Here is a more nuanced case of venous pulsatile tinnitus. Venous sinus stenosis is perhaps the most under-recognized cause of pulsatile tinnitus today. See Venous Sinus Stenosis page and Cases 1 and 2 of venous sinus stenosis and stenting for more information. Venous sinus stenosis is frequently associated with post-stenotic dilatation which can also be described as a diverticulum. Paradoxically, venous sinus diverticulum is perhaps more often listed as a cause of pulsatile tinnitus than sinus stenosis itself. In most literature cases, there is no proof that either diverticulum or the “high riding jugular bulb” — another favorite scapegoat for PT, really did cause PT in cases described. The reason is that in most cases neither case is treated. Most case descriptions do not include critical clinical information such as whether the sound can be suppressed by jugular compression. The bottom line is that, in my view, diverticulum is not as important a cause of PT as sinus stenosis. So, this case is shown as an exception, where diverticulum is in the end felt to play key role in PT.
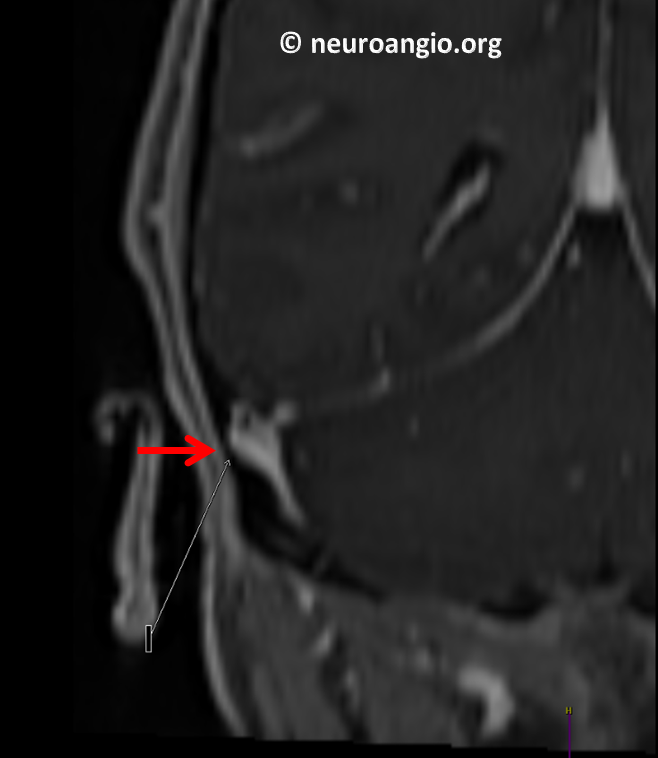
History is typical — severe, constant right-sided PT, completely suppressed by right neck compression. This last sign is key — whether the cause is stenosis, diverticulum, jugular plate dehiscence, etc. — as long as PT has something to do with flow in the transverse/sigmoid/jugular pathway, compression of ipsilateral jugular vein should consistently stop the sound. If it does not, chances of whatever it is that does not right about the sinus causing PT is very low. Any diverticula, stenoses, etc are likely unrelated. Unless the patient has extremely well-developed suboccipital veins, which themselves may be a reflection of C1-level lateral mass jugular vein stenosis. As you can see, simple severe sigmoid sinus stenosis is classic — however things can get a bit more nuanced. In situations such as these clinical experience is key. We rely very heavily on the jugular compression sign. Here is MRI, showing relatively mild stenosis (white) with a post-stenotic diverticulum (red). It is stil likely that the diverticulum is flow-related with jet of flow remodeling bone

Coronal view with diverticulum also pointed out by reading neuroradiologist
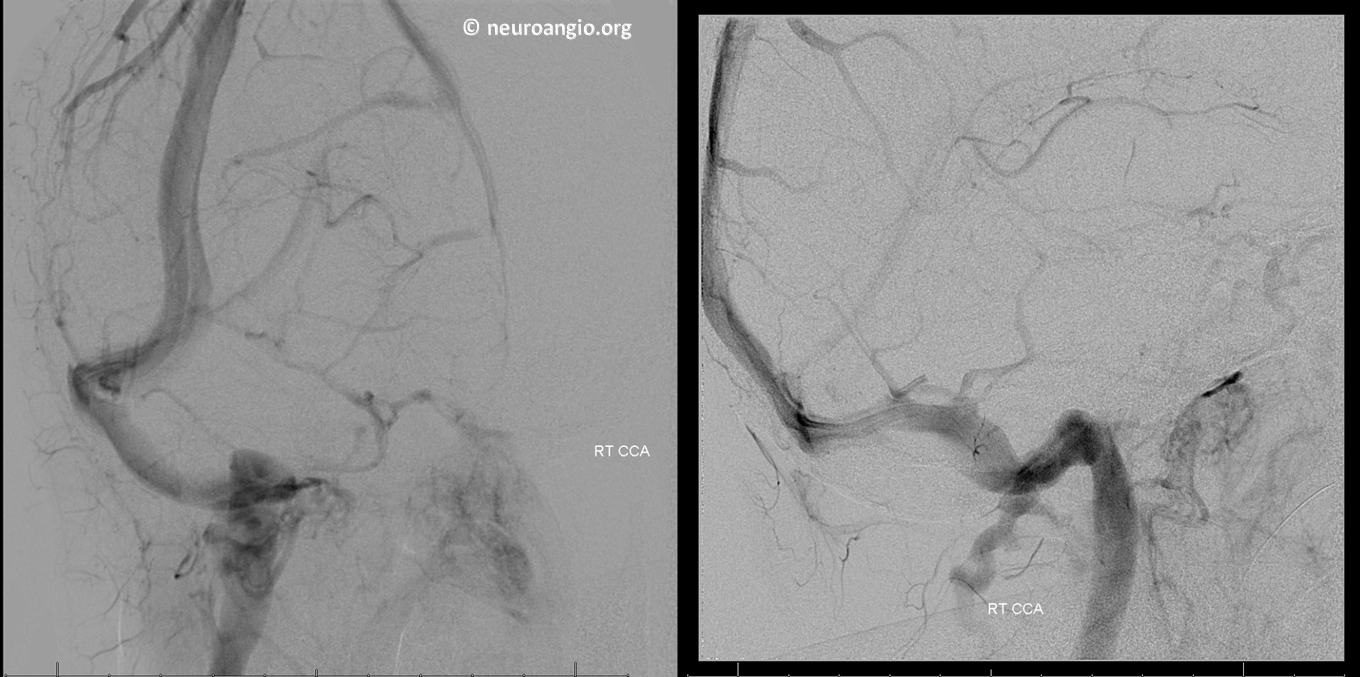
Angio
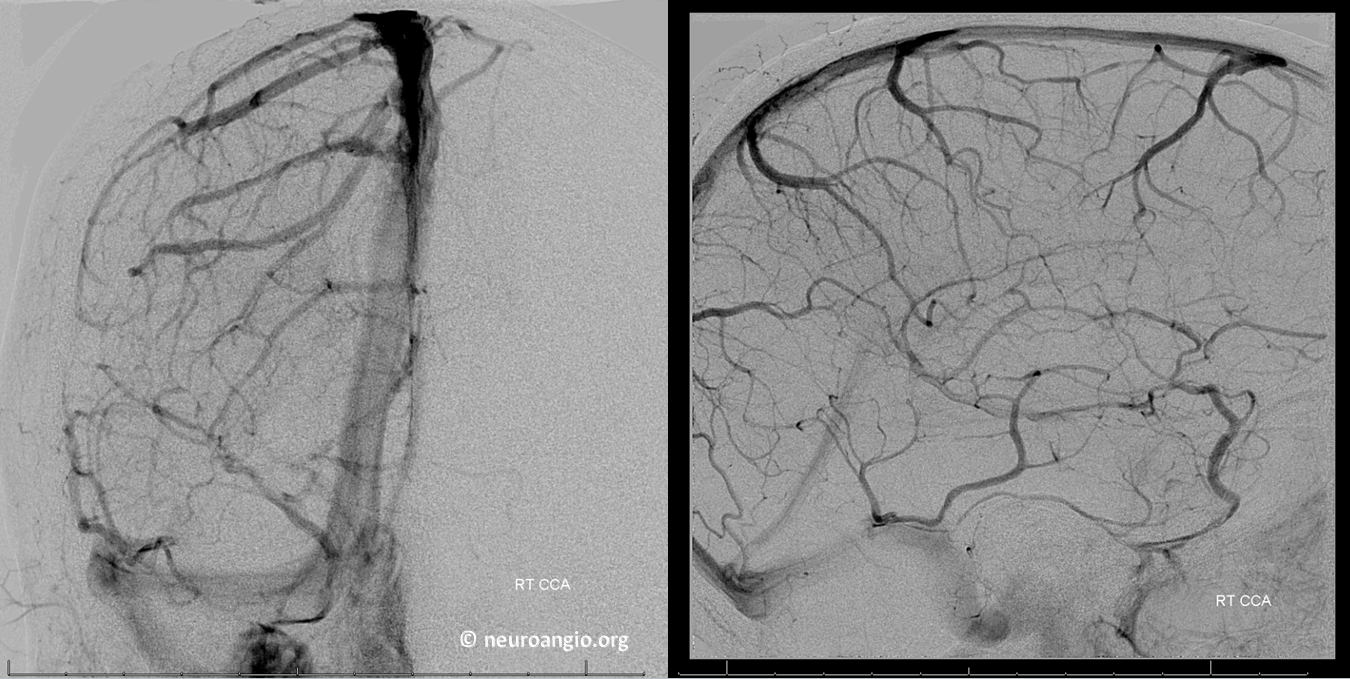
Oblique views. Stenosis is certainly not impressive
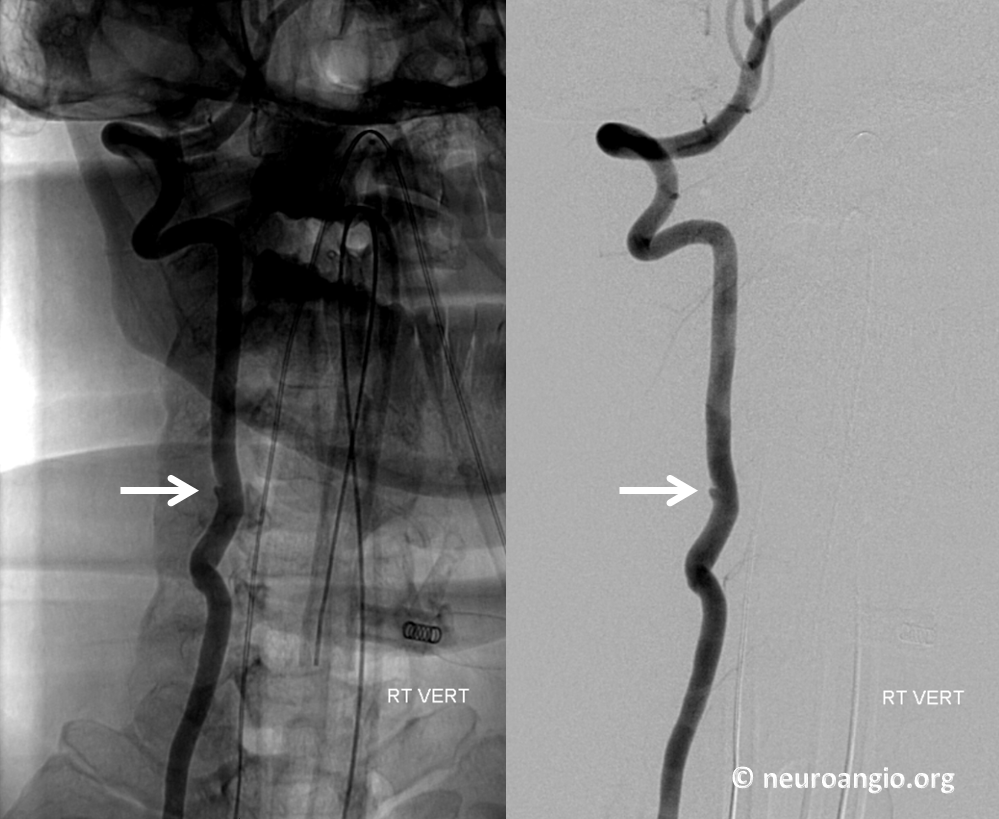
No issues with cervical jugular outflow

Vertebral view is also not impressive in terms of stenosis

However we did encounter an incidental remote mid-vert dissection. We promise we did not cause it. It is important to have faith in your convictions and not let yourself believe that this dissection is a cause of PT in this patient. It is tiny and very low. If you want to see vertebral artery dissection-related PT see case here.
So, pressure measurements showed a smooth 5 mm gradient between jugular bulb and transverse sinus. Not much of a gradient, but we have gone with this being sufficient in face of a clear severe stenosis before (case here)

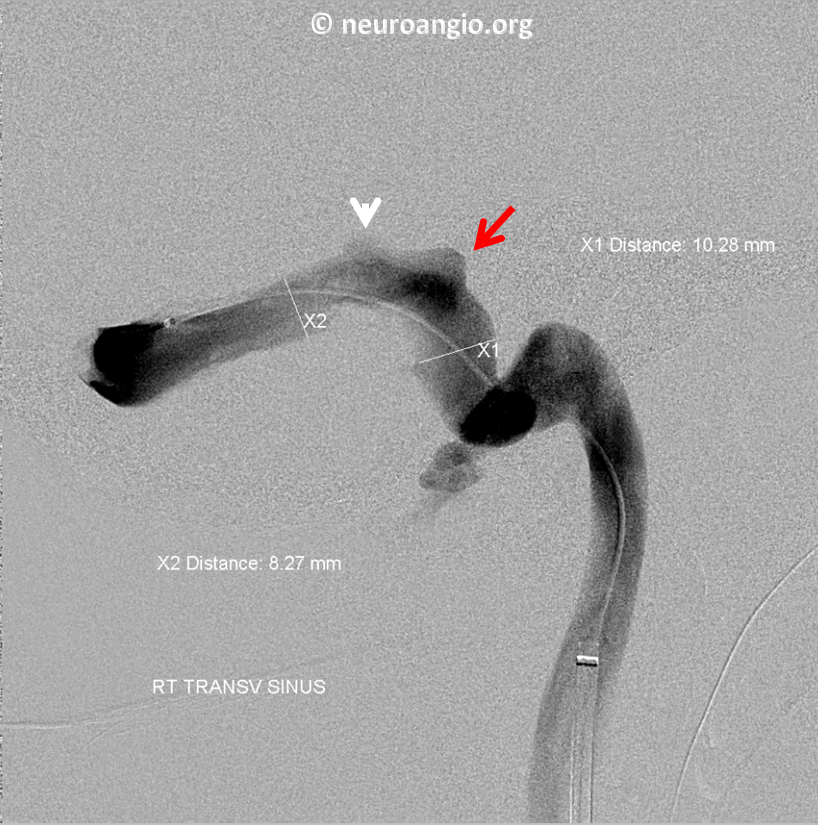
So far, we were not very impressed with the stenosis. Here is a venogram view, with diverticulum shown by red arrow and a smaller more proximal diverticulum by white arrowhead

To stent or not to stent? Another view to convince outselves
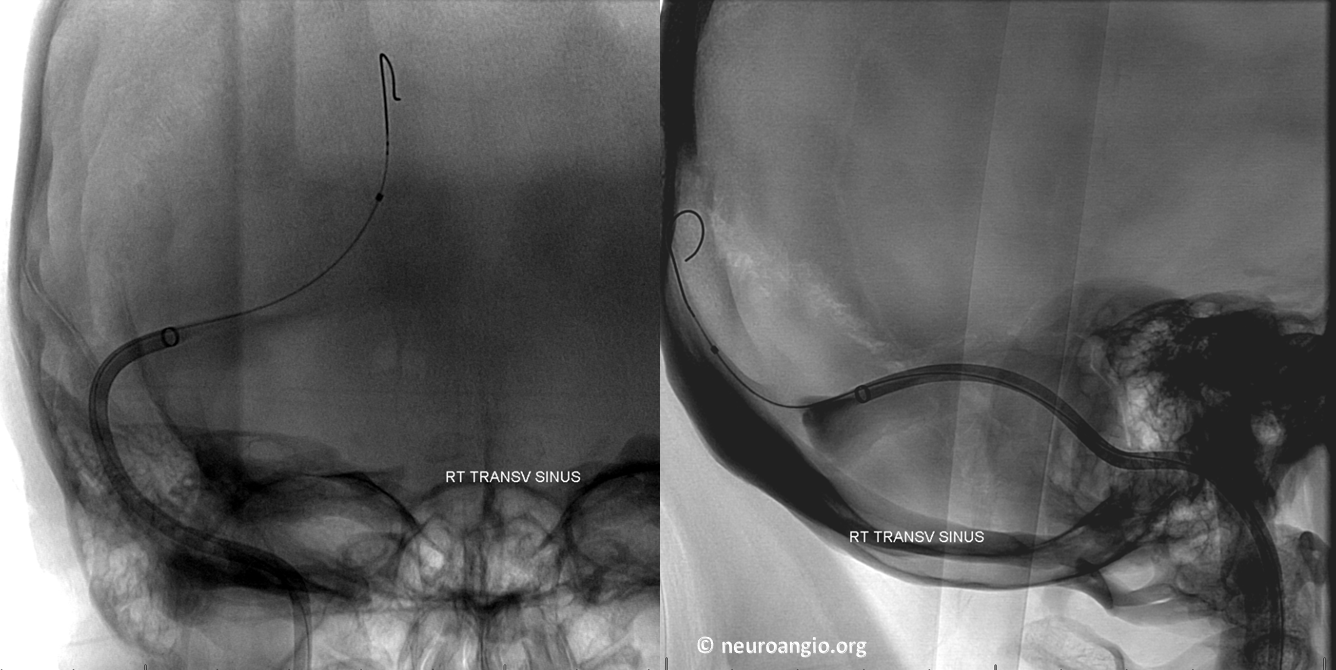
 In the end, we went ahead with stenting. NeuronMax in transverse sinus prior to stent placement. See additional cases on stent-related technique here and here
In the end, we went ahead with stenting. NeuronMax in transverse sinus prior to stent placement. See additional cases on stent-related technique here and here
Post stent
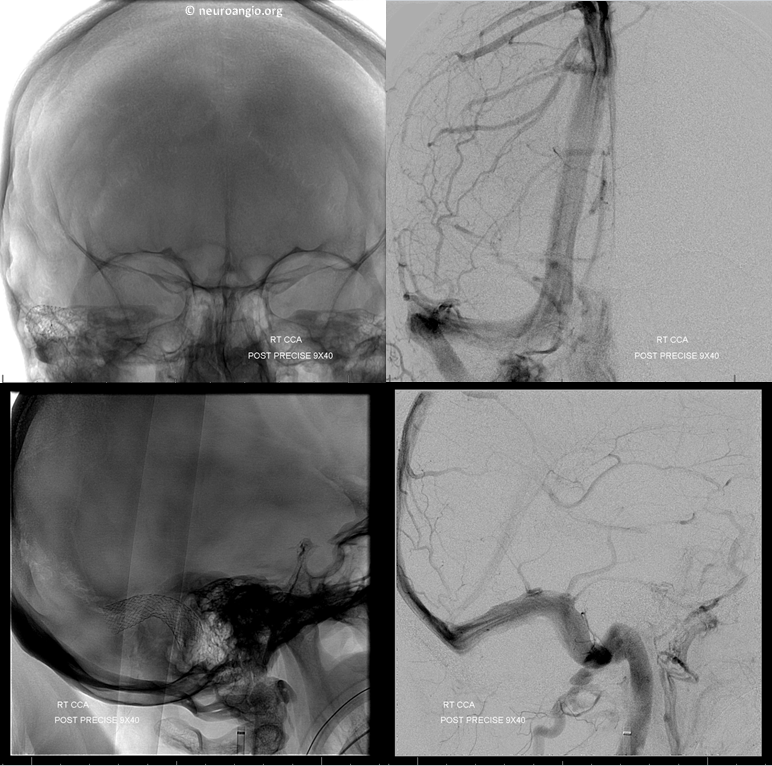
The patient woke up with no PT, and remains without it. In the end, our feeling is that the diverticulum is the culprit in this case.
