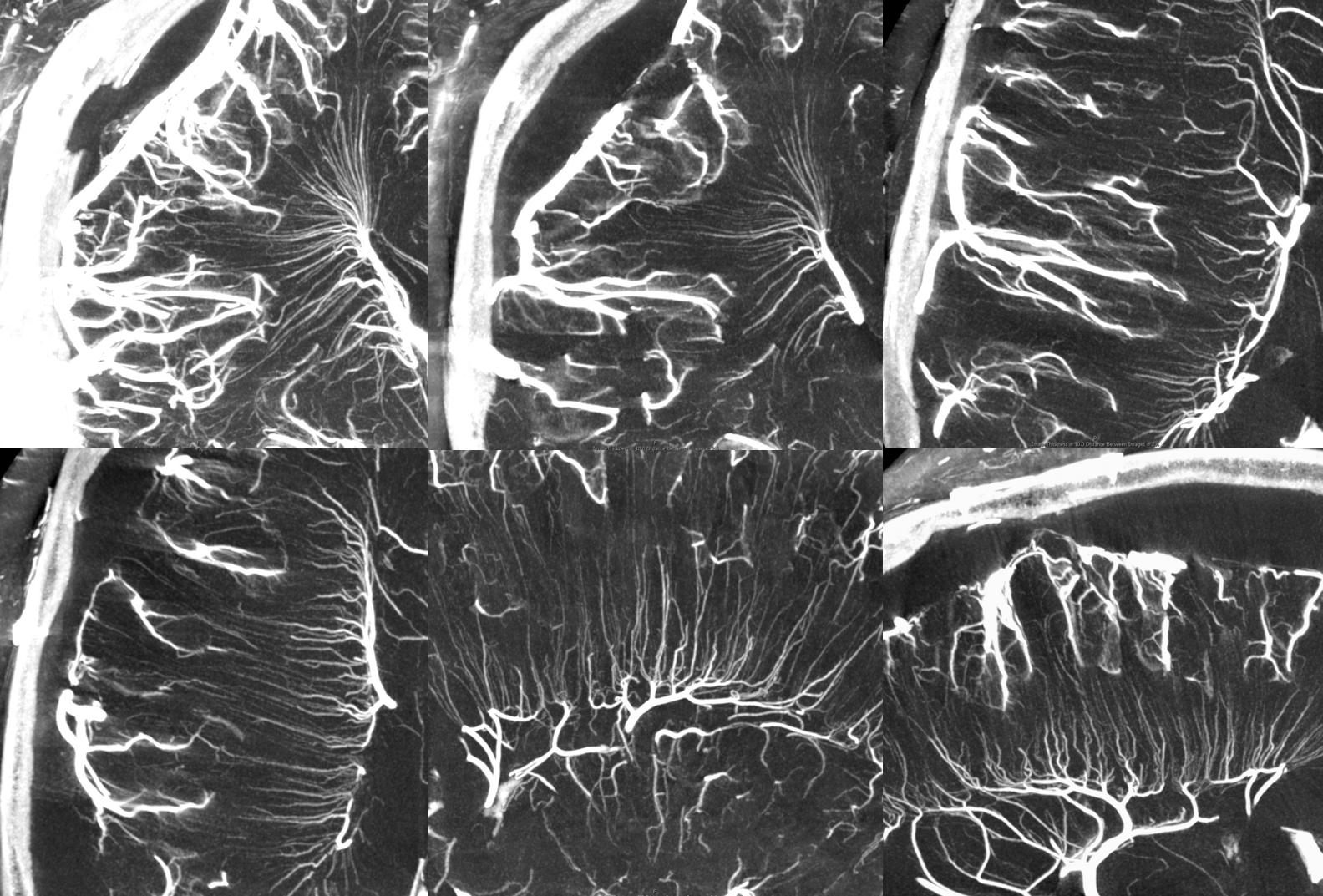
Pure venous phase images below
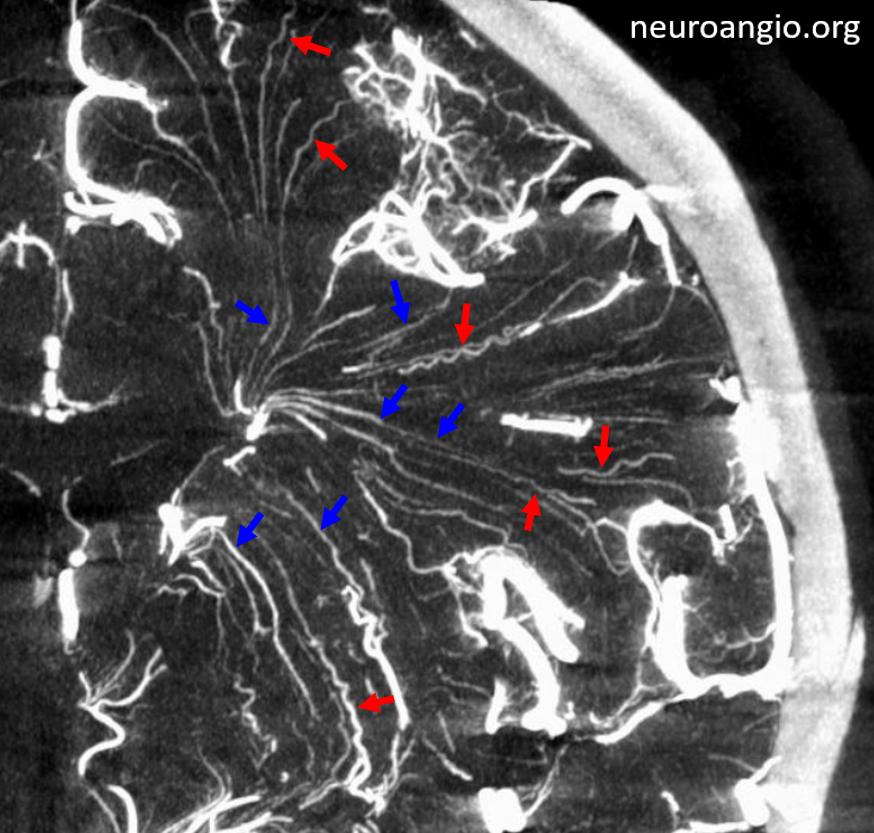
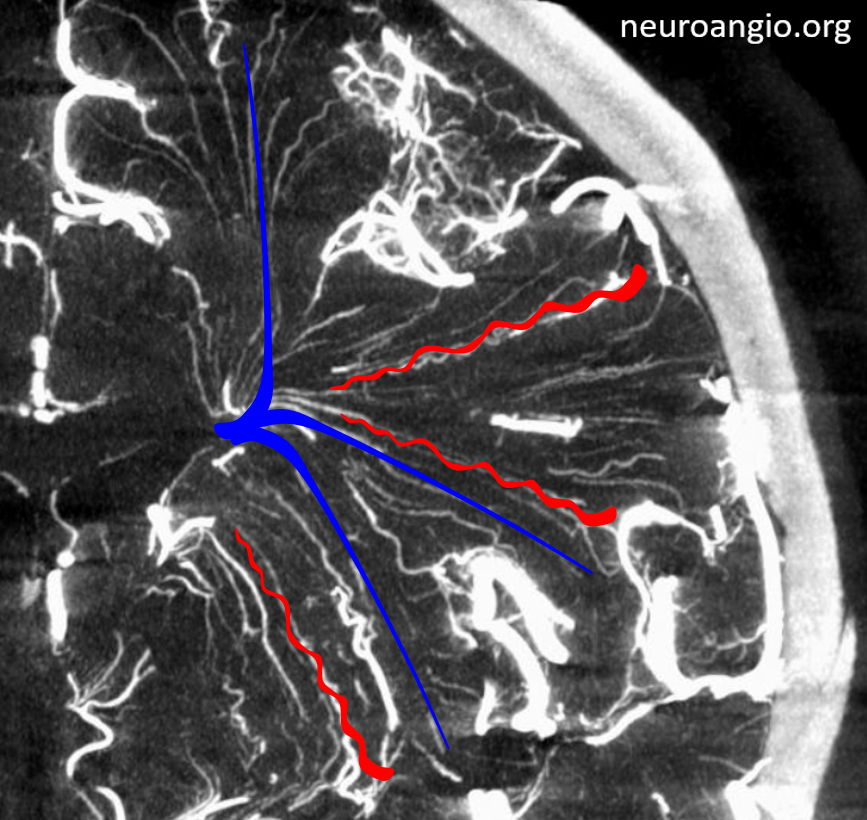
How to differentiate between medullary arteries and veins?
On DYNAs longer than 5-10 seconds, both will be opacified. Telling the difference is not always easy, but there are clues.
Arteries:
- extend from superficial to deep’
- Larger in diameter superficially
- Corkscrew-like in most cases
Veins:
- Mostly extend from subcortical white matter to subependymal areas
- therefore, become larger in diameter as they extend deeper
- Straighter than arteries
Below is a 5 second DYNA, therefore only arteries are seen (arrows) except for a few veins draining basal ganglia
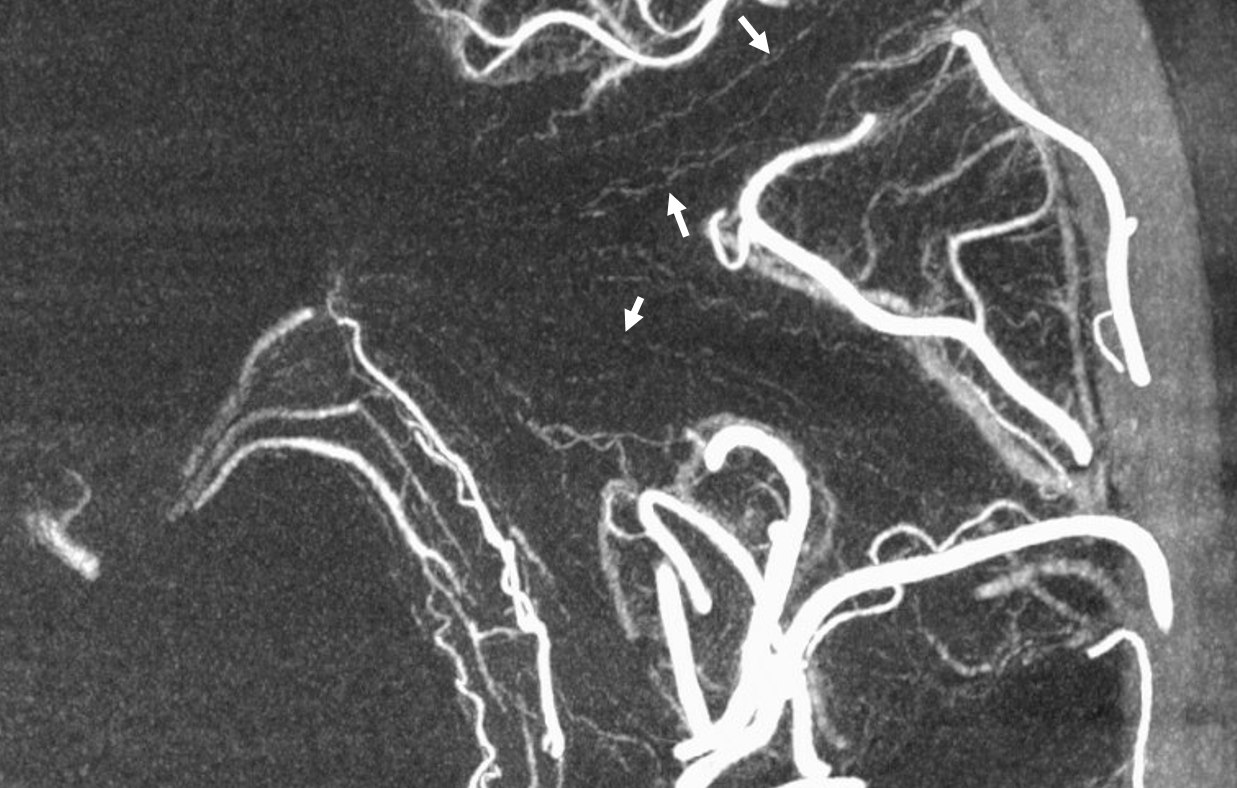
Here are some arrows from an earlier case. Many vessels are difficult to tell…
Like this
Case with subdural hematoma — see mass effect on convexity?
Courtesy Dr. Erez Nossek
Movie — pause to scroll thru individual images
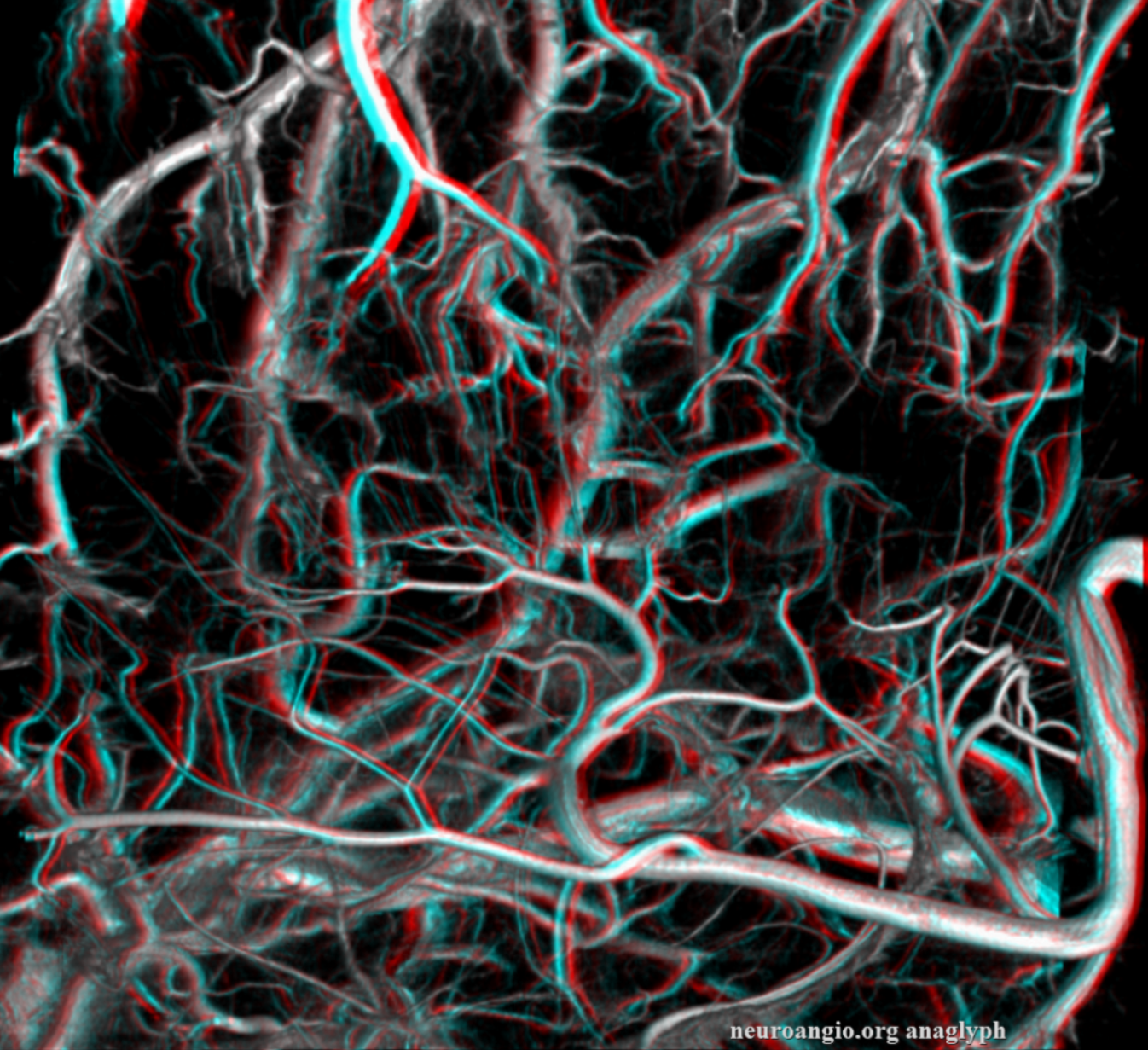
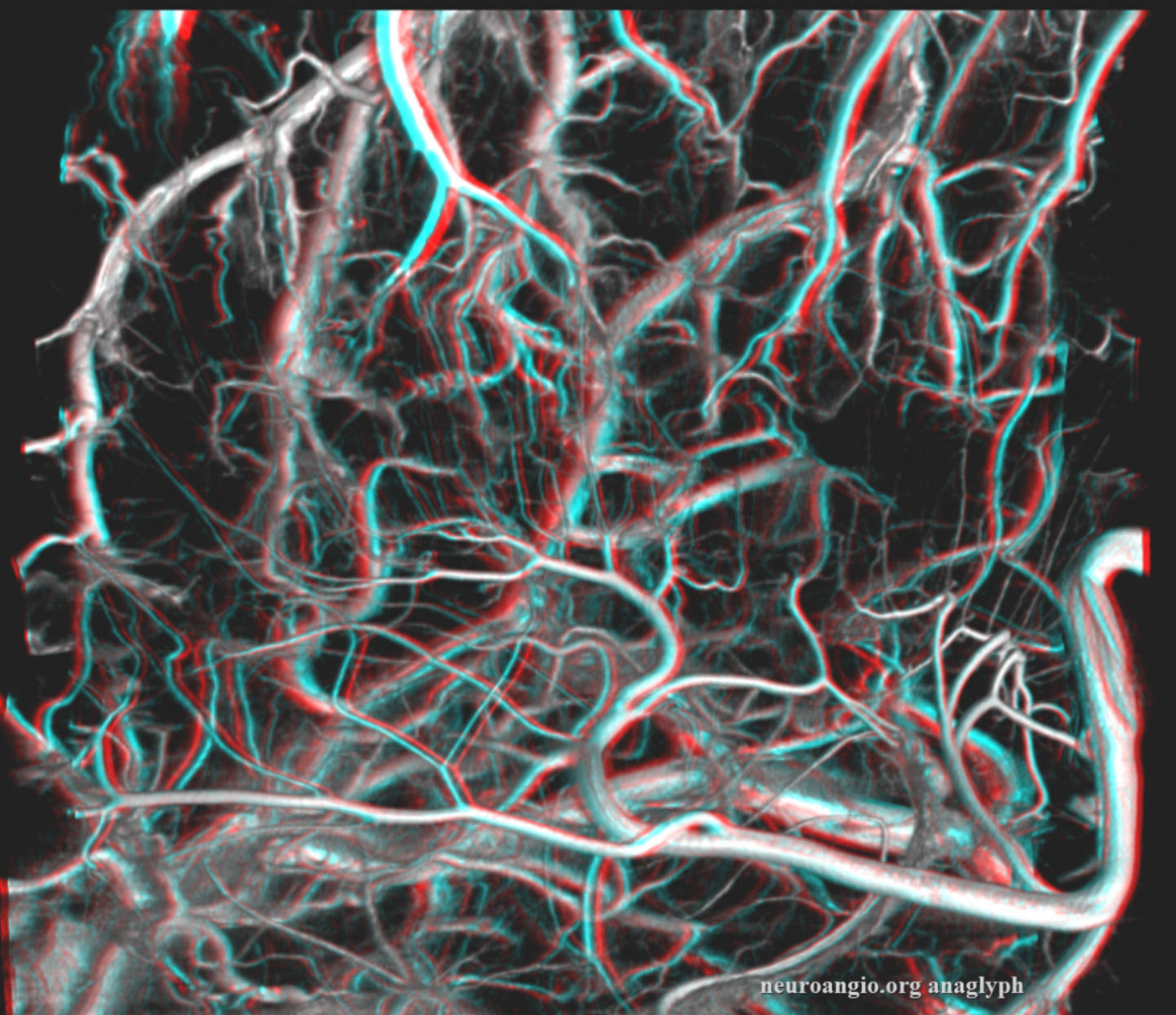
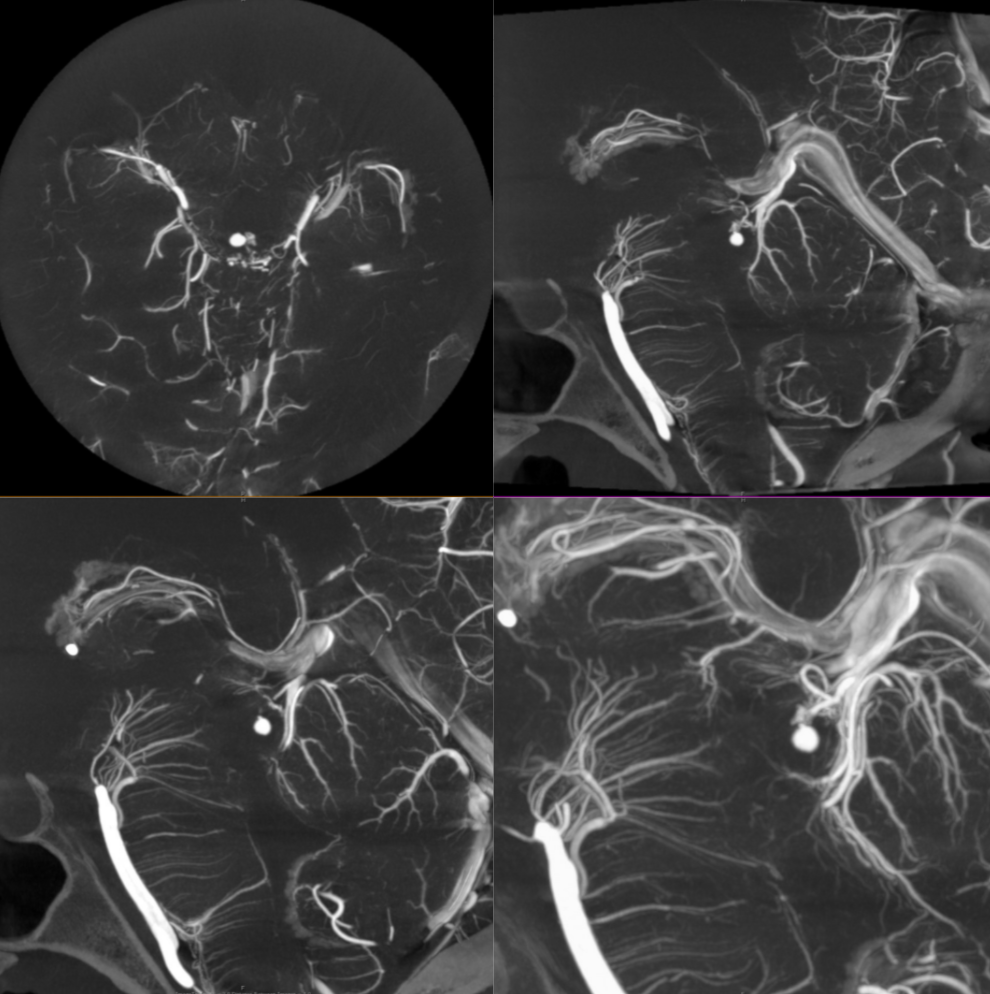
Prominent Subcortical Veins in Cerebritis. Some septic emboli set up shop in the area, inciting a serious inflammatory response. The veins are dilated in all manner of inflammations. This allowed for a decent dataset a 5 sec 3D-DSA to be generated

Homology with Spinal Cord and Brainstem
An idea championed by Lasjaunias, his colleagues, and others, is to see homology / similarity in vascularity of cord, brainstem, and cerebrum. The brainstem to cord similarity is easier to see. However even in cerebrum the similarities are notable. On the venous side, the majority of veins draining the intrinsic substance of the cord / brainstem drain one way — dorsal or ventral. However, the presence of trans-medullary veins, and trans-brainstem ones, is well-documented. Below is a DYNA of a patient with a ruptured tectal plate AVM — you can see both medulla/pons veins draining typically into the anterior pontomesencephalic venous system. a transmedullary vein (pontomedullary junction, lower images) connects to the venous apparatus in the roof of the 4th ventricle (tributary of the vein of lateral recess)
Cases / Pathology
Brain AVM
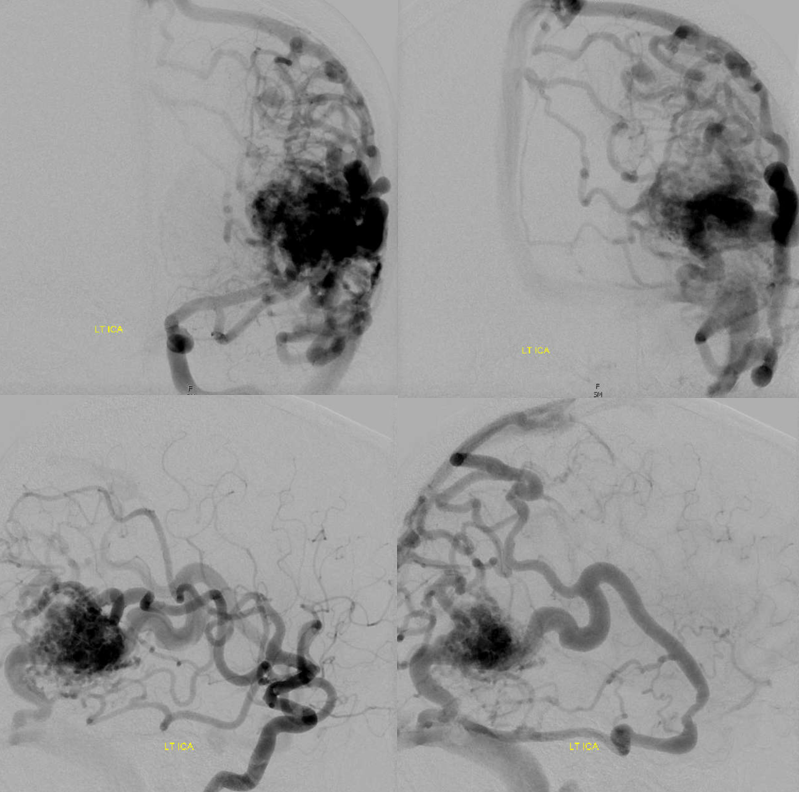
The presence of “deep venous drainage” in an AVM influences the classic Spetzler-Martin grading system, increasing risk of surgical resection. Many AVMs are wedge / pyramid-shaped, with base on cortical surface, extending into the deep white matter to variable degree. It is interesting to note that degree of deep venous drainage does not seem to correlate well with depth of AVM extension — the nidus may extend almost to the subependymal surface and have barely any deep drainage, or not extent too much in and have some. Does that reflect variability in each individual’s baseline venous drainage preference, accentuated by the shunt of the AVM? There is usually one draining vein for the nidus — presumably the enlarged medullary vein — when it comes to surface there may be one or several surface ones, but the intranidal main collector is a medullary vein.
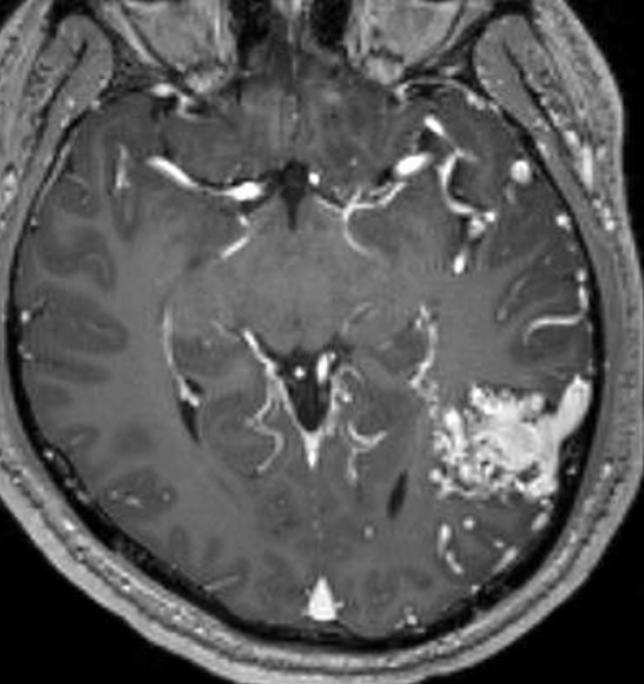
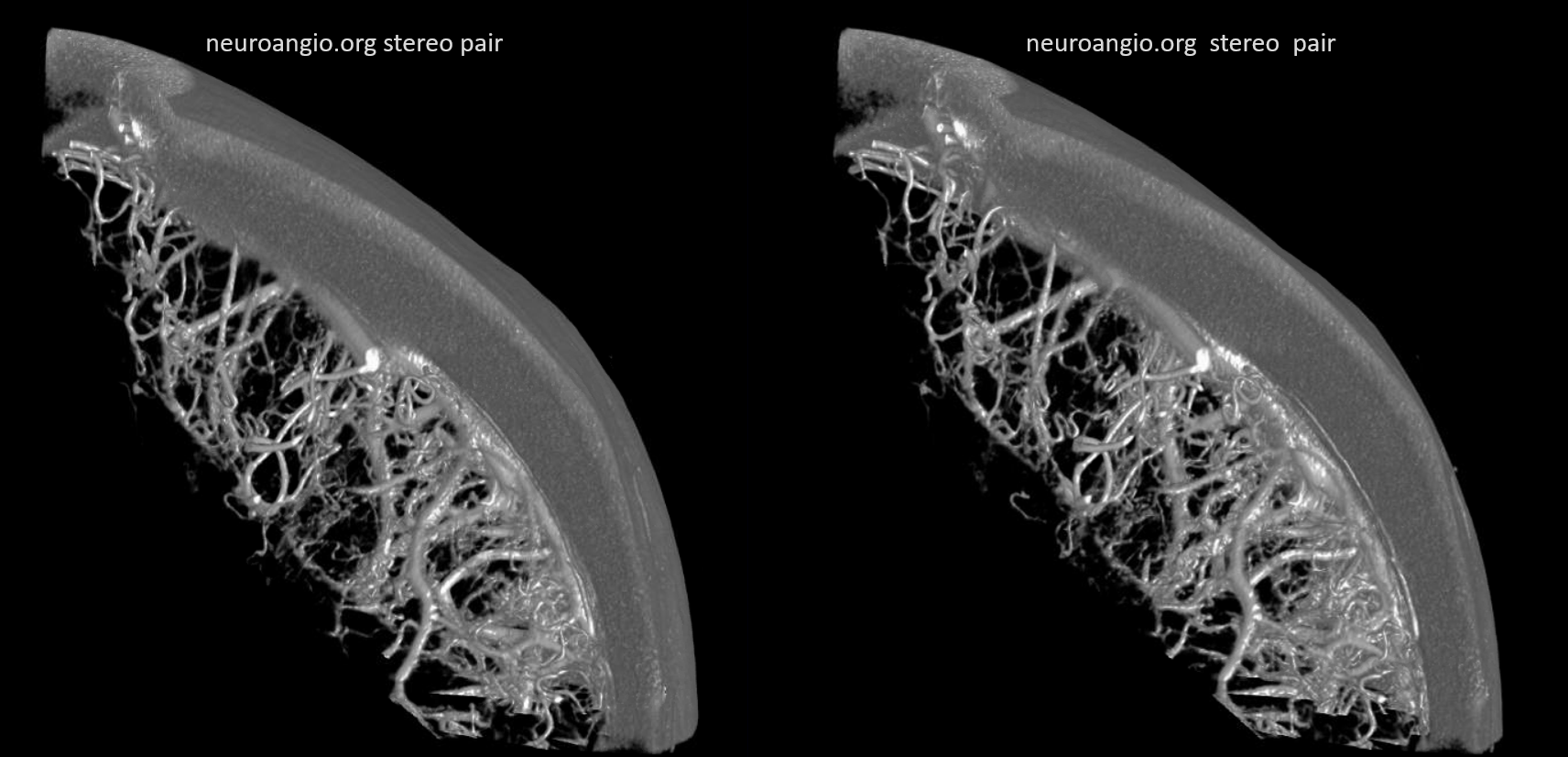
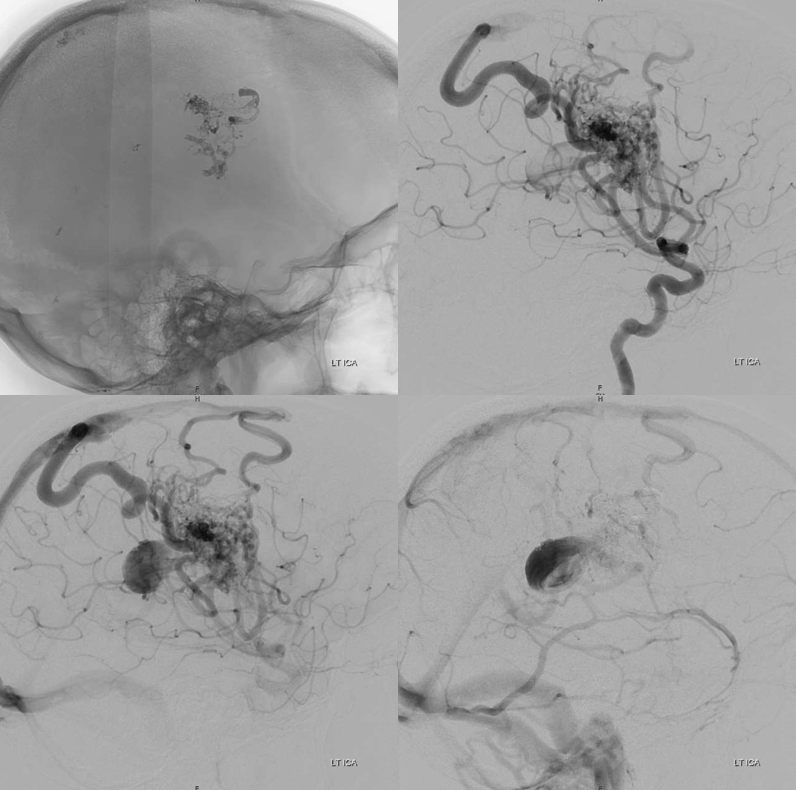
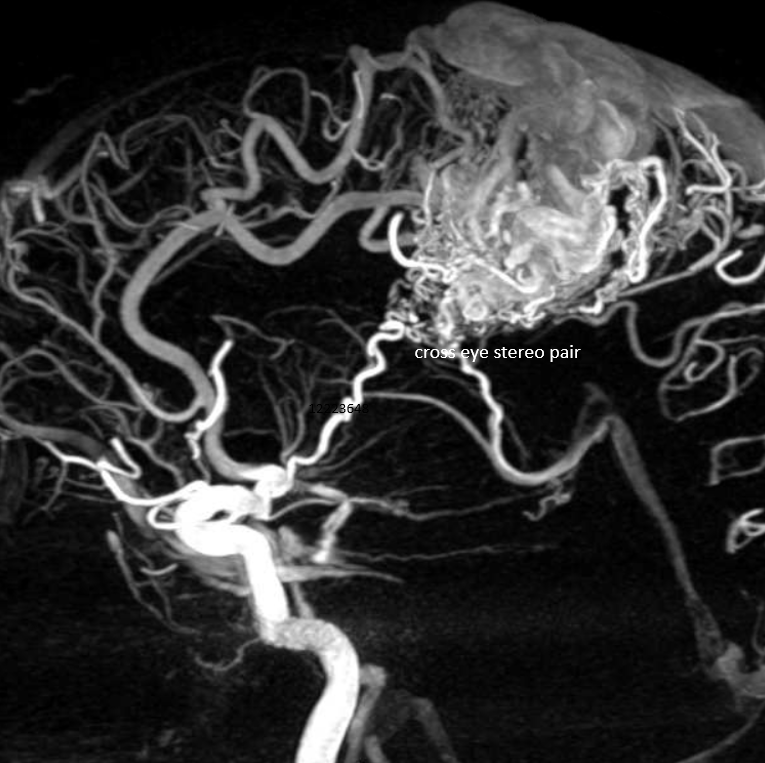
Below are examples of this variability in drainage. In this one there is significant deep drainage, with a pretty rapidly expanding varix causing worsening edema and weakness. Gamma Knife headframe is on right image
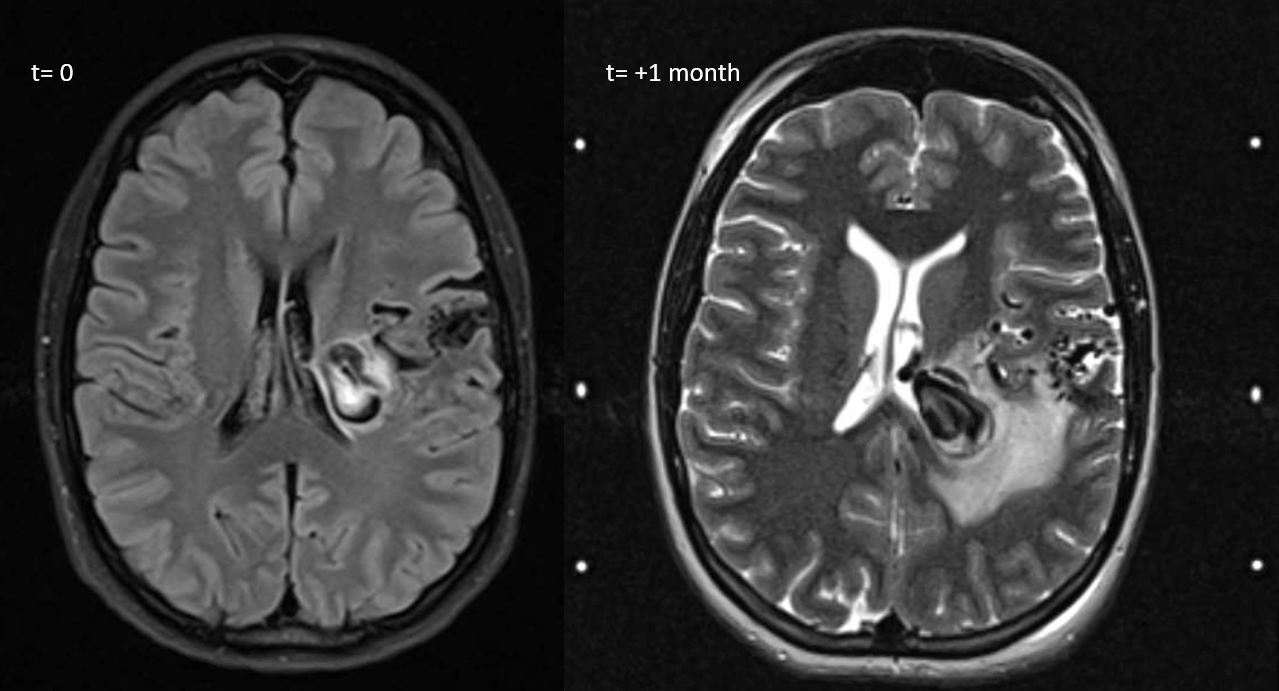
MRI movie — pause and scroll thru individual images
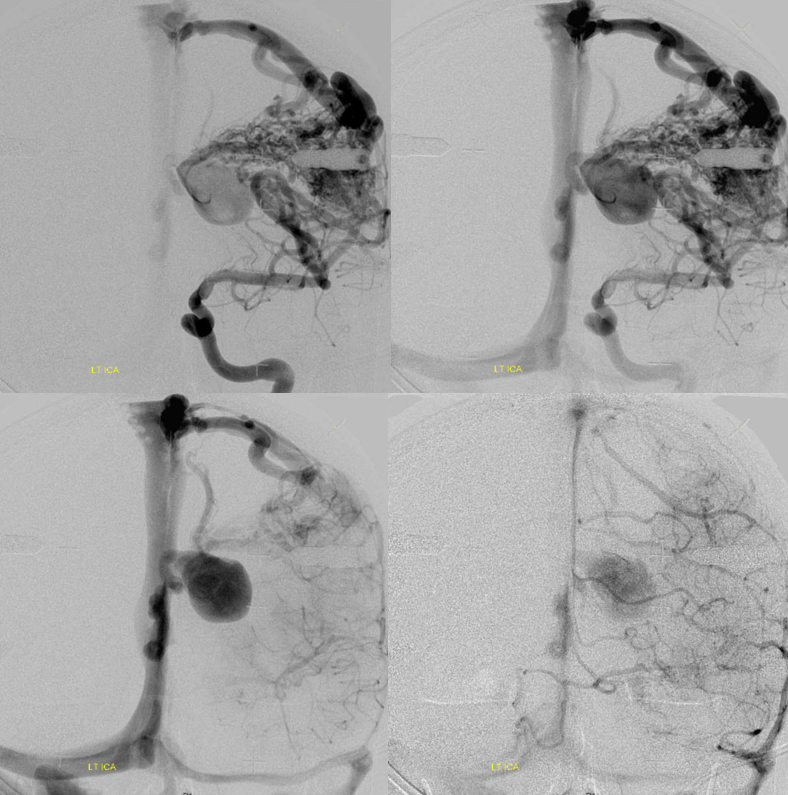
The plan is to Gamma Knife and follow with embolization, targeting the deep component. Pre-embo: notice that one does not need to have deep arterial supply to have plenty of deep venous drainage.
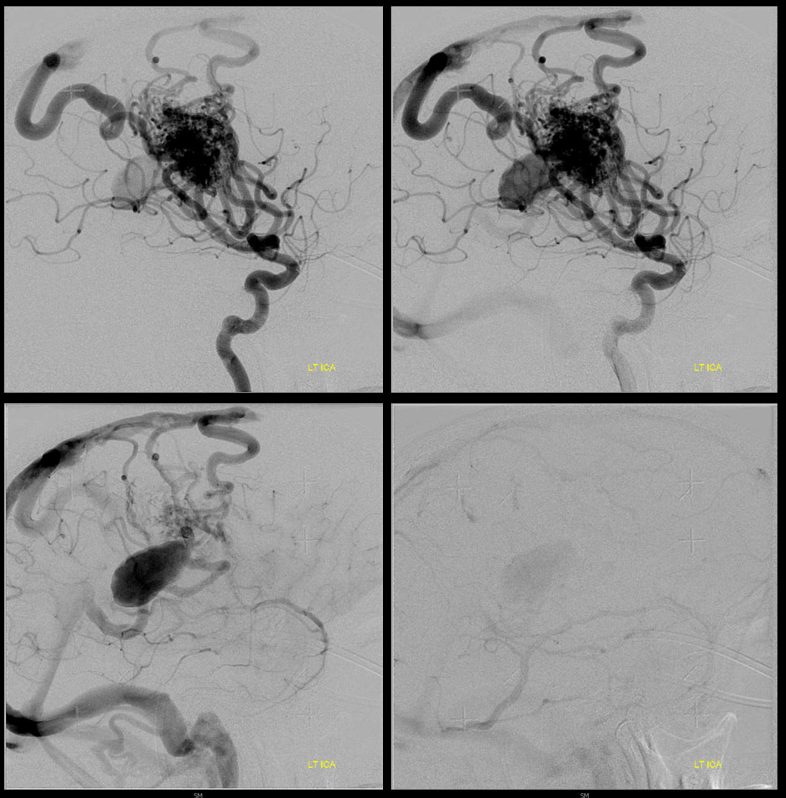
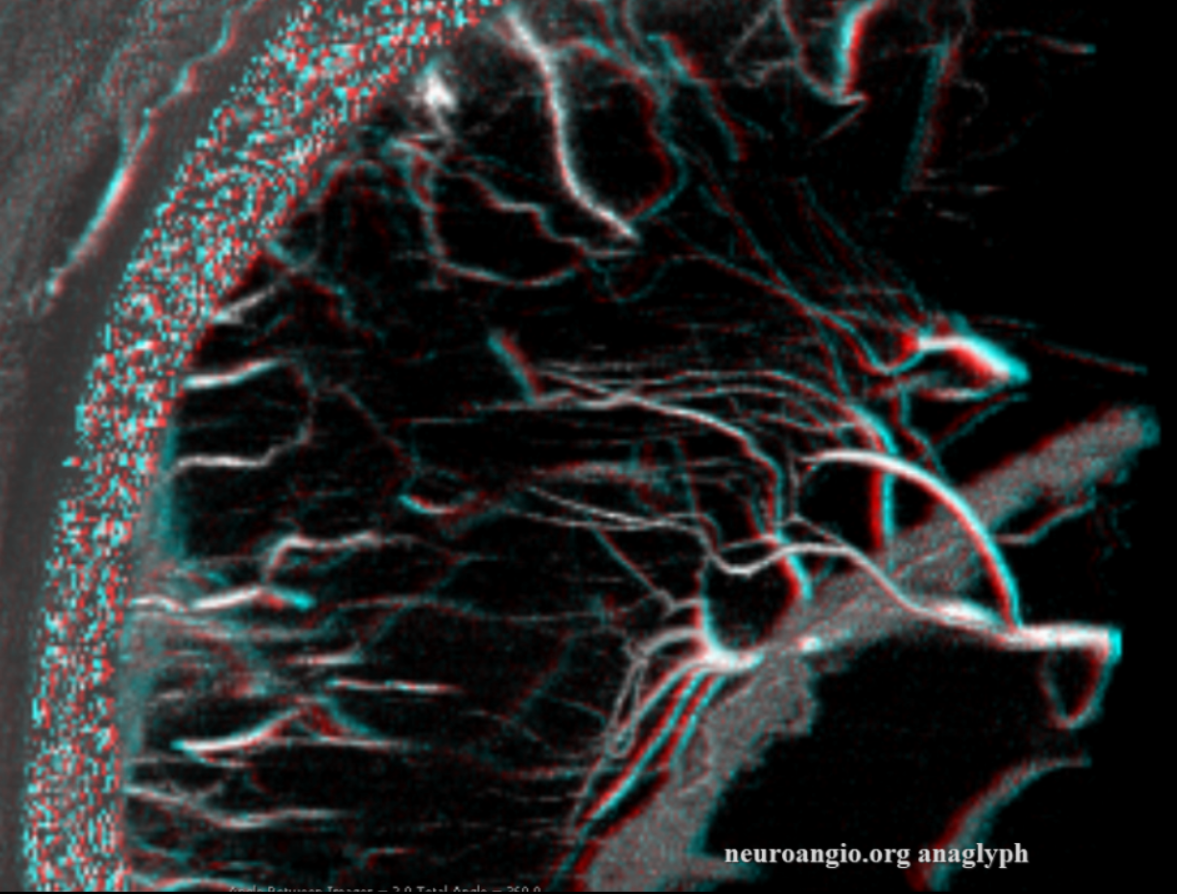
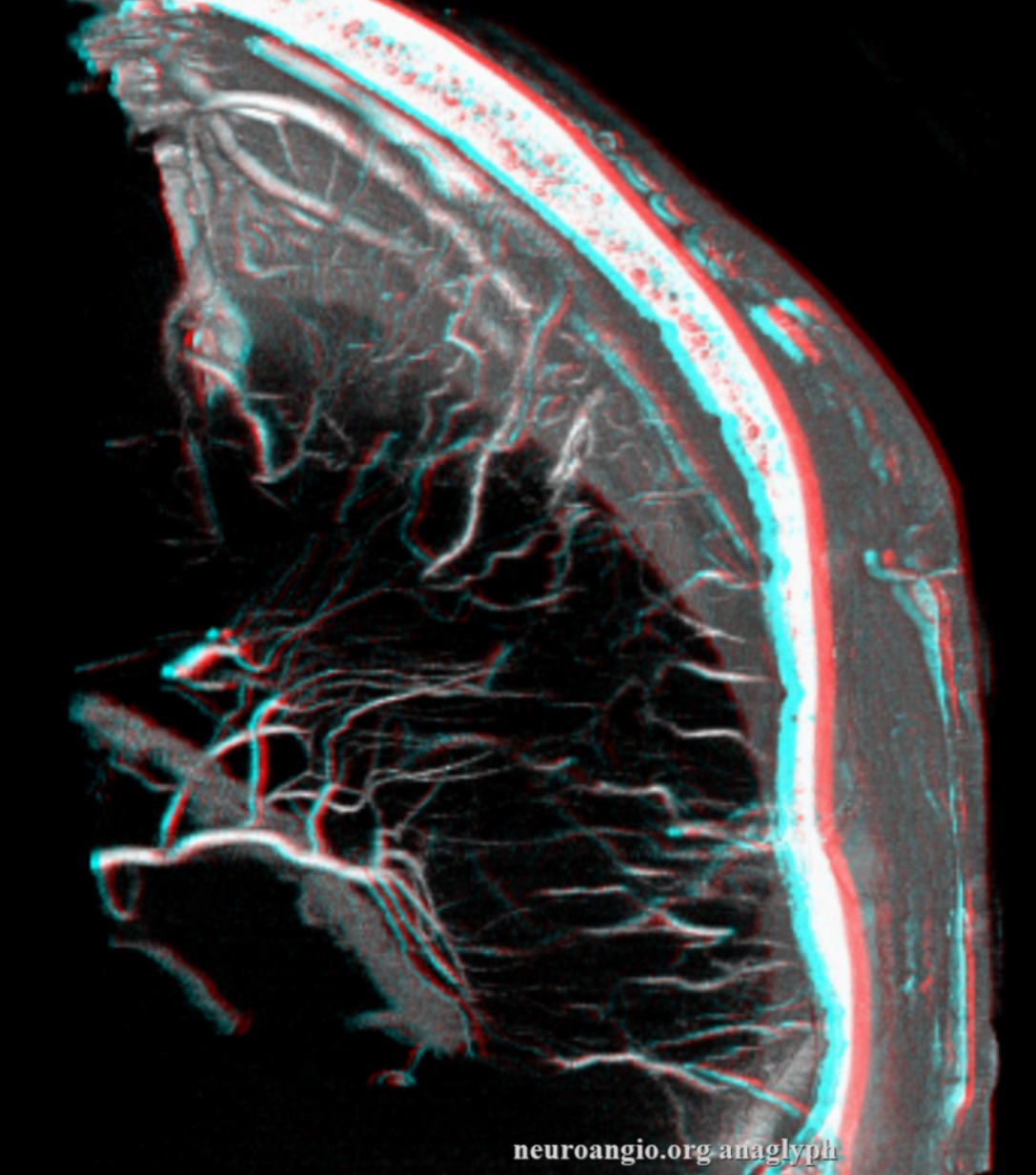
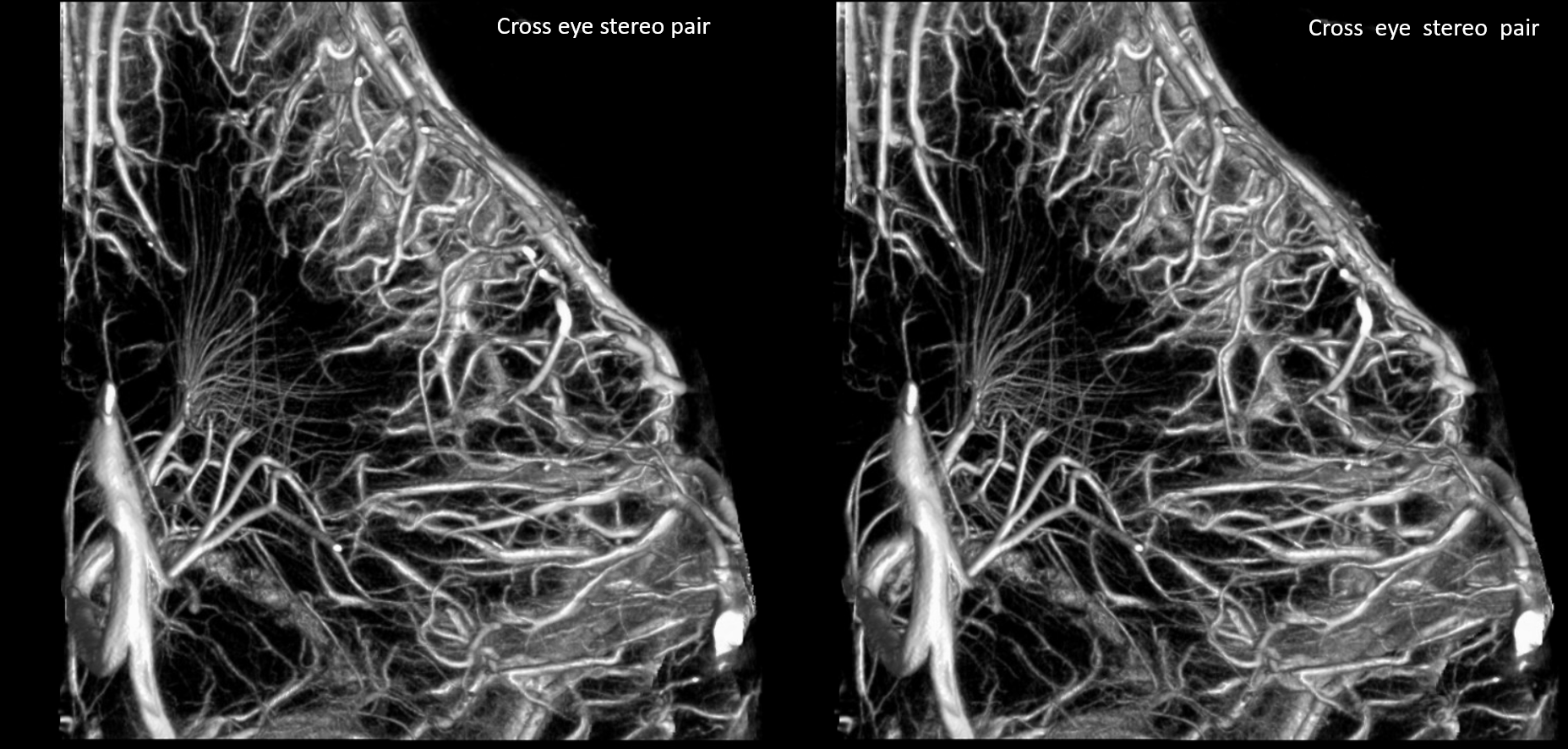
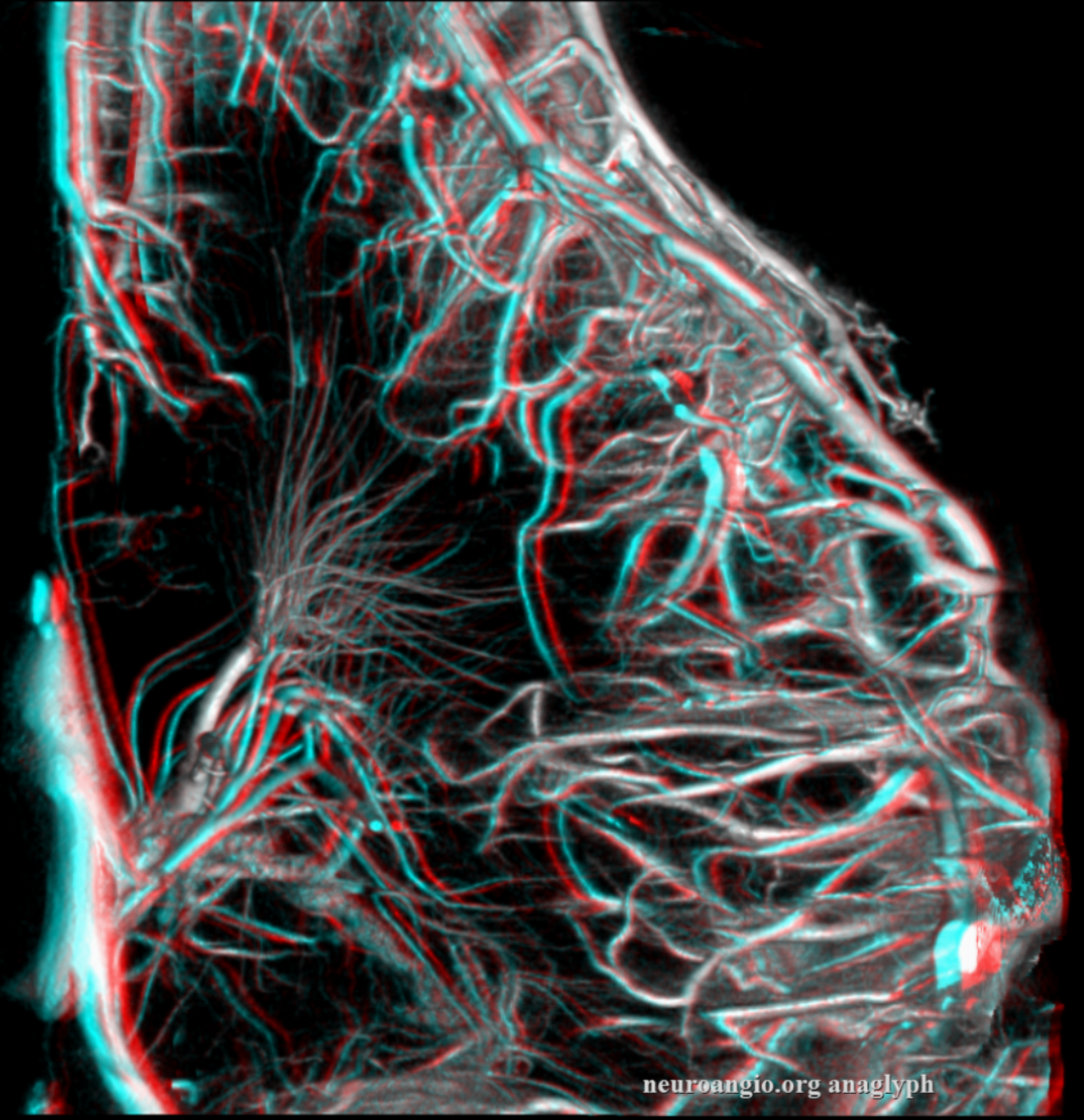
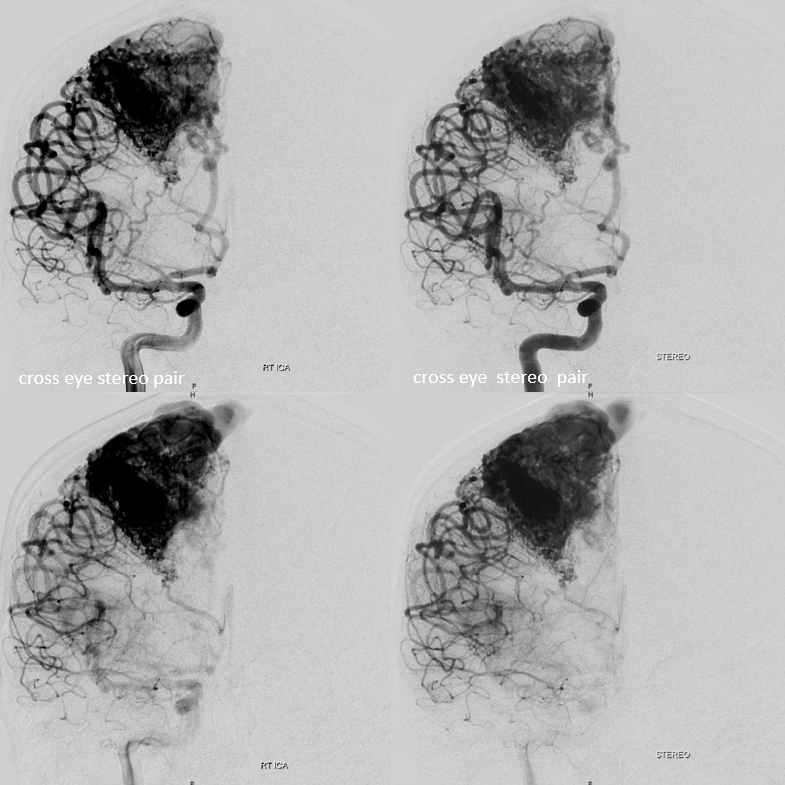
Stereos
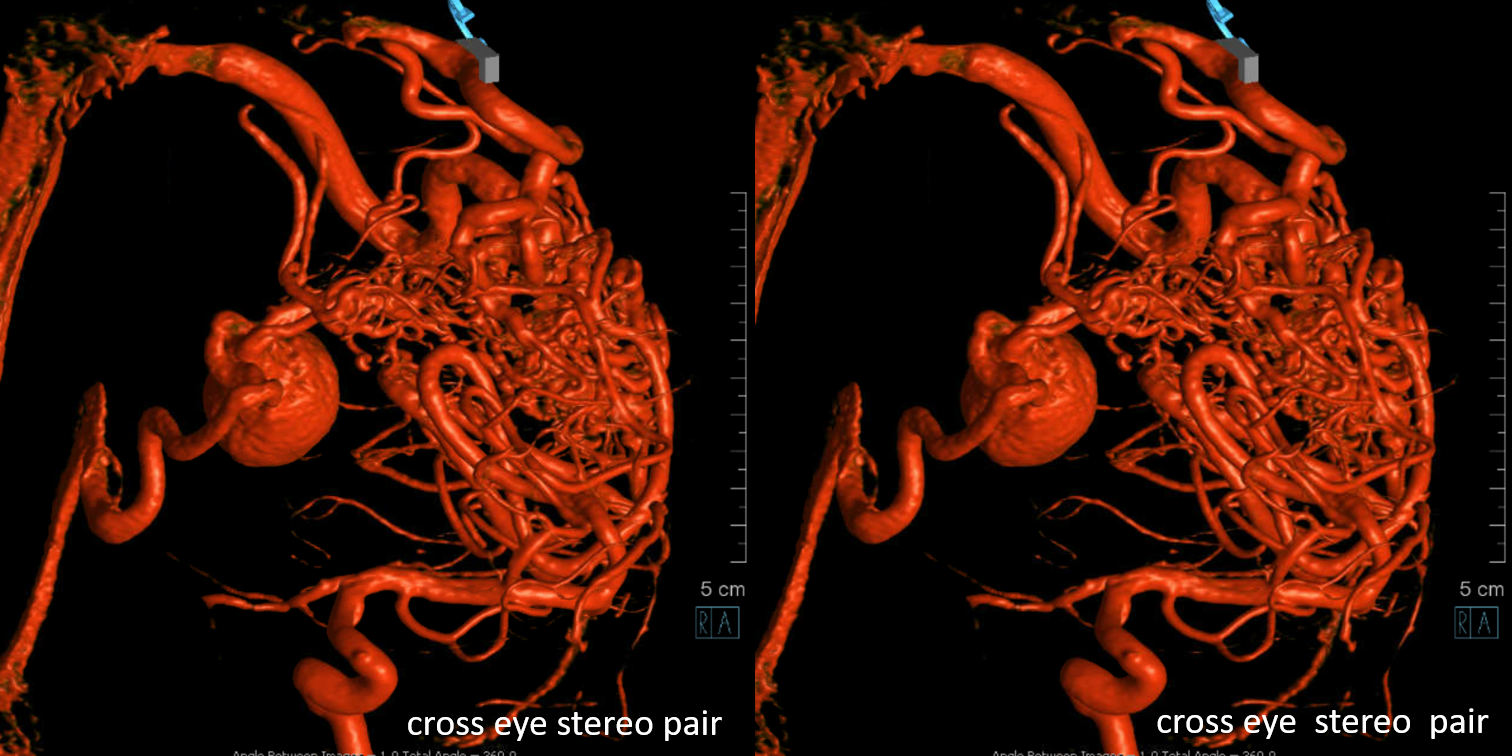
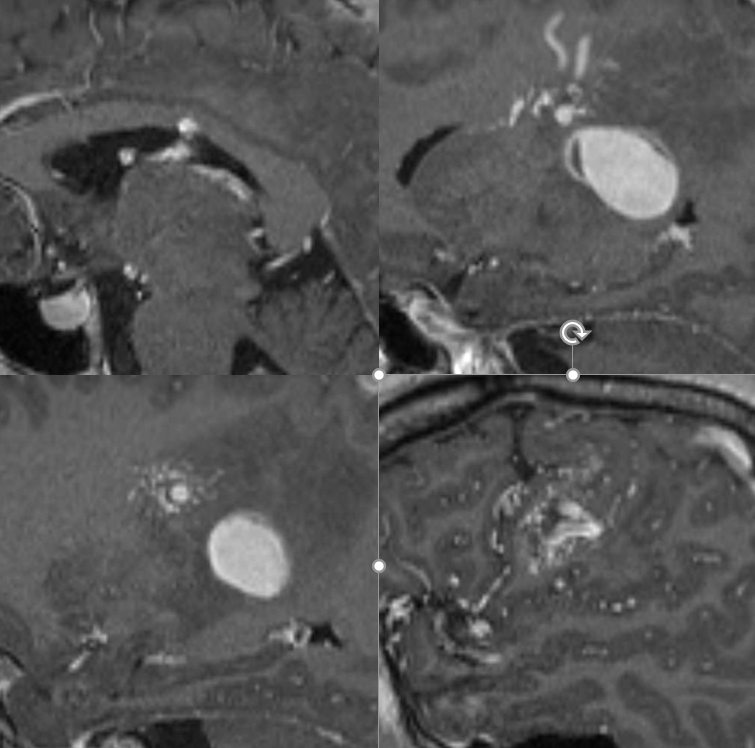
Sagittal MRIs — looking down the barrel of that medullary collecting vein — see how large it is compared to the smaller nidus bottom left picture — because the vein drains deep, it gets larger even though the cross-section of the AVM is smaller in deeper areas. A functionally separate superficially draining medullary vein takes care of the subcortical and cortical nidus (bottom right image)
The embo is obviously high risk — there are sensorimotor white matter tracts (and grey matter cells) right there. Kim Nelson did just fine!
Post embo — mostly nBCA, plus one pedicle with particles (yes, particles are sometimes good for this — to temporarily knock down flow from a position that is not good for liquid embolics). Post embo — a lot less flow though the varix — delayed arrival and stasis — see clot forming in there?
What to do re clot — some heparin overnight and a few weeks of aspirin. Don’t want to overdo it either.
A year later, the AVM is much smaller. The deep vein — lets call it thalamostriate — has shrunk and the varix is gone. A few other notable medullary veins draining upwards towards the parasagittal cortex are still there.
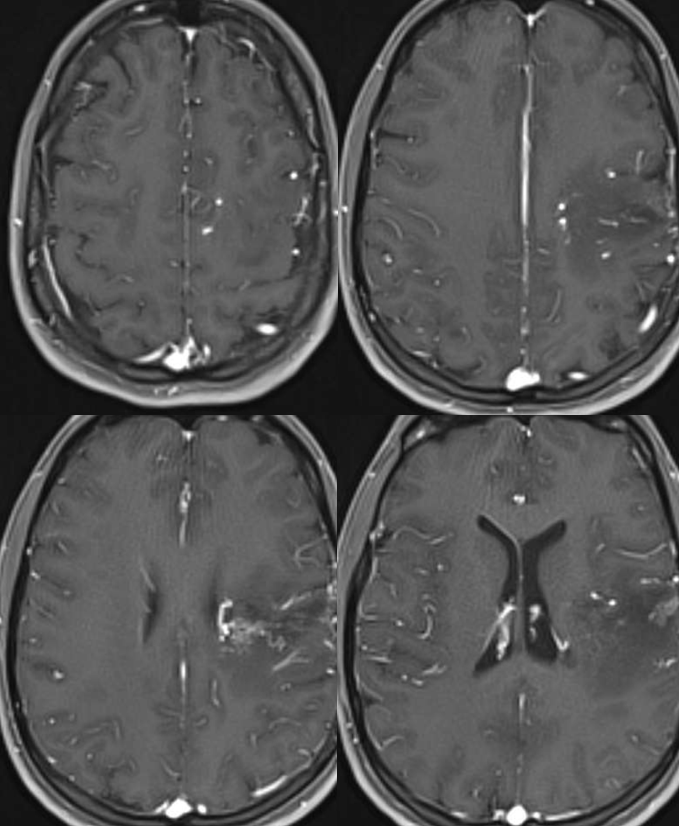
There is impressive “radiation change” — white matter edema extending to subcortical areas. Some necrosis inside the nidus. Nothing unexpected. See that subependymal horseshoe of susceptibility at the lateral posterior border of left ventricle? Is that a radiation-induced cavernoma? Bleed? A good luck charm, courtesy of Gamma Knife Surgeon?
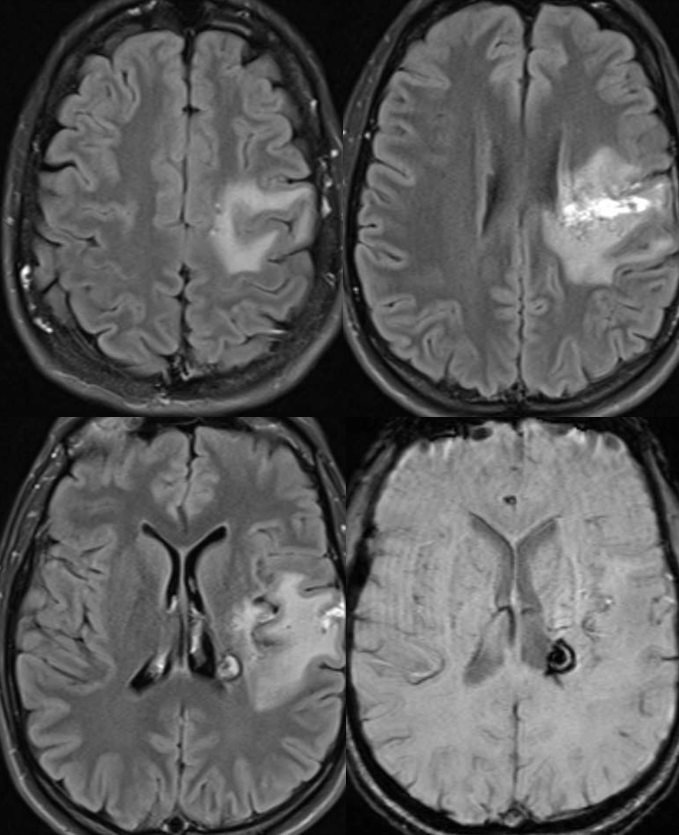
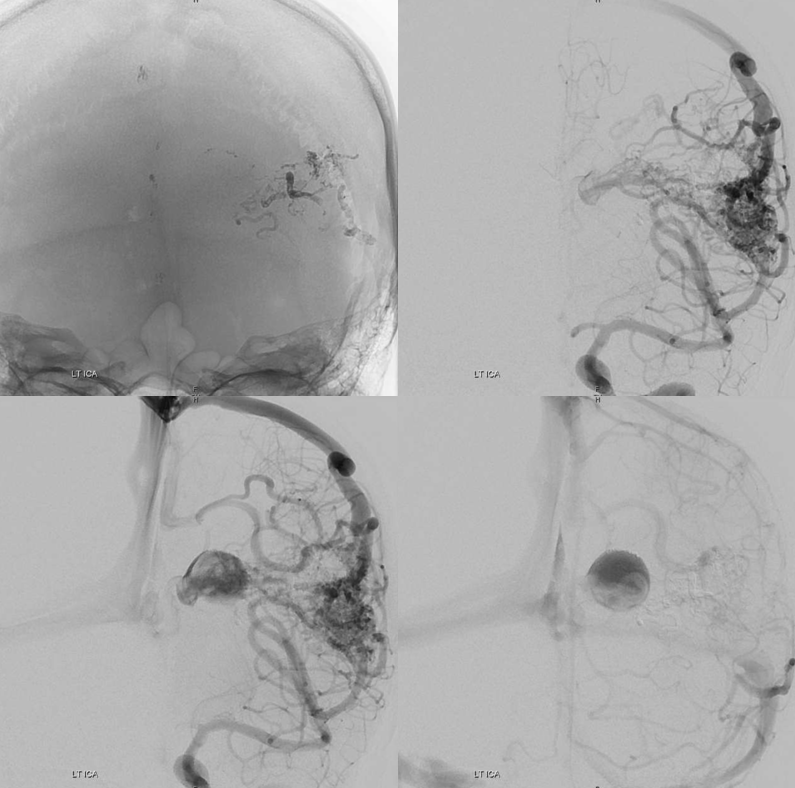
Below is the opposite — a deep extension nidus with some lateral lenticulostriate supply, yet comparatively very little deep drainage.
MRI movie shows well the functionally single medullary draining vein within the center of the nidus
Another one