As noted in several other pulsatile tinnitus pages here, the relationship between venous hypertension, PT, and venous sinus stenosis continues to be defined. Some believe venous stenosis to be the long-sought cause of IH, others feel that high CSF pressure compresses the sinus and thus sinus stenosis is a secondary phenomenon. I believe the latter is true most of the time however there are exceptions including a case illustrated here, where venous stenosis persists despite shunt placement. Here is a case of left-sided pulsatile tinnitus and intracranial hypertension. PT was treated by stenting, is gone, and remains gone. However, IH has recurred after 1 year and a shunt had to be placed. Despite a working shunt, which is now programmable, the patient continues to have venous stenosis just outside of the stent, as is typical. Also, significantly, the patient developed right-sided PT now. Left side remains silent. This case underscores how much we still do not understand about the relationship between venous stenosis and IH
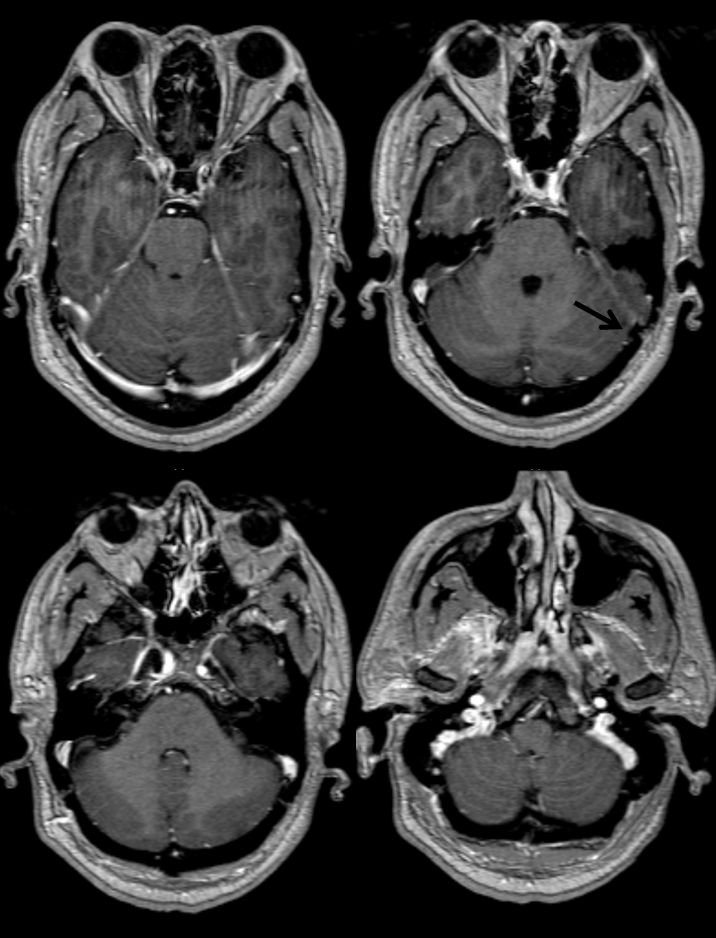
Here is an MRI before stenting. Severe stenosis is evident bilaterally, left (black arrow) more than right
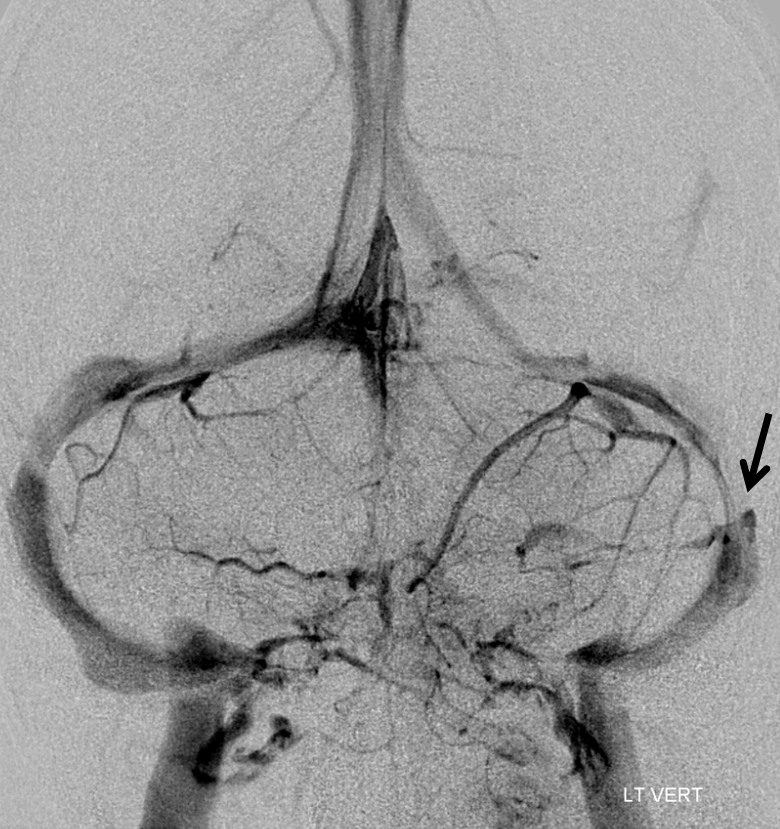
MRV, Time of Flight. Never a pretty study, but shows what you need to see

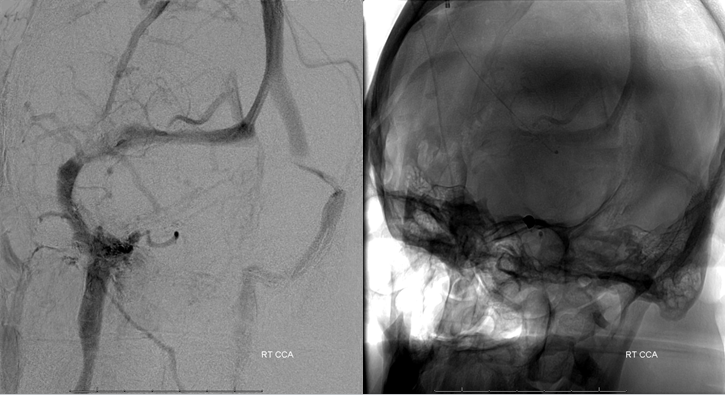
Angio. Vert injection shows bilateral stenosis, left (arrow) greater than right. What is a bit unusual is that the right sided jugular outflow is still mildly dominant. Usually the sound is on the side of the bigger sinus and jugular vein. Here, probably because the left side is still pretty sizable and left sided stenosis is much worse, the sound was on the left.
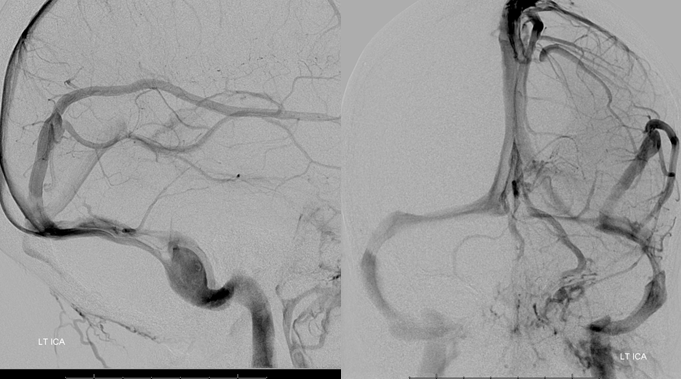
Frontal and lateral views of left ICA injection show pretty severe stenosis on left. There is a large dural venous sinus present at hte posterior temporal/occipital region (not marked, but illustrated in the Venous Sinuses section.
Closeup of left sigmoid stenosis

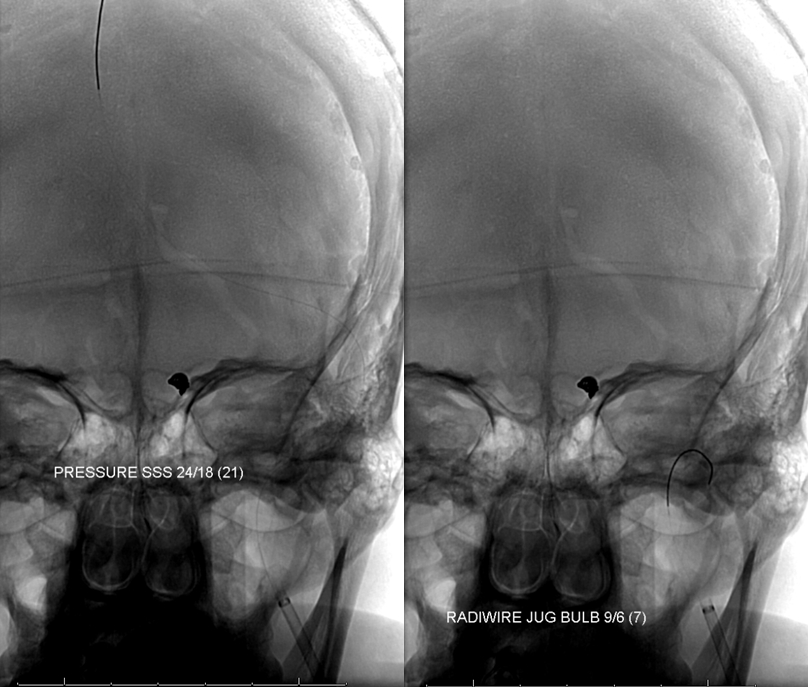
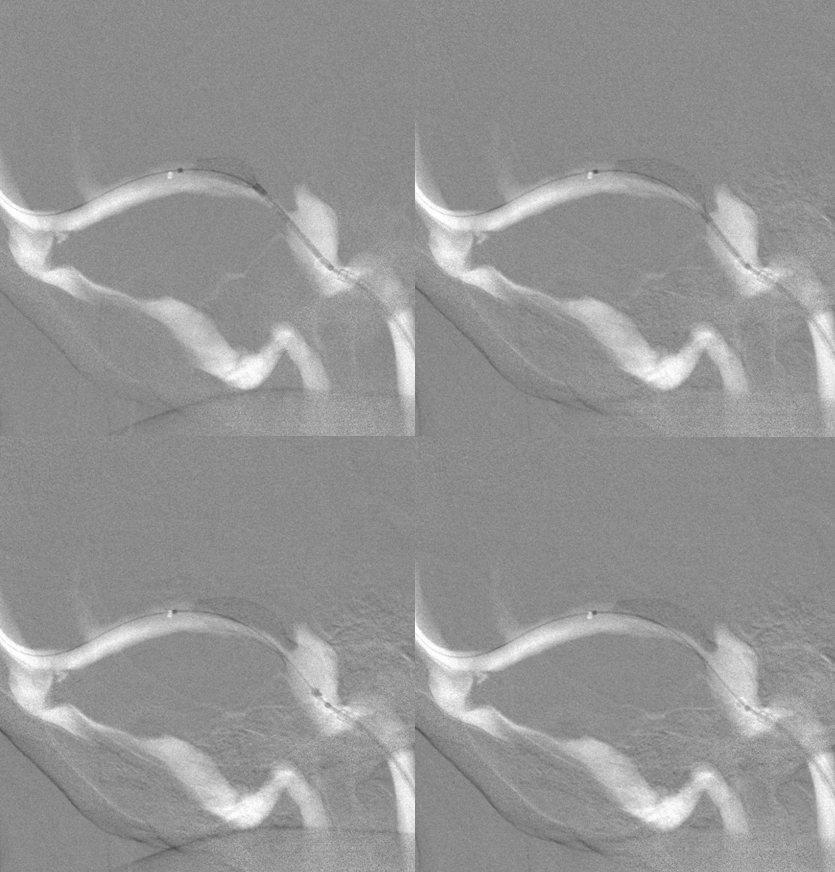
Pressure gradient measurements. That’s a pretty big gradient
“Precise” stent deployment
Post-stenting venous injection

Venous phase of left CCA injection, shows no preferential left-sided outflow with moderate persistent right-sided (black arrowhead) stenosis
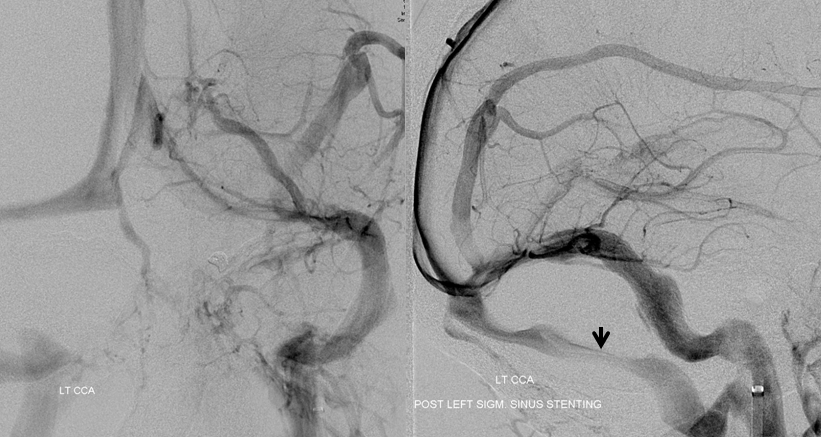
left-sided PT has disappeared and remains silent. Two years later, however, there is recurrence and shunt placement (white arrow). Despite working shunt, there is also recurrence of narrowing in the transverse and sigmoid sinus just distal to the stent (black arrow) and persistent right sigmoid stenosis (black arrowhead). It would be expected that working shunt would normalize CSF pressure and there would no longer be sinus stenosis either outside of stent or on right side if CSF pressure was the primary problem and venous sinus stenosis secondary. This does not seem to be the case here

Despite narrowing outside of stent on left, the left side is silent. There is however now new right-sided PT. This is likely due to reduction of left-sided outflow due to aforementioned left transverse and sigmoid sinus stenosis, which results in higher right-sided flows. The patient remains under observation
Conclusion: Relationship between PT and IH and venous stenosis remains complex. However, we know one thing — if there is venous sinus stenosis and pressure gradient across it, and PT on that side is abolished by ipsilateral jugular compression (proof that venous stenosis is cause of PT), stenting works and is durable, even if IH recurs.
Back to Diagnosis and Treatment of Pulsatile Tinnitus home page
