The most under-recognized cause of pulsatile tinnitus is venous sinus stenosis. It is a common and usually asymptomatic / incidental finding. However, that is not always the case. Some patients develop pulse-synchronous tinnitus due to turbulent flow across the area of stenosis. The stenosis is usually in the sigmoid sinus, and almost always “mirror image” bilateral. The sound is typically on the side of the bigger sinus. The hallmark of venous pulsatile tinnitus is the ability of patient to supress the sound by ipsilateral jugular compression. This simple and reproducible maneuver stops or markedly reduces flow in the entire transverse/sigmoid/jugular pathway. Even in patients with large emissary/subocipital/mastoid veins, jugular compression usually stops the sound completely. Thus combination of sigmoid sinus stenosis ipsilateral to the sound which can be temporarily abolished by jugular compression is virtually diagnostic of sinus stenosis as cause of pulsatile tinnitus.
The natural history of venous sinus stenosis is overwhelmingly benign. A well-recognized association between sinus stenosis and intracranial hypertension now exists. However, not all patients with venous sinus stenosis have intracranial hypertension and vice versa. For those with isolated sinus stenosis, the long-term prognosis appears favorable. Most patients with pulsatile tinnitus due to venous stenosis are able to tolerate the sound, especially once they learn that the cause is usually not “dangerous”. However, for a substantial minority the sound is loud, constant, disruptive and profoundly disturbing. In such cases, venous sinus stenting can be extremely effective as a durable cure.
Here is a real-life quite severe PT auscultated with a stethoscope on the OTHER side of the sound (sound on right, stethoscope on left mastoid bone). Cause is venous sinus stenosis. The sound is so loud on the right that it drowns out this sound on the left. This is how loud venous stenosis can get. Periods of relative silence correspond to times when the jugular vein is compressed. When compression is released, the sound comes back.
Here is the sound on the “bad” side in the same patient. Same idea — relative silence corresponds to times of jugular compression
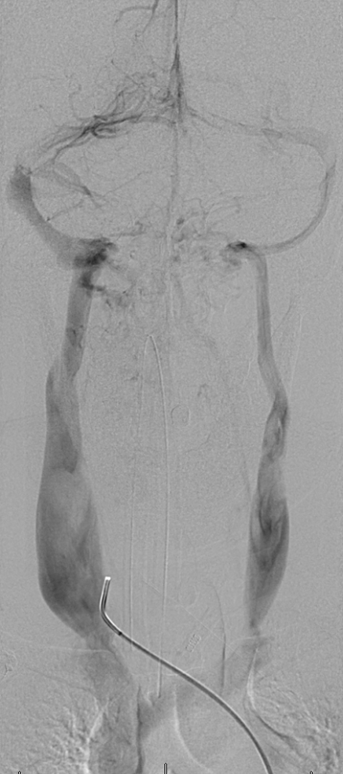
The patient below presents with a loud, constant, whoosh-like sound on the right side, which can be completely abolushed by right jugular compression. A faint bruit is heard over the mastoid bone. Some very loud venous sounds can be auscultated, particularly with a good stethoscope in a quiet room. Our typical workup is a noncontrast brain MRA, contrast brain MRI (which is as good as an MRV), and contrast neck MRA. This patient came in with an outside CTA. Fortunately, the CTA was bad with lots of venous contamination, which allowed for visualization of venous sinuses.
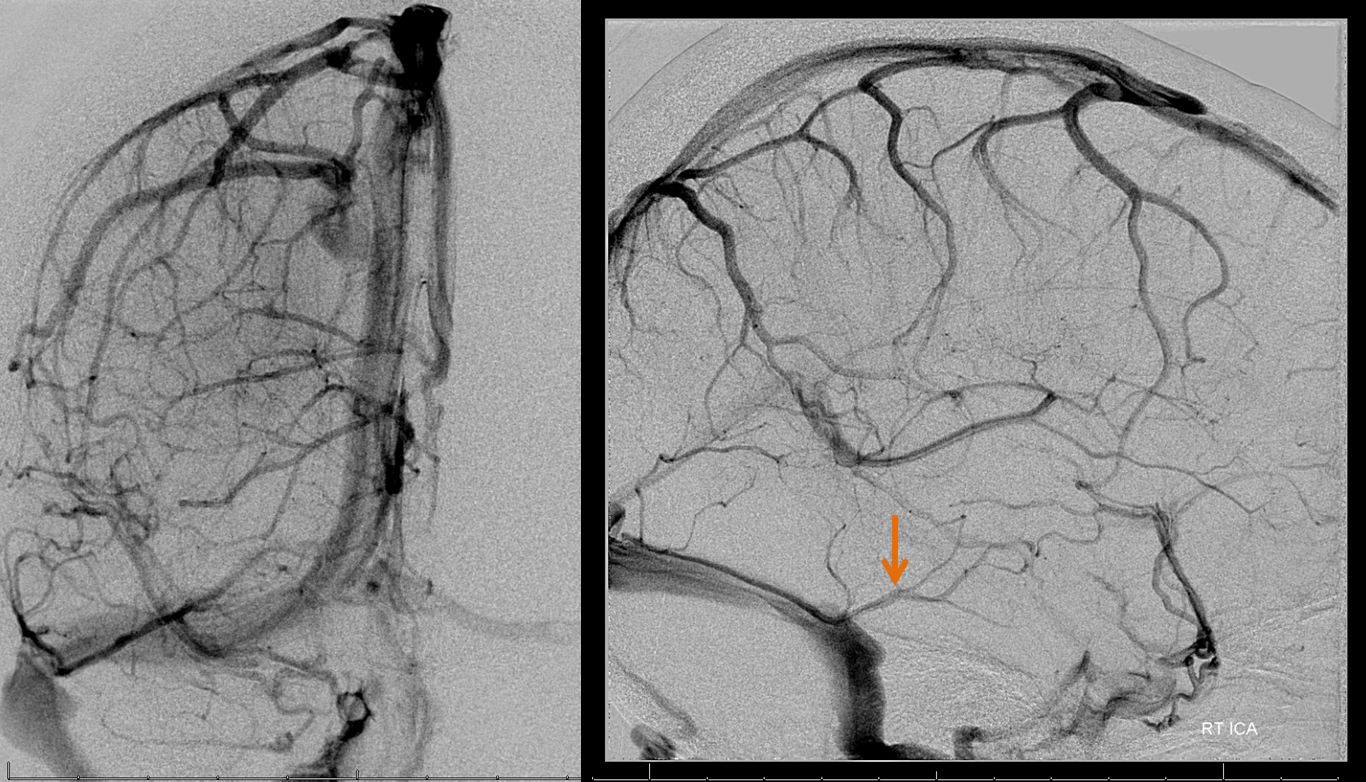
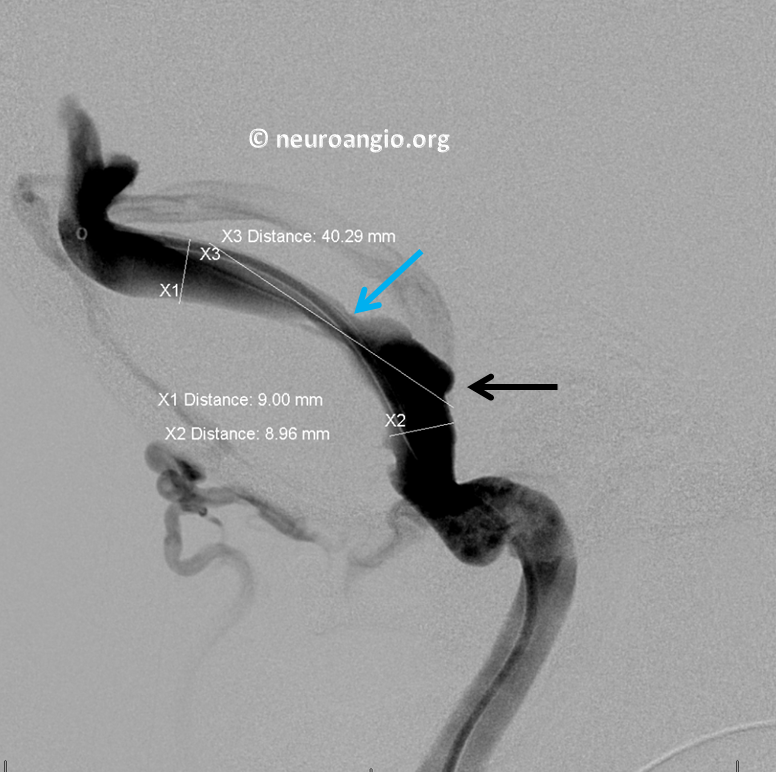
Right sided outflow is strongly dominant. Stenosis is shown by blue arrow. Notice a post-stenotic diverticulum (black arrow) with bony remodeling. Diverticulum is a frequent bystander in sinus stenosis. It is not the primary problem and only very rarely the cause of pulsatile tinnitus. Stenosis is.
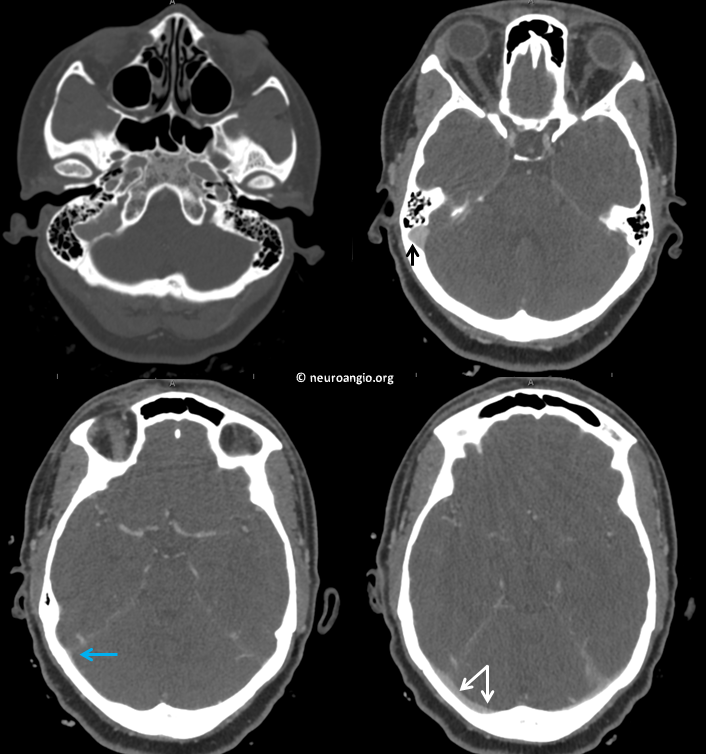
Coronal views are usually better to appreciate degree of stenosis. Same diverticulum (black)
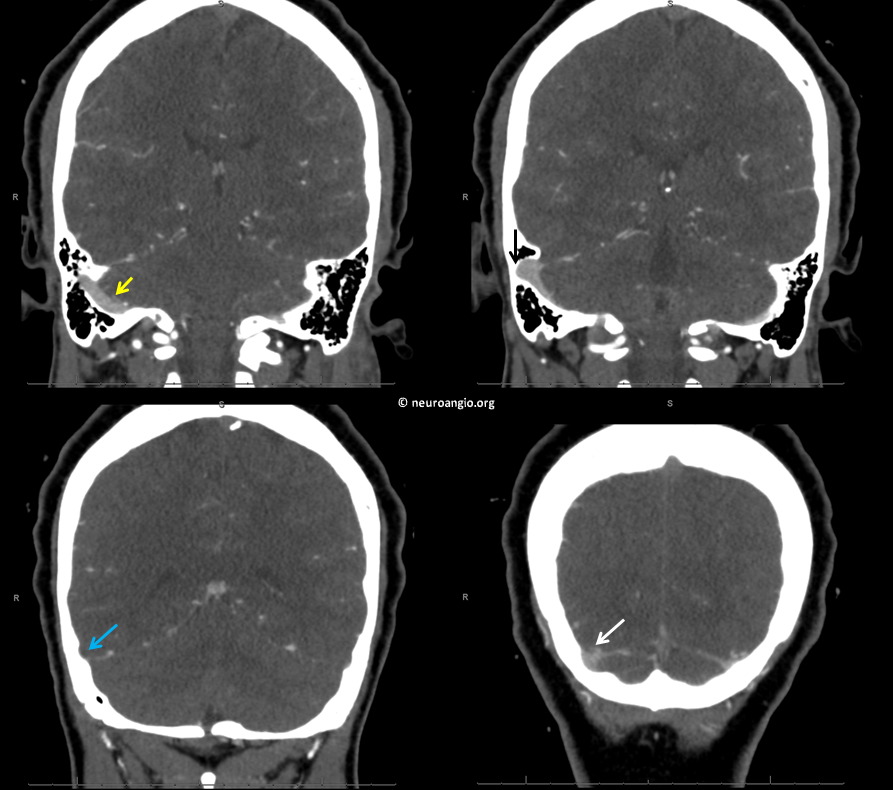
Angio. Typical flattened appearance of stenosis (blue arrow) with reduced contrast density in frontal view. Post-stenotic dilatation/deverticulum is black. Mirror image stenosis on the left (purple).
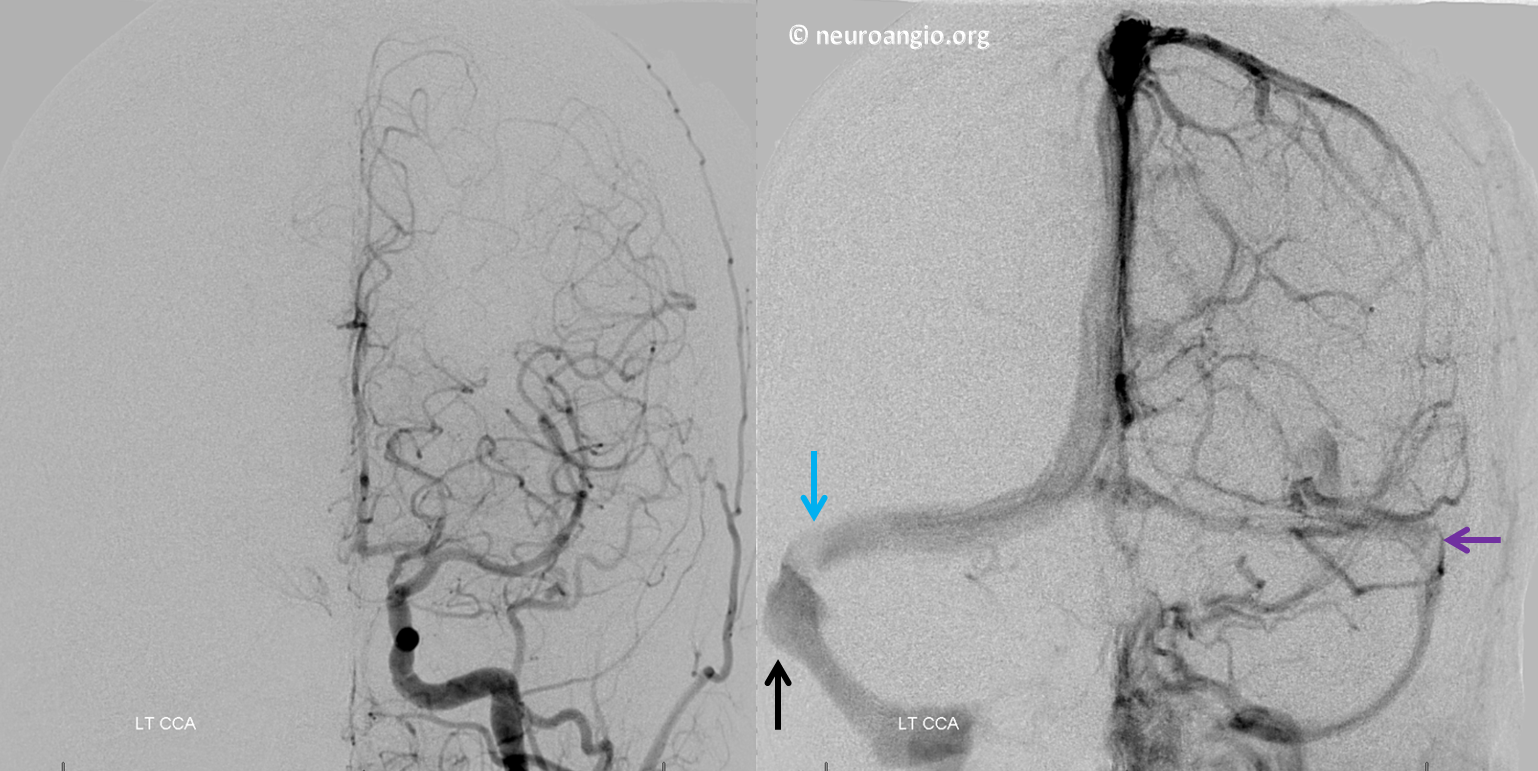
Vert injection venous phase.
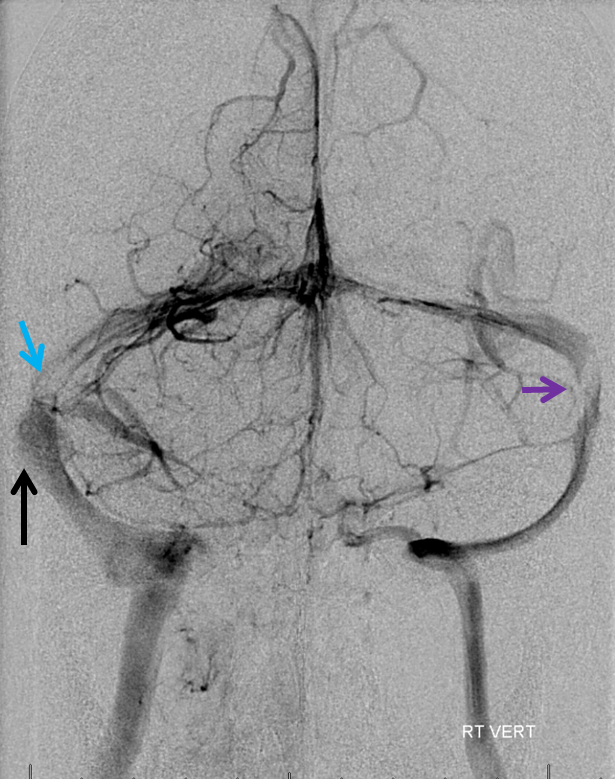
Vert injection cervical view to show otherwise normal jugular veins
Right ICA injection. It is important to examine tributary veins at level of stenosis. Usually the Labbe drains there. In this case, it is hypoplastic and can be safely covered with an uncovered stent
A full angiogram with external/common injections was done to show absence of dural fistula or other cause.
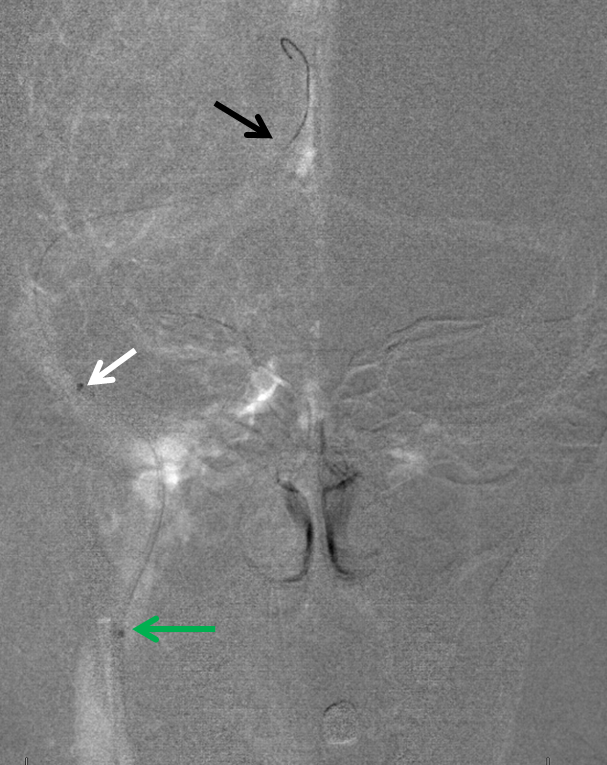
Now we move on to stenting. A NeuronMax 90 cm sheath (green arrow) is placed into the jugular. A 5F Sofia or another similar distal support catheter (white arrow) can be used to get high quality images of the sinus for morphology and measurements.
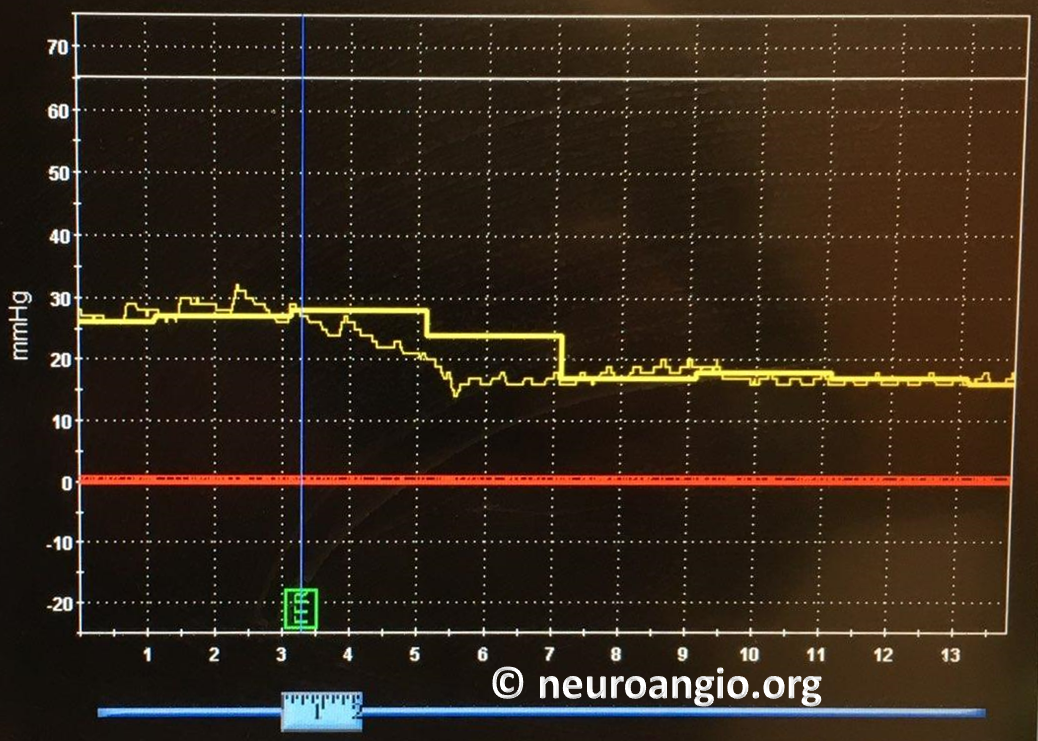
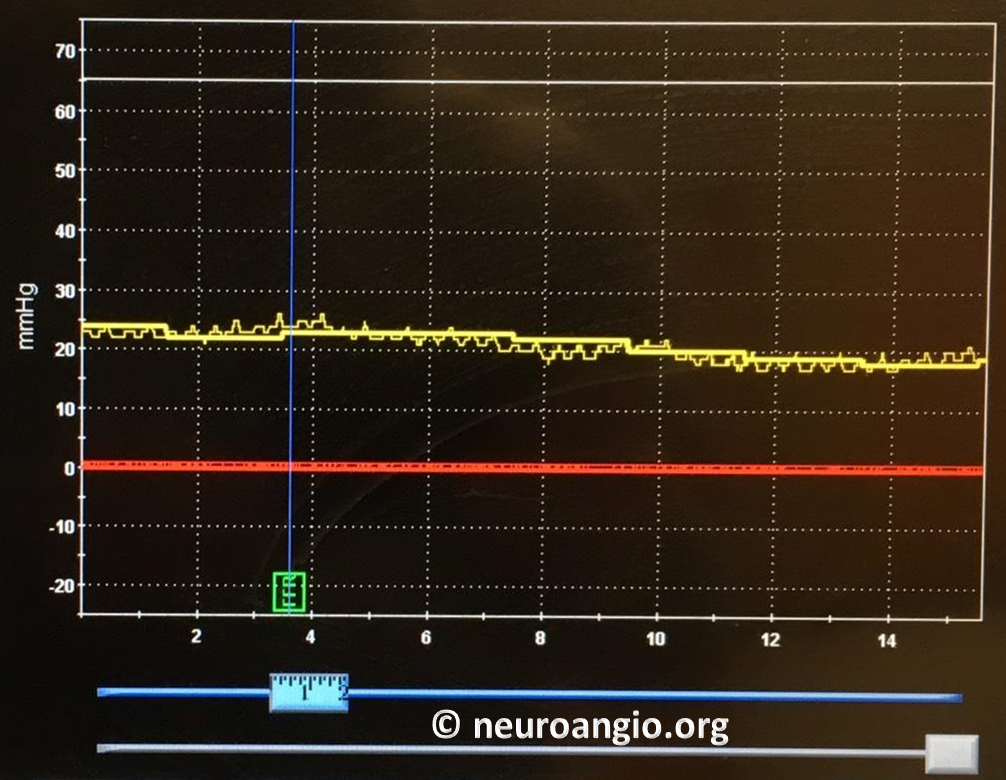
A Volcano 014 pressure wire (Pressure sensor at black arrow tip) is placed into the sinus system to perform pressure measurements. Existence of pressure gradient across the stenosis is a constant feature in venous pulsatile tinnitus. How much gradient exactly is necessary is not established. Usually, it is a focal drop over a short segment of more than 5 mm Hg.
Below is a pressure curve generated as the Volcano wire is withdrawn from the torcular to the jugular bulb. The acute pressure fall is over the area of sinus stenosis. The gradient is about 11 cm (28 cm Hg to 17 cm Hg)
Next, we get a good picture by injecting the Sofia. Measurements are made.

Lateral view. Notice how the post-stenotic dilatation/diverticulum is in line with the vector of sinus flow
Next, the Neuronmax (green) is advanced over the 5F Sofia into the distal sigmoid sinus. Most stents are relatively stiff and it is extremely helpful to advance the soft-tip neuronmax to where the stent will be deployed to facilitate atraumatic adjancement of the stent. Other ways of stent advancement (such as over a stiff 014 wire are possible also. We prefer this one
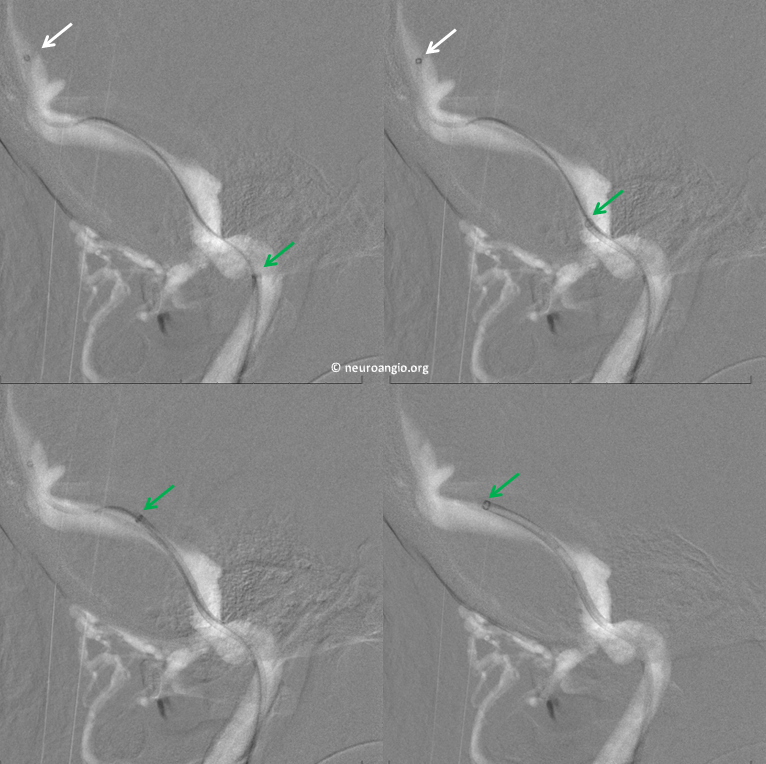
Now the stent (Precise 9×40) is advanced within the NeuronMax to the desired location
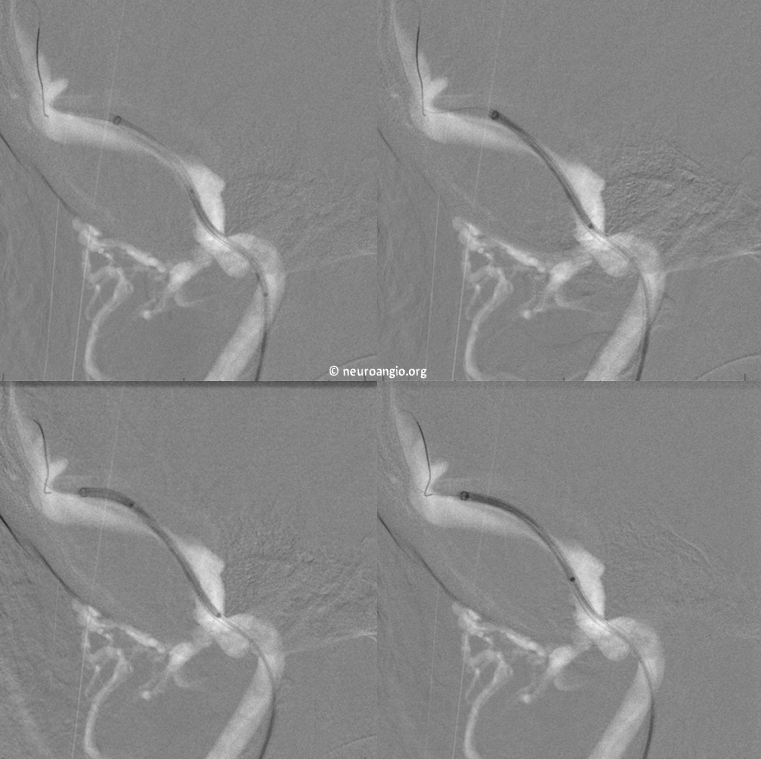
The Neuronmax is withdrawn back to the jugular bulb. The stent is a bit more distal at this point and will be pulled back prior to deployment

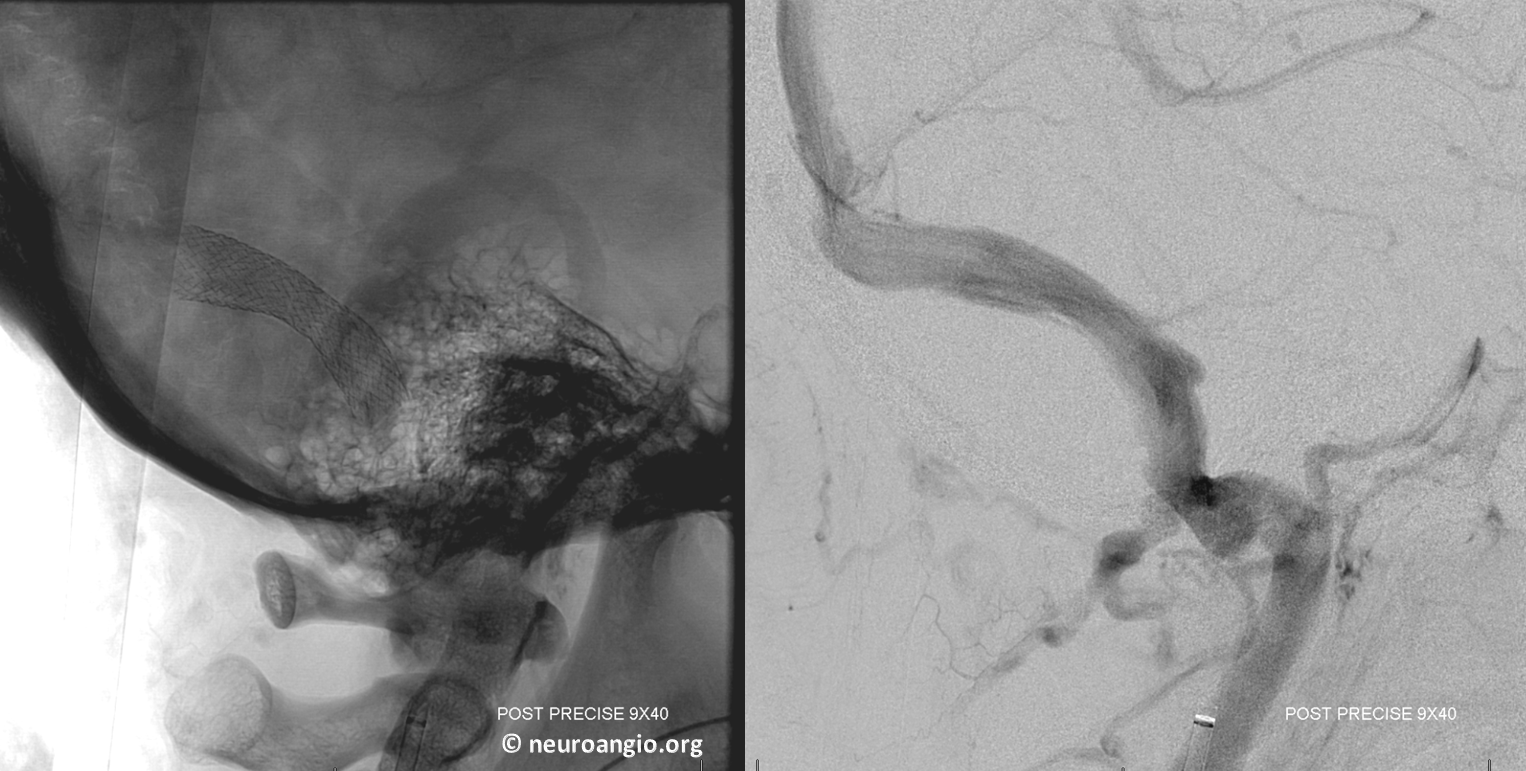
Deployment. The idea is to cover both stenosis and diverticulum, just in case
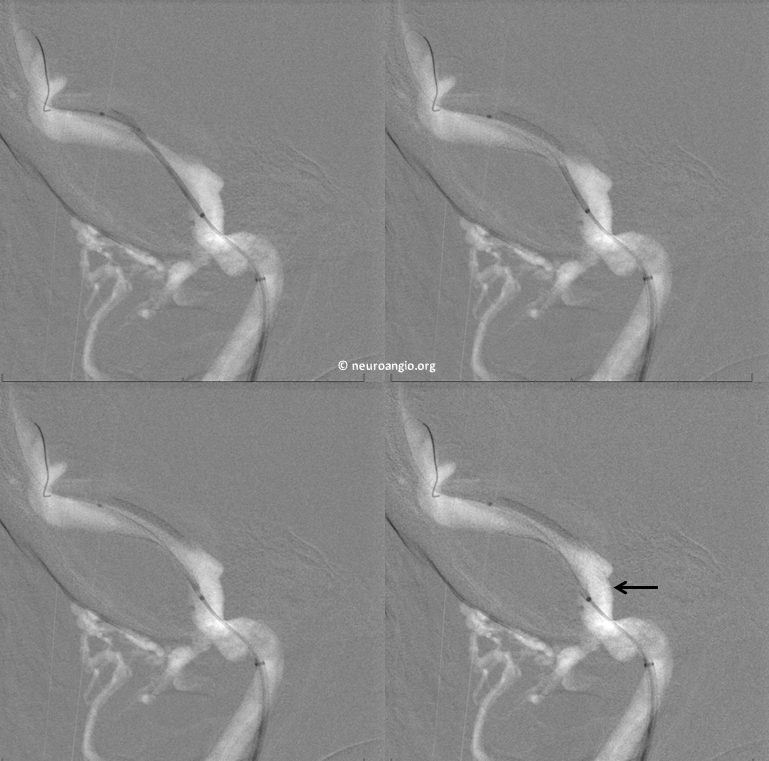
Post-deployment right common carotid angio. Good bye stenosis

Lateral views
Post-deployment pressure measurements. No more gradient
Pulsatile tinnitus is gone. In every case of venous sinus stenosis where the patient has been able to abolish the sound by jugular compression and no other cause was found, venous stenting resulted in immediate, complete, and permanent cure of pulsatile tinnitus.
Bibliography
Stéphanie Lenck, MD Marc-Antoine Labeyrie, MD Fabrice Vallee Jean-Pierre Saint-Maurice, MD Antoine Guillonnet, MD Anne-Laure Bernat, MD Pierre Vironneau, MD Emmanuel Houdart, MD. Stent Placement for Disabling Pulsatile Tinnitus Caused by a Lateral Sinus Stenosis: A Retrospective Study Operative Neurosurgery, Volume 13, Issue 5, 1 October 2017, Pages 560–565,
Francesco SignorelliKalid MahlaFrancis Turjman. Endovascular treatment of two concomitant causes of pulsatile tinnitus: sigmoid sinus stenosis and ipsilateral jugular bulb diverticulum. Case report and literature review. Acta Neurochirurgica. January 2012, Volume 154, Issue 1, pp 89–92
Baomin, Li; Yongbing, Shi; Xiangyu, Cao Angioplasty and Stenting for Intractable Pulsatile Tinnitus Caused by Dural Venous Sinus Stenosis: A Case Series Report. Otology & Neurotology: February 2014 – Volume 35 – Issue 2 – p 366–370
John M. Mathis, Douglas Mattox, Patrick Malloy, Gregg Zoarski. Endovascular Treatment of Pulsatile Tinnitus Caused by Dural Sinus Stenosis. Thieme Medical Publishers, Inc., 381 Park Avenue South, New York, NY 10016
